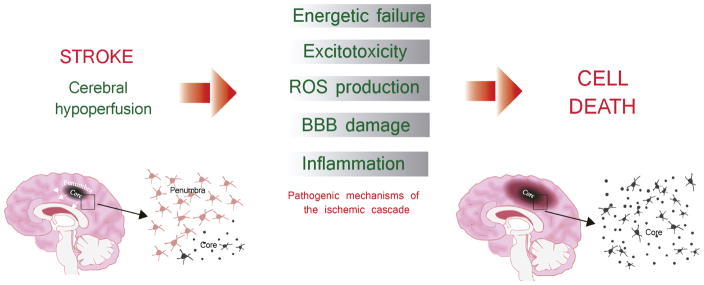
Fig. 1. The ischemic cascade.
Ischemic injury results from a series of cellular and molecular events caused by a sudden decrease or loss of blood flow and subsequent reperfusion of the ischemic territory. This succession of events is the so called ischemic cascade, consisting of a cellular bioenergetics failure, followed by excitotoxicity, oxidative stress, blood-brain barrier (BBB) dysfunction and post-ischemic inflammation, which collectively contribute to cell death in the ischemic. Within the first minutes, the lack of blood flow produces the energy failure in brain cells, triggering the release of the neurotransmitter glutamate. The postsynaptic overactivated NMDA (N-metil-D-aspartate) receptors will lead the excitotoxicity processes (mainly due to the influx of Ca2+) and then, the subsequent cellular damage due to the production of reactive oxygen species (ROS). Afterwards, the lack of blood flow and ROS will also damage the microvasculature producing the breakdown of the brain-blood-barrier (BBB), allowing the infiltration of leukocytes into the brain parenchyma. Resident brain cells (mainly microglial cells), but also astrocytes, together with infiltrated cells will release pro-inflammatory citokines triggering neuroinflammation, and therefore enhancing the brain damage. Two different regions can be distingued during the progression of the ischemic injury, that is, core and penumbra. The infarct core is the region in which the severe decrease of blood flow caused an energy failure and therefore cells rapidly die by necrosis. By contrary, the penumbra is the region which a preserved energy state. Without any intervention, the infarct core finally expands into the penumbra.