Abstract
Background
Regular physical activity (PA) induces desirable changes in plasma levels of high- and low-density lipoproteins (HDL and LDL, respectively) and triglycerides (TG), important risk factors for cardiometabolic diseases. However, doubts whether intensity and duration have equivalent benefits remain.
Objective
To assess the association of PA intensity and duration with HDL, LDL and TG levels.
Methods
Cross-sectional study with 12,688 participants from the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil) baseline, who were not on lipid-lowering medication. After adjustment for important covariates, multiple linear regression was used to assess the association of PA intensity and duration with HDL, LDL and TG (natural logarithm) levels.
Results
Both moderate and vigorous PA and PA practice ≥ 150 min/week were significantly associated with higher HDL and lower TG levels. Vigorous PA was associated with lower LDL only on univariate analysis. After adjustments, moderate and vigorous PA increased mean HDL level by 0.89 mg/dL and 1.71 mg/dL, respectively, and reduced TG geometric mean by 0.98 mg/dL and 0.93 mg/dL, respectively. PA practice ≥ 150 min/week increased mean HDL level by 1.05 mg/dL, and decreased TG geometric mean by 0.98 mg/dL.
Conclusion
Our findings reinforce the benefits of both PA parameters studied on HDL and TG levels, with a slight advantage for vigorous PA as compared to the recommendation based only on PA duration.
Keywords: Motor Activity, Cardiovascular Diseases, Health Profile, Hypercholesterolemia, Cholesterol, Triglycerides
Introduction
High plasma concentrations of low-density lipoproteins (LDL) and triglycerides (TG) and low high-density lipoprotein (HDL) levels are risk factors for cardiovascular disease (CVD).1 In addition to reducing the risk for CVD,2-7 an increase in HDL can halt the progression or even cause the regression of atherosclerotic plaques.8
Observational and experimental studies have shown that regular practice of physical activity (PA) induces desirable changes in plasma lipid levels,9 especially HDL increase and TG decrease, in addition to triggering beneficial effects on total cholesterol and its low-density and very-low-density fractions (LDL and VLDL, respectively).10,11 The effect of PA on HDL and TG levels seems to depend on neither weight nor diet changes.12 Physical activity is assumed to increase the activity of lipase lipoprotein and lecithin cholesterol acyltransferase and to reduce the activity of hepatic lipase and cholesterol esterified transfer protein, components of reverse cholesterol transport.13 Despite the well-known benefits resulting from PA practice, there are controversies about which PA characteristic would be more important to improve lipid profile: exercise intensity,14 frequency,15,16 duration17 or a combination of frequency and intensity.14 The reduction in TG levels was associated with higher PA intensity, but not with PA frequency.12
The World Health Organization (WHO) recommends, for adults aged 18-64 years, at least 150 min/week of moderate-intensity aerobic PA or 75 min/week of vigorous-intensity aerobic PA, or an equivalent combination of those, and aerobic activities should be performed in bouts of at least 10 minutes to yield benefits for cardiovascular health.18
Few studies in Brazil have estimated the contribution of different aspects of PA to HDL, LDL and TG concentrations. The present study was aimed at estimating the association of intensity and duration of leisure-time PA with the lipid profile of adult men and women participating in the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil) and not using any lipid-lowering medication. The major objective of the ELSA-Brasil was to investigate the biological, behavioral, environmental, occupational and psychosocial determinants of the incidence of CVD and diabetes.19,20
Methods
The ELSA-Brasil cohort included 15,105 active and retired individuals, aged 35 to 74 years, from teaching and research institutions in six Brazilian capitals. Because ELSA-Brasil is a multicenter study carried out in six states of three geopolitical regions of Brazil, it has an important diversity of phenotypes with information on a large number of sociodemographic, behavioral, clinical and laboratory factors that might influence lipid profile.
The present study has a cross-sectional design and uses data from the baseline of ELSA-Brasil, carried out from 2008 to 2010. In the investigation centers, data were collected by certified interviewers and checkers, meeting the criteria recommended by a Quality Control Committee,21 allowing the necessary standardization.
The eligibility criterion of the present study was as follows: individuals aged 35 to 69 years, undergoing laboratory tests to measure HDL, LDL and TG levels, and who answered the International Physical Activity Questionnaire (IPAQ) on leisure-time PA.
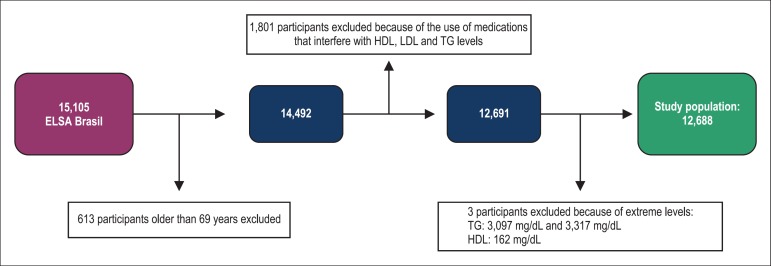
Because IPAQ was validated only for adults up to the age of 69 years, 613 participants (4.06%) aged 70 to 74 years were excluded.22 In addition, 1,801 participants (11.92%) were ineligible because they were on medications that could influence HDL, LDL and TG levels: atorvastatin calcium; bezafibrate; ciprofibrate; ezetimibe; fenofibrate; fluvastatin sodium; gemfibrozil; lovastatin; nicotinamide; orlistat; pravastatin sodium; simvastatin; rosuvastatin calcium; nicotinic acid; conjugated estrogens and estrone sulfate. Three individuals (0.02%) had extreme TG and HDL levels and were excluded from the analysis. The final sample comprised 12,688 individuals (Figure 1).
Figure 1.
Study population selection. HDL: high-density lipoprotein; LDL: low-density lipoprotein; TG: triglycerides.
All laboratory parameters were measured in blood samples collected in the local investigation centers, after a mean 12-hour fasting period (minimum of 10 hours, and maximum of 14 hours). The samples were sent to the central laboratory of ELSA-Brasil in São Paulo for analysis, via a transport service specialized in frozen biological material, and processed using ADVIA 1200 automated analyzer (Siemens Healthcare Diagnostics, USA). Triglyceride levels were measured by using the colorimetric method containing glycerophosphate and peroxidase. LDL levels were estimated by using Friedewald formula, and, when TG levels were higher than 400 mg/dL, homogeneous enzymatic colorimetric assay without precipitation was used. HDL levels were measured using homogeneous enzymatic colorimetric assay without precipitation.23
The results of HDL, LDL and TG measurements were assessed in continuous and categorical ways. The categorical analysis was obtained from cutoff points for the desirable minimum HDL levels, ≥ 40 mg/dL for men and ≥ 50 mg/dL for women. For LDL and TG levels, the cutoff points considered were below 160 mg/dL and 150 mg/dL, respectively.24
Information regarding leisure-time PA practice were obtained via the long version of IPAQ for leisure-time PA, containing questions related to PA frequency, duration and intensity.25,26
Physical activity was categorized as follows: 1) insufficient - no PA practice OR some PA, but not meeting the other two categories; 2) moderate - 3 or more days of vigorous-intensity PA for at least 20 min/day, OR 5 or more days of moderate-intensity PA and/or walking, in combination or alone, at least 30 min/day, OR 5 or more days of any combination of walking, moderate-or-vigorous-intensity PA achieving a minimum of 600 MET-min/week; and 3) vigorous - vigorous-intensity PA on at least 3 days, accumulating a minimum of 1500 MET-min/week, or 7 or more days of any combination of walking, moderate-or-vigorous-intensity PA accumulating a minimum of 3000 MET-min/week.26
In addition, PA was assessed by using both the total reported PA duration in min/week, represented by the sum of the time spent with insufficient-, moderate- and vigorous-intensity PA, and the categorization into little active or active, based on the WHO recommendation of moderate PA for at least 150 min/week, or vigorous PA for at least 75 min/week.18
Sociodemographic characteristics included: sex; age (years); schooling (incomplete elementary, complete elementary, middle- or high-school level); per capita income obtained by dividing the mean point of each of the 10 bands of family net income per month by the number of people depending on that income (quintile); and self-reported race/skin color (black, mixed, white, yellow/native). Individuals self-reporting yellow skin color (2%) and native (1%) were grouped into a single category due to their small number.
Anthropometric indicators were body mass index (BMI), obtained by dividing body weight (kg) by square height (m2), and waist/hip ratio (WHR), resulting from dividing waist circumference (cm) by hip circumference (cm). Body weight and standing height were measured according to consolidated technical standards and criteria.21
The validated food-frequency questionnaire provided data of participants' food intake.27 Regarding fruits and vegetables, regular intake was defined as their usual ingestion at least five days per week, and low intake, as their usual ingestion four or less days per week. The intake of fat and carbohydrates was assessed by their daily consumption in grams.
The category "smoker" referred to having ever smoked at least 100 cigarettes during life and currently smoking, and "ex-smoker"/non-smoker referred to not currently smoking. The use of alcoholic beverages was categorized as follows: never used alcohol; ex-user; moderate user; and abuser. Alcohol abuse was defined as weekly alcohol consumption greater than 140 g and 210 g for women and men, respectively.
Statistical analysis
The normality of distribution of each continuous variable was assessed by using Shapiro Wilk test. Variables with normal distribution were described as mean ± standard deviation, and the others, as median and interquartile intervals. The distribution of categorical variables was compared by using chi-square test, and that of continuous variables, by using Mann-Whitney test for those whose distribution was not normal. Because TG levels do not have normal distribution, they were transformed into natural logarithm (ln) in the regression model, with exponentiation of the coefficients of explanatory variables to indicate values of multiplicative changes in the geometric mean of TG levels.
The independent association of PA practice with HDL, LDL and TG (ln) concentrations was estimated by using multiple linear regression after adjusting for sex and age and the other confounding variables that remained associated with response variables to the level of p < 0.05 in the final model.
Raw and adjusted coefficients of determination (R2) were used to estimate the contribution of PA and other explanatory variables to the distribution of the response variables in the final model of HDL, LDL and TG. The specific percentage contribution of each different PA indicator to response-variable variability in the final model was estimated by comparing adjusted coefficients of determination before and after inclusion of the PA intensity or duration variable in the model.
The analyses were performed by using Stata statistical software, 12.0 version.
Results
Most of the 12,688 participants included in the study were of the female sex and had white skin color and high-school level. Mean age was 50 years, mean BMI was 26.8 kg/m2, 15.3% smoked, and most of the participants were moderate alcohol users (Table 1).
Table 1.
Sociodemographic, behavioral and anthropometric characteristics and lipid profile of ELSA-Brasil participants aged 35 to 69 years, according to sex (2008-2010)
| Variables | Male n = 5,731 | Female n = 6,957 | Total n = 12,688 |
|---|---|---|---|
| Sociodemographic characteristics | |||
| Sex (%) | 45.2 | 54.8 | |
| Age in years | 50.4 (± 8.2) | 50.5 (± 8.1) | 50.5 (± 8.1) |
| Skin color/race (%) | |||
| White | 50.5 | 50.5 | 50.5 |
| Mixed | 31.8 | 27.6 | 29.5 |
| Black | 14.6 | 18.2 | 16.6 |
| Yellow/ Native | 3.1 | 3.6 | 3.4 |
| Schooling (%) | |||
| High school | 48.2 | 54.6 | 51.7 |
| Middle school | 35.5 | 36.7 | 36.1 |
| Complete elementary | 8.4 | 5.2 | 6.6 |
| Incomplete elementary | 7.9 | 3.6 | 5.6 |
| Behaviors | |||
| Smoking (%) | |||
| Never smoked/ Ex-smoker | 84.7 | 87.4 | 86.2 |
| Smoker | 15.3 | 12.6 | 13.8 |
| Alcohol consumption (%) | |||
| Never | 4.5 | 15.5 | 10.5 |
| Ex-user | 19.9 | 20.1 | 20.0 |
| Moderate user | 63.1 | 60.9 | 61.9 |
| Abuser | 12.5 | 3.6 | 7.6 |
| Fruit and vegetable consumption (%) | |||
| ≤ 4x/week | 61.8 | 44.4 | 52.3 |
| ≥ 5x/week | 38.2 | 55.6 | 47.7 |
| Saturated fat intake (g)† | 32.2 (23.7; 44.2) | 27.4 (20.1; 36.6) | 29.4 (21.5; 40.1) |
| Carbohydrate intake (g)† | 354.6 (273.3; 468.4) | 289.3 (224.6; 377.6) | 316.3 (242.3; 416.9) |
| Leisure-time physical activity | |||
| Physical activity recommended by WHO* (%) | |||
| < 150 min/week | 57.7 | 68.4 | 63.6 |
| ≥ 150 min/week | 42.3 | 31.6 | 36.4 |
| Physical activity intensity†(%) | |||
| Insufficient | 74.7 | 81.0 | 78.1 |
| Moderate | 14.0 | 12.0 | 12.8 |
| Vigorous | 11.3 | 7.0 | 9.1 |
| Total physical activity duration (min/week) (median, Q1 and Q3) | 80.0 (0; 240.0) | 0 (0; 180.0) | 60.0 (0; 190.0) |
| Anthropometrics | |||
| Body mass index (kg/m2)* | 26.8 (± 4.3) | 26.9 (± 5.1) | 26.8 (± 4.8) |
| Waist-hip ratio* | 0.94 (± 0.07) | 0.84 (± 0.07) | 0.89 (± 0.09) |
| Lipids | |||
| HDL (mg/dL)* | 50.9 (± 12.2) | 61.8 (± 14.5) | 56.9 (± 14.6) |
| LDL (mg/dL)* | 133.9 (± 35.3) | 133.0 (± 34.4) | 133.4 (± 34.8) |
| Triglycerides (mg/dL)† | 131.0 (92.0; 192.0) | 100.0 (73.0; 140.0) | 112.0 (80.0; 163.0) |
Q1 and Q3: interquartile interval; WHO: World Health Organization; (*) Duration recommended by WHO; (†) Intensity defined based on long IPAQ. HDL: high-density lipoprotein; LDL: low-density lipoprotein; (*) Mean (standard deviation); (†) Median (interquartile intervals).
Regarding weekly leisure-time PA practice, almost 80% of the individuals had it insufficient, less than 10% had it vigorous, and PA distribution was similar in both sexes. Of the participants, 64% did not report PA practice according to WHO recommendations, and the median total PA duration was 60 minutes per week for the total population (Table 1).
Regarding lipid profile, HDL and LDL values ranged from 20 to 148 mg/dL and 32 to 515 mg/dL for men, and from 18 to 146 mg/dL and 33 to 411 mg/dL for women, respectively. TG values ranged from 26 to 2,070 (mg/dL) for men and from 26 to 1,438 100 mg/dL for women (Table 1).
Less than half of the men and slightly more than half of the women met the recommendations for HDL levels, and similar prevalences were observed for desirable levels according to sex. Altered TG was observed in 3/5 of men and 2/5 of women (Table 2). Sex, age, skin color, per capita income (quintile), schooling, smoking habit, alcohol use, BMI and WHR were statistically associated with recommended HDL and TG levels. On the other hand, desirable LDL levels were statistically associated with age, schooling, smoking habit, BMI and WHR (Table 2). Recommended HDL and TG levels were statistically associated with PA intensity, total PA duration and recommended PA duration of at least 150 min/week. Desirable LDL levels were statistically associated with only total PA duration (Table 3).
Table 2.
Distribution of study participants according to sociodemographic, behavioral and anthropometric characteristics, and according to desirable levels of HDL and LDL and triglycerides (n = 12,688)
| Variables | desirable HDL | altered HDL | p-value | desirable LDL | altered LDL | p-value | desirable TG | altered TG | p-value |
|---|---|---|---|---|---|---|---|---|---|
| Sex (%) | < 0.001* | 0.655* | < 0.001* | ||||||
| Male | 46.8 | 37.3 | 45.1 | 45.6 | 38.3 | 61.0 | |||
| Female | 53.2 | 62.7 | 54.9 | 54.4 | 61.7 | 39.0 | |||
| Age (years) (%) | < 0.001* | < 0.001* | < 0.001* | ||||||
| 35 - 44 | 24.6 | 30.5 | 28.0 | 16.2 | 27.7 | 20.6 | |||
| 45 - 54 | 42.4 | 42.7 | 42.2 | 43.7 | 42.1 | 43.3 | |||
| 55 - 64 | 27.5 | 22.1 | 24.6 | 33.8 | 24.9 | 30.3 | |||
| 65 - 69 | 5.6 | 4.8 | 5.2 | 6.3 | 5.3 | 5.8 | |||
| Skin color/race (%) | 0.041* | 0.440* | < 0.001* | ||||||
| White | 50.9 | 49.0 | 50.5 | 50.6 | 50.6 | 50.4 | |||
| Mixed | 29.0 | 32.0 | 29.3 | 30.2 | 28.6 | 31.6 | |||
| Black | 6.8 | 15.7 | 16.7 | 16.3 | 17.5 | 14.4 | |||
| Yellow/Native | 3.4 | 3.3 | 3.5 | 2.9 | 3.3 | 3.6 | |||
| Schooling (%) | < 0.001* | 0.017* | < 0.001* | ||||||
| High school | 52.9 | 45.9 | 51.5 | 52.3 | 54.2 | 45.7 | |||
| Middle school | 35.1 | 41.1 | 36.6 | 34.2 | 34.9 | 39.0 | |||
| Complete elementary | 6.5 | 7.5 | 6.6 | 6.9 | 6.1 | 8.0 | |||
| Incomplete elementary | 5.5 | 5.5 | 5.3 | 6.6 | 4.8 | 7.3 | |||
| Per capita income (%) | < 0.001* | 0.089* | < 0.001* | ||||||
| 1st quintile (higher) | 21.1 | 14.2 | 19.5 | 21.3 | 21.1 | 16.9 | |||
| 2nd quintile | 18.7 | 16.6 | 18.2 | 18.7 | 18.6 | 17.7 | |||
| 3rd quintile | 19.4 | 18.9 | 19.2 | 19.7 | 19.4 | 19.2 | |||
| 4th quintile | 21.2 | 24.2 | 22.0 | 20.8 | 21.5 | 22.3 | |||
| 5th quintile (lower) | 19.6 | 26.0 | 21.1 | 19.5 | 19.4 | 23.9 | |||
| Smoking (%) | < 0.001* | 0.003* | < 0.001* | ||||||
| Never smoked/ Ex-smoker | 86.8 | 83.7 | 86.7 | 84.4 | 87.8 | 82.6 | |||
| Smoker | 13.2 | 16.3 | 13.3 | 15.6 | 12.2 | 17.4 | |||
| Alcohol consumption (%) | < 0.001* | 0.783* | < 0.001* | ||||||
| Never | 9.6 | 14.3 | 10.6 | 9.9 | 11.1 | 9.0 | |||
| Ex-user | 18.7 | 26.2 | 20.0 | 20.0 | 20.2 | 19.6 | |||
| Moderate user | 63.4 | 54.9 | 61.8 | 62.2 | 63.1 | 59.2 | |||
| Abuser | 8.3 | 4.6 | 7.6 | 7.8 | 5.7 | 12.2 | |||
| Fruit and vegetable consumption (%) | 0.783* | 0.974* | < 0.001* | ||||||
| ≤ 4x/week | 52.3 | 52.5 | 52.3 | 52.3 | 50.3 | 56.8 | |||
| ≥ 5x/week | 47.8 | 47.5 | 47.7 | 47.7 | 49.7 | 43.2 | |||
| BMI (kg/m2) (%) | < 0.001* | < 0.001* | < 0.001* | ||||||
| Slimness | 1.2 | 0.3 | 1.2 | 0.2 | 1.4 | 0.2 | |||
| Eutrophy | 40.6 | 24.4 | 39.3 | 31.7 | 44.4 | 22.2 | |||
| Overweight | 38.6 | 42.7 | 38.1 | 44.1 | 36.5 | 45.9 | |||
| Obesity | 19.6 | 32.6 | 21.4 | 24.0 | 17.7 | 31.7 | |||
| WHR (%) | < 0.001* | < 0.001* | < 0.001* | ||||||
| M ≤ 0,9; W ≤ 0,85 | 44.7 | 28.6 | 44.1 | 33.4 | 51.8 | 18.8 | |||
| M > 0,9; W > 0,85 | 55.3 | 71.4 | 55.9 | 66.7 | 48.2 | 81.3 |
HDL: high-density lipoprotein; desirable HDL - ≥ 40 mg/dL for men, and ≥ 50 mg/dL for women; LDL: low-density lipoprotein; desirable LDL - <160 mg/dL; TG: triglycerides; desirable TG - < 150 mg/dL; BMI: body mass index; WHR: waist-hip ratio; M: men; W: women; p < 0.001 - statistical significance;
chi-square test.
Table 3.
Prevalence of desirable levels of HLD, LDL and triglycerides according to indicators of physical activity intensity and duration of ELSA-Brasil participants aged 35 to 69 years, 2008-2010, n = 12,688
| Variables | desirable HDL | altered HDL | p-value | desirable LDL | altered LDL | p-value | desirable TG | altered TG | p-value |
|---|---|---|---|---|---|---|---|---|---|
| PA (WHO) (%) | < 0.001* | 0.391* | < 0.001* | ||||||
| < 150 min/week | 61.8 | 71.8 | 63.8 | 62.9 | 62.2 | 66.9 | |||
| ≥ 150 min/week | 38.2 | 28.2 | 36.2 | 37.1 | 37.9 | 33.1 | |||
| PA intensity (%) | < 0.001* | 0.046* | < 0.001* | ||||||
| Insufficient | 76.9 | 83.7 | 78.3 | 77.7 | 76.6 | 81.7 | |||
| Moderate | 13.3 | 10.7 | 12.5 | 14.1 | 13.5 | 11.3 | |||
| Vigorous | 9.8 | 5.7 | 9.3 | 8.6 | 9.9 | 7.1 | |||
| Total PA duration (min/week)‡ | 60.0 | 0.0 | < 0.001† | 60.0 | 0.0 | < 0.001† | 60.0 | 30.0 | < 0.001† |
HDL: high-density lipoprotein; desirable HDL - ≥ 40 mg/dL for men and ≥ 50 mg/dL for women; LDL: low-density lipoprotein; desirable LDL - ≤160 mg/dL; TG: triglycerides; desirable TG - ≤ 150mg/dL; p < 0.001 - statistical significance; WHO: World Health Organization; PA: physical activity;
chi-square test;
Wilcoxon test (Mann-Whitney);
Median.
Table 4 shows the results of simple linear regression analysis. Moderate- and vigorous-intensity PA was associated with an increase in HDL, with suggestion of dose-response gradient. Both longer total PA duration and PA practice for at least 150 min/week or more were associated with HDL elevation. All associations maintained after adjustment for sex and age, and later for the other confounding variables including race/skin color, per capita income, schooling, WHR, BMI, alcohol consumption, current smoking and total carbohydrate and saturated fat intake (Table 4). The regular consumption of fruits and vegetables was not statistically associated with HDL levels on multivariate regression analysis.
Table 4.
Association of different indicators of leisure-time physical activity with HDL, LDL and triglyceride levels on simple linear and multiple regression analyses of ELSA-Brasil participants (n = 12,688)
| Univariate | Adjustment for sex and age‡ | Adjustment for all confounding factors§ | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Variables | β | [95%CI] | R2 | B | [95%CI] | Adj R2 | β | [95%CI] | Adj R2 |
| HDL | |||||||||
| PA intensity | 0.003 | 0.152 | 0.266 | ||||||
| Moderate | 1.592 | (0.822; 2.361)* | 2.087 | (1.376; 2.799)* | 0.893 | (0.219; 1.566)† | |||
| Vigorous | 2.265 | (1.368; 3.162)* | 3.927 | (3.097; 4.758)* | 1.710 | (0.918; 2.501)* | |||
| PA (WHO) | 0.003 | 0.153 | |||||||
| ≥ 150 min/week | 1.522 | (0.996; 2.048)* | 2.772 | (2.284; 3.260)* | 1.055 | (0.582; 1.527)* | 0.266 | ||
| Total PA duration (min/week) | 0.004 | (0.003; 0.005)* | 0.002 | 0.007 | (0.006; 0.008)* | 0.153 | 0.003 | (0.002; 0.005)* | 0.267 |
| TG (ln) | |||||||||
| PA intensity | 0.006 | 0.093 | 0.230 | ||||||
| Moderate | -0.044 | (-0.072; -0.016)* | -0.073 | (-0.097; -0.046)* | -0.020 | (-0.045; 0.005) | |||
| Vigorous | -0.136 | (-0.168; -0.103)* | -0.163 | (-0.195; -0.132)* | -0.068 | (-0.097; -0.039)* | |||
| PA (WHO) | 0.091 | 0.229 | |||||||
| ≥ 150 min/week | -0.058 | (-0.077; -0.038)* | 0.003 | -0.093 | (-0.111; -0.074)* | -0.022 | (-0.040; -0.005)† | ||
| Total PA duration (min/week) | 0.000 | (0.000; 0.000)* | 0.003 | 0.000 | (0.000; 0.000)* | 0.092 | 0.000 | (0.000; 0.000)* | 0.230 |
| LDL | |||||||||
| PA intensity | 0.001 | 0.025 | |||||||
| Moderate | 1.564 | (-0.279; 3.407) | 0.609 | (-1.215; 2.433) | |||||
| Vigorous | -2.282 | (-4.430; -0.134)† | -1.501 | (-3.631; 0.628) | |||||
| PA (WHO) | |||||||||
| ≥ 150 min/week | 0.307 | (-0.952; 1.567) | 0.000 | ||||||
| Total PA duration (min/week) | -0.001 | (-0.004; 0.002) | 0.000 | ||||||
B: β coefficient; CI: confidence interval; R2: coefficient of determination; AdjR2: adjusted coefficient of determination; HDL: high-density lipoprotein; LDL: low-density lipoprotein; TG: triglycerides; PA: physical activity; PA intensity: intensity of PA defined based on short IPAQ; TG: triglyceride; WHO: World Health Organization; Total PA duration: sum of PA in minutes per week;
Statistical significance p < 0.001;
Statistical significance 0.05 > p > 0.001;
Multiple regression with HDL, LDL and TG (natural logarithm) adjusted for sex, age;
Multiple regression with HDL and TG (natural logarithm) and PA adjusted for sex (only HDL), age, skin color, schooling (only HDL), per capita income, alcohol consumption, smoking, waist-hip ratio, body mass index, total carbohydrate and saturated fat intakes.
On multiple linear regression, comparing the adjusted coefficient of determination before and after the inclusion of the variable 'PA intensity' (R2 = 0.265 and 0.266, respectively), PA intensity explains only 0.1% of the total variability of HDL levels in the population studied. On the other hand, PA duration ≥ 150 min/week and total PA duration explained, respectively, 0.1% and 0.2% of the total variability of HDL levels in the ELSA-Brasil cohort, considering that adjusted coefficient of determination after the inclusion of those two PA variables were 0.266 and 0.267, respectively.
Comparing to insufficient-intensity PA, moderate-intensity PA was associated with a 0.89-mg/dL increase in HDL levels, and vigorous-intensity PA was associated with a 1.71-mg/dL increase in HDL levels, after adjusting for confounding factors (Table 4). That is, individuals with insufficient PA and HDL level of 50.8 mg/dL could have their HDL increased to 51.7 mg/dL or 52.5 mg/dL, when practicing moderate- or vigorous-intensity PA, respectively, and maintaining all other characteristics, behaviors and measures unchanged.
On simple linear regression, higher PA intensity, PA practice of at least 150 min/week and total PA duration (min/week) were associated with lower TG levels (Table 3). The associations found remained statistically significant after adjusting for sex, age and other confounding variables (race/skin color, per capita income, WHR, alcohol consumption, current smoking, and total carbohydrate and saturated fat intake).
The final adjusted results show that, as compared to insufficient PA, moderate and vigorous PA associated with a 0.98-mg/dL and 0.93-mg/dL reduction in the geometric mean of TG, respectively, indicating dose-response relationship. This implies that individuals with TG levels of 111.9 mg/dL and insufficient PA could reduce their TG values to 109.7 mg/dL or 104.6 mg/dL, respectively, by performing moderate or vigorous PA, and maintaining all other behavioral and anthropometric factors unchanged.
A PA practice greater than 150 min/week, as recommended by WHO, associated with a 0.98-mg/dL reduction in the geometric mean of TG. The comparison of the adjusted coefficient of determination of multivariate analysis before and after the inclusion of the 'PA intensity' variable (R2 = 0.228 and 0.230, respectively) indicates that PA explains only 0.2% of the variability of TG levels in the population studied. On the other hand, according to WHO recommendation, PA explains 0.1% of that distribution, because the adjusted coefficient of determination after the inclusion of PA intensity was 0.229.
On univariate analysis, LDL showed a statistically significant association with only vigorous-intensity PA. However, after adjusting for sex and age, PA association with LDL levels lost statistical significance; therefore, multivariate analysis was not performed (Table 3).
Discussion
The present study showed that PA practice, categorized into different aspects, associated independently with higher HDL concentrations and lower TG levels in a large sample of individuals not using lipid-lowering drugs. In addition, our results do not indicate that PA intensity is clearly superior or inferior to the PA duration of 150 min/week recommended by WHO. Considering that the Brazilian population has significant cardiovascular morbidity and mortality and high sedentary rate, our results are relevant because they emphasize the need to maintain and widen public programs to foster regular PA practice, aimed at improving the population's lipid profile.
Our results support those reported in studies assessing HDL and TG. Similarly, in studies on physical training, HDL increase and TG reduction are more frequently observed than a reduction in total cholesterol or LDL levels.28
To assess the impact of PA duration and intensity on HDL, LDL and TG levels, we analyzed separately the different parameters of PA classification. Some studies have reported a dose-response relationship in the association between PA intensity and lipid profile improvement, mainly HDL elevation and TG reduction in previously sedentary or inactive populations.6,9-11,29-31 In accordance with that, we found that the greater the PA intensity, the higher the mean increase in HDL levels and the lower the TG levels.
Three meta-analyses on the impact of physical training have shown mean increases in HDL of 1.2, 2.53 and 1.95 mg/dL, and mean reductions in TG of 15.8 and 7.12 mg/dL after the intervention.17,32,33 We found a mean increase in HDL of 0.89 mg/dL in individuals practicing moderate PA as compared to insufficient PA, and a 1.71-mg/dL increase for vigorous PA. Moderate PA reduced by 0.98 mg/dL the geometric mean of TG as compared to insufficient PA, while vigorous PA reduced by 0.93 mg/dL. The lipid profile improvement has a direct impact on the risk for CVD and diabetes. The Lipid Research Clinic Prevalence Mortality Follow-up (LRCF) has shown that the 1-mg/dL increase in HDL reduced by 3.5% the risk of coronary artery disease (CAD), and by 3.7% and 4.7% mortality in men and women, respectively.34 According to the results of HEART, a 1-mg/dL increment in plasma HDL is associated with a 2% to 3% reduction in the risk for CAD.7
Unlike studies reporting that the amount of exercise, as compared to exercise intensity, determined a higher difference in plasma lipoprotein concentrations,15,35,36 the present study found that both frequency and intensity are important for that effect, intensity exerting greater interference. Considering the findings of the ELSA-Brasil study and controversies in the literature, it is necessary to clarify the role played by PA, especially regarding PA amount and intensity, to improve the PA recommendations aimed at increasing HDL and reducing TG.
A Dutch cross-sectional study with individuals of three ethnicities, using the SQUASH questionnaire to measure PA level and the same ELSA-Brasil criteria to define favorable lipid profile, has reported that PA intensity, but not PA duration, associated with a more favorable lipid profile. Total PA duration associated with better HDL and TG levels only in Afro-Surinamese individuals.11 We observed a stronger association between vigorous-intensity PA and favorable lipid profile, in addition to an association with total PA duration per week, regardless of PA intensity. It is worth noting that 25% of the individuals had no leisure-time PA (total leisure-time PA = 0). Our results suggest that vigorous PA, but not moderate PA, is associated with greater benefit to lipid profile as compared to PA duration. It is worth noting that because of the cross-sectional design of this study, a causality relationship between PA, in any modality assessed, and TG and HDL levels could not be inferred.
According to 2011 WHO recommendation, adults should practice at least 150 min/week of insufficient-to-moderate-intensity PA during leisure time or at least 75 min/week of vigorous PA. In the present study, 64% of the participants did not reach the recommended PA level during leisure time, that percentage being higher among women (68.4%) than among men (57.7%). In addition, we observed that PA practice during the time recommended by WHO was associated with significantly higher HDL levels and lower TG levels, regardless of intensity. Therefore, our results support the WHO recommendation of at least 150 min/week of PA, which is simpler and easier to be disseminated as compared to intensity-based recommendations.
This study design observed measures to assure the quality of the information. The collection of data and biological material in the six centers followed strictly standardized procedures, undergoing constant quality control. Storage and laboratory tests were centralized in a certified laboratory. The sample was sufficiently large and heterogeneous (sex, age, schooling and behaviors) to assure statistical power for the analyses performed.23
It is worth noting, however, that the leisure-time PA section of the long IPAQ questionnaire has limitations and lower accuracy than PA measurement by use of objective devices.37,38 In large epidemiological investigations, such as ELSA-Brasil, however, the use of a questionnaire is an easy and low-cost way to assess PA, providing information that allows estimating PA levels, intensity and frequency. In addition, IPAQ has been validated in several countries, including in Brazil.39,40
The present study estimated the independent contribution of leisure-time PA during the past week on current HDL, LDL and TG levels. Part of the individuals classified as active in the past week might not be active routinely and vice-versa, or non-active individuals in the past week might be active most of the time. However, those errors might not be differential concerning lipid profile. Non-differential errors tend to attenuate the estimated associations, leading to underestimation of the real PA contribution to lipid profile in this study. It is worth noting that our analysis considered PA during neither transportation nor occupation.
Conclusion
A beneficial association exists between higher PA levels and a favorable HDL and TG lipid profile for men and women. Vigorous, but not moderate, PA practice was associated with more positive lipid profile changes than PA duration alone. Such findings contribute to support public policies of prevention and reduction of the risk for cardiometabolic diseases based on the expansion and facilitation of leisure-time PA practice.
Acknowledgments
ELSA-Brasil was financed by the Brazilian Ministry of Health (Department of Science and Technology), Ministry of Science and Technology (Financer of Studies and Projects and Brazilian National Research Board - CNPq), processes: 01 06 0010.00 RS, 01 06 0212.00BA, 01 06 0300.00 ES, 01 06 0278.00 MG, 01 06 0115.00SP, 01 06 0071.00 RJ. SM Barreto receives a research fellowship from CNPq (process 300159/99-4) and RCS received a Master's grant from CAPES.
Footnotes
Author contributions
Conception and design of the research, Statistical analysis and Writing of the manuscript: da Silva RC, Diniz MFHS, Barreto SM; Acquisition of data: Vidigal PG, Fedeli LMG, Barreto SM; Analysis and interpretation of the data: da Silva RC, Diniz MFHS, Alvim S, Vidigal PG, Fedeli LMG, Barreto SM; Obtaining financing: Barreto SM; Critical revision of the manuscript for intellectual content: Alvim S, Vidigal PG, Fedeli LMG, Barreto SM.
Potential Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Sources of Funding: This study was funded by Ministério da Saúde e Ministério da Ciência e Tecnologia.
Study Association: This article is part of the thesis of master submitted by Raquel Caroline da Silva, from Universidade Federal de Minas Gerais.
References
- 1.National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106(25):3143–3421. [PubMed] [Google Scholar]
- 2.Assmann G, Schulte H. Relation of high-density lipoprotein cholesterol and triglycerides to incidence of atherosclerotic coronary disease (the PROCAM experience). Prospective Cardiovascular Münster study. Am J Cardiol. 1992;70(7):733–737. doi: 10.1016/0002-9149(92)90550-i. [DOI] [PubMed] [Google Scholar]
- 3.Multiple Risk Factor Intervention Trial Research Group Multiple risk factor intervention trial. Risk factor changes and mortality results. JAMA. 1982;248(12):1465–1477. [PubMed] [Google Scholar]
- 4.Semenkovich CF, Goldberg AC, Goldberg IJ. Melmed S, Polonsky KS, Larsen PR, Kronenberg HM. Williams Textbook of Endocrinology. 12th ed. Philadelphia: Elsevier Saunders; 2011. Disorders of lipid metabolism; pp. 1633–1674. [Google Scholar]
- 5.Camont L, Chapman MJ, Kontush A. Biological activities of HDL subpopulations and their relevance to cardiovascular disease. Trends Mol Med. 2011;17(10):594–603. doi: 10.1016/j.molmed.2011.05.013. [DOI] [PubMed] [Google Scholar]
- 6.Skretteberg PT, Grundvold I, Kjeldsen SE, Erikssen JE, Sandvik L, Liestøl K, et al. HDL-cholesterol and prediction of coronary heart disease: modified by physical fitness? A 28-year follow-up of apparently healthy men. Atherosclerosis. 2012;220(1):250–256. doi: 10.1016/j.atherosclerosis.2011.10.009. [DOI] [PubMed] [Google Scholar]
- 7.Barter P, Gotto AM, LaRosa JC, Maroni J, Szarek M, Grundy SM, et al. Treating to New Targets Investigators HDL cholesterol, very low levels of LDL cholesterol, and cardiovascular events. N Engl J Med. 2007;357(13):1301–1310. doi: 10.1056/NEJMoa064278. [DOI] [PubMed] [Google Scholar]
- 8.Ineu ML, Manenti E, da Costa JL, Moriguchi E. HDL management: recent advances and perspectives beyond LDL reduction. Arq Bras Cardiol. 2006;87(6):788–794. doi: 10.1590/s0066-782x2006001900017. [DOI] [PubMed] [Google Scholar]
- 9.Halverstadt A, Phares DA, Wilund KR, Goldberg AP, Hagberg JM. Endurance exercise training raises high-density lipoprotein cholesterol and lowers small low-density lipoprotein and very low-density lipoprotein independent of body fat phenotypes in older men and women. Metabolism. 2007;56(4):444–450. doi: 10.1016/j.metabol.2006.10.019. [DOI] [PubMed] [Google Scholar]
- 10.Kraus WE, Houmard JA, Duscha BD, Knetzger KJ, Wharton MB, McCartney JS, et al. Effects of the amount and intensity of exercise on plasma lipoproteins. N Engl J Med. 2002;347(19):1483–1492. doi: 10.1056/NEJMoa020194. [DOI] [PubMed] [Google Scholar]
- 11.de Munter JS, van Valkengoed IG, Stronks K, Agyemang C. Total physical activity might not be a good measure in the relationship with HDL cholesterol and triglycerides in a multi-ethnic population: a cross-sectional study. Lipids Health Dis. 2011;10:223–223. doi: 10.1186/1476-511X-10-223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Romero Moraleda B, Morencos E, Peinado AB, Bermejo L, Gomez Candela C, Benito PJ, PRONAF Study group Can the exercise mode determine lipid profile improvements in obese patients. Nutr Hosp. 2013;28(3):607–617. doi: 10.3305/nh.2013.28.3.6284. [DOI] [PubMed] [Google Scholar]
- 13.Lehmann R, Engler H, Honegger R, Riesen W, Spinas GA. Alterations of lipolytic enzymes and high-density lipoprotein subfractions induced by physical activity in type 2 diabetes mellitus. Eur J Clin Invest. 2001;31(1):37–44. doi: 10.1046/j.1365-2362.2001.00752.x. [DOI] [PubMed] [Google Scholar]
- 14.Braun LT, Rosenson RS. Freeman MW, editor; Waltham MA. Effects of exercise on lipoproteins and hemostatic factors. [2015 Dec 10]. Available from: http://www.curenarm.net/UPTODATE/contents/mobipreview.htm?11/49/120063?source=see_link.
- 15.King AC, Haskell WL, Young DR, Oka RK, Stefanick ML. Long-term effects of varying intensities and formats of physical activity on participation rates, fitness, and lipoproteins in men and women aged 50 to 65 years. Circulation. 1995;91(10):2596–2604. doi: 10.1161/01.cir.91.10.2596. [DOI] [PubMed] [Google Scholar]
- 16.Kodama S, Tanaka S, Saito K, Shu M, Sone Y, Onitake F, et al. Effect of aerobic exercise training on serum levels of high-density lipoprotein cholesterol: a meta-analysis. Arch Intern Med. 2007;167(10):999–1008. doi: 10.1001/archinte.167.10.999. [DOI] [PubMed] [Google Scholar]
- 17.O'Donovan G, Owen A, Bird S, Kearney EM, Nevill AM, Jones DW, et al. Changes in cardiorespiratory fitness and coronary heart disease risk factors following 24 wk of moderate- or high-intensity exercise of equal energy cost. J Appl Physiol. 2005;98(5):1619–1625. doi: 10.1152/japplphysiol.01310.2004. [DOI] [PubMed] [Google Scholar]
- 18.World Health Organization . Global recommendations on physical activity for health. 2011. [2015 Dec 10]. Available from: http://www.who.int/dietphysicalactivity/publications/9789241599979/en/ [PubMed] [Google Scholar]
- 19.Schmidt MI, Duncan BB, Mill JG, Lotufo PA, Chor D, Barreto SM, et al. Cohort profile: Longitudinal Study of Adult Health (ELSA-Brasil) Int J Epidemiol. 2015;44(1):68–75. doi: 10.1093/ije/dyu027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Aquino EM, Barreto SM, Bensenor IM, Carvalho MS, Chor D, Duncan BB, et al. Brazilian Longitudinal Study of Adult Health (ELSA-Brasil): objectives and design. Am J Epidemiol. 2012;175(4):315–324. doi: 10.1093/aje/kwr294. [DOI] [PubMed] [Google Scholar]
- 21.Fedeli LG, Vidigal PG, Leite CM, Castilhos CD, Pimentel RA, Maniero VC, et al. Logistics of collection and transportation of biological samples and the organization of the central laboratory in the ELSA-Brasil. Rev Saude Publica. 2013;47(2):63–71. doi: 10.1590/s0034-8910.2013047003807. [DOI] [PubMed] [Google Scholar]
- 22.Grimm EK, Swartz AM, Hart T, Miller NE, Strath SJ. Comparison of the IPAQ-short form and accelerometry predictions of physical activity in older adults. J Aging Phys Act. 2012;20(1):64–79. doi: 10.1123/japa.20.1.64. [DOI] [PubMed] [Google Scholar]
- 23.Schmidt MI, Griep RH, Passos VM, Luft VC, Goulart AC, Menezes GM, et al. Strategies and development of quality assurance and control in the ELSA-Brasil. Rev Saude Publica. 2013;47(Suppl 2):105–112. doi: 10.1590/s0034-8910.2013047003889. [DOI] [PubMed] [Google Scholar]
- 24.Xavier HT, Izar MC, Faria Neto JR, Assad MH, Rocha VZ, Sposito AC, et al. Sociedade Brasileira de Cardiologia V Diretriz brasileira de dislipidemias e prevenção da aterosclerose. Arq. Bras. Cardiol. 2013;101(4 Suppl 1):1–20. doi: 10.5935/abc.2013S010. [DOI] [PubMed] [Google Scholar]
- 25.Mil JG, Pinto K, Griep RH, Goulart A, Foppa M, Lotufo PA, et al. Medical assessments and measurements in ELSA-Brasil. Rev Saúde Pública. 2013;47(Suppl 2):54–62. doi: 10.1590/s0034-8910.2013047003851. [DOI] [PubMed] [Google Scholar]
- 26.Guidelines for data processing and analysis of the International Physical Activity Questionnaire (IPAQ) - Short and long forms. [2015 Dec 10]. Nov, 2005. Available from: http://www.ipaq.ki.se/dloads/IPAQ%20LS%20Scoring%20Protocols_Nov05.pdf. [Google Scholar]
- 27.Molina MdelC, Benseñor IM, Cardoso L de O, Velasquez-Melendez G, Drehmer M, Pereira TS, et al. Reproducibility and relative validity of the Food Frequency Questionnaire used in the ELSA-Brasil. Cad Saude Publica. 2013;29(2):379–389. [PubMed] [Google Scholar]
- 28.Durstine JL, Grandjean PW, Cox CA, Thompson PD. Lipids, lipoproteins, and exercise. J Cardiopulm Rehabil. 2002;22(6):385–398. doi: 10.1097/00008483-200211000-00002. [DOI] [PubMed] [Google Scholar]
- 29.Guedes DP, Gonçalves LA. Impact of the habitual physical activity on lipid profile in adults. Arq Bras Endocrinol Metabol. 2007;51(1):72–78. doi: 10.1590/s0004-27302007000100012. [DOI] [PubMed] [Google Scholar]
- 30.Monda KL, Ballantyne CM, North KE. Longitudinal impact of physical activity on lipid profiles in middle-aged adults: the Atherosclerosis Risk in Communities Study. J Lipid Res. 2009;50(8):1685–1691. doi: 10.1194/jlr.P900029-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mann S, Beedie C, Jimenez A. Differential effects of aerobic exercise, resistance training and combined exercise modalities on cholesterol and the lipid profile: review, synthesis and recommendations. Sports Med. 2014;44(2):211–221. doi: 10.1007/s40279-013-0110-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tran ZV, Weltman A, Glass GV, Mood DP. The effects of exercise on blood lipids and lipoproteins: a meta-analysis of studies. Med Sci Sports Exerc. 1983;15(5):393–402. [PubMed] [Google Scholar]
- 33.Halbert JA, Silagy CA, Finucane P, Withers RT, Hamdorf PA. Exercise training and blood lipids in hyperlipidemic and normolipidemic adults: a meta-analysis of randomized, controlled trials. Eur J Clin Nutr. 1999;53(7):514–522. doi: 10.1038/sj.ejcn.1600784. [DOI] [PubMed] [Google Scholar]
- 34.Forti N, Diament J. High-density lipoproteins: metabolic, clinical, epidemiological and therapeutic intervention aspects. An update for clinicians. Arq Bras Cardiol. 2006;87(5):671–679. doi: 10.1590/s0066-782x2006001800019. [DOI] [PubMed] [Google Scholar]
- 35.Wood PD, Haskell WL, Blair SN, Williams PT, Krauss RM, Lindgren FT, et al. Increased exercise level and plasma lipoprotein concentrations: a one-year, randomized, controlled study in sedentary, middle-aged men. Metabolism. 1983;32(1):31–39. doi: 10.1016/0026-0495(83)90152-x. [DOI] [PubMed] [Google Scholar]
- 36.Kokkinos PF, Holland JC, Narayan P, Colleran JA, Dotson CO, Papademetriou V. Miles run per week and high-density lipoprotein cholesterol levels in healthy, middle-aged men: a dose-response relationship. Arch Intern Med. 1995;155(4):415–420. [PubMed] [Google Scholar]
- 37.Sunami Y, Motoyama M, Kinoshita F, Mizooka Y, Sueta K, Matsunaga A, et al. Effects of low-intensity aerobic training on the high-density lipoprotein cholesterol concentration in healthy elderly subjects. Metabolism. 1999;48(8):984–988. doi: 10.1016/s0026-0495(99)90194-4. [DOI] [PubMed] [Google Scholar]
- 38.Santos CM, Barbosa JM, Cheng LA, Wanderley Júnior RS, Barros MV. Atividade física no contexto dos deslocamentos: revisão sistemática dos estudos epidemiológicos realizados no Brasil. Rev Bras Ativ Fis Saúde Pelotas/RS. 2009;14(1):15–22. [Google Scholar]
- 39.Celis-Morales CA, Perez-Bravo F, Ibañez L, Salas C, Bailey ME, Gill JM. Objective vs. self-reported physical activity and sedentary time: effects of measurement method on relationships with risk biomarkers. PLoS One. 2012;7(5): doi: 10.1371/journal.pone.0036345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lee PH, Macfarlane DJ, Lam TH, Stewart SM. Validity of the international physical activity questionnaire short form (IPAQ-SF): a systematic review. Int J Behav Nutr Phys Act. 2011;8:115–115. doi: 10.1186/1479-5868-8-115. [DOI] [PMC free article] [PubMed] [Google Scholar]