Abstract
Tertiary hyperparathyroidism is a common cause of hypercalcemia after kidney transplant. We designed this 12-month, prospective, multicenter, open–label, randomized study to evaluate whether subtotal parathyroidectomy is more effective than cinacalcet for controlling hypercalcemia caused by persistent hyperparathyroidism after kidney transplant. Kidney allograft recipients with hypercalcemia and elevated intact parathyroid hormone (iPTH) concentration were eligible if they had received a transplant ≥6 months before the study and had an eGFR>30 ml/min per 1.73 m2. The primary end point was the proportion of patients with normocalcemia at 12 months. Secondary end points were serum iPTH concentration, serum phosphate concentration, bone mineral density, vascular calcification, renal function, patient and graft survival, and economic cost. In total, 30 patients were randomized to receive cinacalcet (n=15) or subtotal parathyroidectomy (n=15). At 12 months, ten of 15 patients in the cinacalcet group and 15 of 15 patients in the parathyroidectomy group (P=0.04) achieved normocalcemia. Normalization of serum phosphate concentration occurred in almost all patients. Subtotal parathyroidectomy induced greater reduction of iPTH and associated with a significant increase in femoral neck bone mineral density; vascular calcification remained unchanged in both groups. The most frequent adverse events were digestive intolerance in the cinacalcet group and hypocalcemia in the parathyroidectomy group. Surgery would be more cost effective than cinacalcet if cinacalcet duration reached 14 months. All patients were alive with a functioning graft at the end of follow-up. In conclusion, subtotal parathyroidectomy was superior to cinacalcet in controlling hypercalcemia in these patients with kidney transplants and persistent hyperparathyroidism.
Keywords: hyperparathyroidism, renal transplantation, calcium
Kidney transplantation is the best therapeutic option for patients with ESRD.1 Improvements in transplant care and new immunosuppressive drugs have led to a progressive increase in short–term graft survival.2 However, long-term outcome has not increased accordingly because of progressive chronic allograft damage and patient death.3 Persistent hyperparathyroidism has been associated with both chronic allograft nephropathy4 and cardiovascular morbidity and mortality after kidney transplantation.5,6
Secondary hyperparathyroidism is a common complication in CKD. Parathyroid glands are committed to secrete parathyroid hormone (PTH) to correct calcium and phosphate serum levels. However, progressive decline in GFR overcomes the compensatory capacity of PTH. Continuous stimulation on parathyroid tissue induces relevant pathogenic abnormalities as downregulation of the vitamin D receptor and calcium-sensing receptor, which result in the loss of PTH calcium–dependent autoregulation.7 Indeed, parathyroid glands become hyperplasic, and even adenoma can be developed. Kidney transplantation rapidly restores GFR and the renal capacity to respond to PTH (that is, phosphaturia and tubular calcium reabsorption).8,9 Usually, some degree of autoregulation is preserved with progressive PTH reduction and regression of parathyroid hyperplasia a few months after transplantation. However, in 20%–30% of patients, parathyroid gland resistance to inhibitory feedback persisted several years after transplantation,9 and inappropriately high PTH levels are associated with hypercalcemia, hypophosphatemia, renal allograft calcifications and dysfunction, loss of bone mineral density (BMD) and increased risk of fracture, vascular calcification, and increased risk of cardiovascular events.10–13 These patients are diagnosed with tertiary hyperparathyroidism or persistent hyperparathyroidism after kidney transplantation.
Long–term clinical management is rather controversial and very limited because of hypercalcemia that can be aggravated by vitamin D supplementation or vitamin D analogs.14,15 Subtotal parathyroidectomy has been considered until recently the only therapeutic approach. However, it is an invasive procedure with potential surgical complications, because it is sometimes difficult to determine the precise amount of gland to be removed.16 Therefore, a surgical expertise is critical to minimize complications and reduce the risk of hypoparathyroidism and unsatisfactory reduction of PTH. Physicians and patients are reluctant to indicate or accept subtotal parathyroidectomy,17,18 especially after the appearance of cinacalcet into the clinics. Cinacalcet (Mimpara; Amgen Inc., Thousand Oaks, CA) is an allosteric modulator of the calcium-sensing receptor that is able to reduce PTH and calcium in patients on dialysis with secondary hyperparathyroidism.19 In renal transplant recipients with tertiary hyperparathyroidism, a recent clinical trial showed that cinacalcet is superior to placebo at correcting hypercalcemia and hypophosphatemia.20 However, there are no clinical studies comparing cinacalcet with subtotal parathyroidectomy in this setting.
Results
Study Population
Thirty-seven patients fulfilling criteria were assessed for eligibility. Seven patients were screening failures (three withdrew consent before any study procedure, and four had laboratory values during that screening visit that did not comply with inclusion/exclusion criteria). In total, 30 patients were randomized (intention to treat population) to receive cinacalcet (n=15) or parathyroidectomy (n=15). Table 1 shows patient baseline main clinical characteristics. Patients were included in the study a mean time of 45 months after transplantation. Regarding maintenance immunosuppression, 15 of 30 were on a steroid-free regime, and 24 of 30 were on tacrolimus. All patients on steroids were receiving 5 mg/d prednisone without modification during the study. There were two patients on cyclosporin (one in each arm) and four patients on sirolimus (two in each arm). All patients were on mycophenolate.
Table 1.
Patient baseline characteristics
| Variable | All Patients (n=30) | Cinacalcet (n=15) | Subtotal Parathyroidectomy (n=15) | P Value |
|---|---|---|---|---|
| Age, yr | 53.9±12.4 | 55.0±13.6 | 53.0±11.8 | 0.67 |
| Sex, men/women | 13/17 | 7/8 | 6/9 | 0.71 |
| Time on dialysis, mo | 38.8±29.2 | 33.5±26.9 | 44.1±32.5 | 0.39 |
| Cause of ESRD | ||||
| Diabetes | 2 | 1 | 1 | |
| Hypertension | 4 | 2 | 2 | |
| GN | 5 | 2 | 3 | |
| ADPKD | 5 | 3 | 2 | |
| Other | 14 | 7 | 7 | |
| Previous transplant, yes/no | 4/26 | 2/13 | 2/13 | >0.99 |
| Time after kidney transplantation, mo | 45.5±39.9 | 46.5±42.2 | 44.4±38.8 | 0.89 |
| BP, mmHg | ||||
| Systolic | 140±20 | 136±22 | 147±16 | 0.13 |
| Diastolic | 82±14 | 80±11 | 84±16 | 0.33 |
| Steroid treatment, yes/no | 15/15 | 7/8 | 8/7 | 0.90 |
| Tacrolimus, yes/no | 24/6 | 12/3 | 12/3 | >0.99 |
Data is displayed as means±standard deviation and number of cases/events. ADPKD, autosomical dominant polycystic kidney disease.
In the cinacalcet group, the starting cinacalcet dose was 30 mg/d, and then, it was adjusted to accomplish normocalcemia. At month 3, cinacalcet doses were 60 mg/d (33%) and 30 mg/d (67%), and at month 12, they were 60 mg/d (36%) and 30 mg/d (64%). One patient discontinued cinacalcet at month 3 because of oral intolerance. Surgical intact parathyroid hormone (iPTH) reduction was assessed during the surgical procedure (Figure 1). The iPTH decline 10 minutes after parathyroid gland removal ranged between 75.1% and 97.7%.
Figure 1.
The iPTH decline early after subtotal parathyroidectomy was higher than 75%. Assessment of iPTH decline early after subtotal parathyroidectomy. iPTH was measured at baseline and 10 minutes after surgery to assure that enough parathyroid gland tissue had been removed.
Baseline serum calcium, phosphate, iPTH, and calcidiol serum levels as well as eGFR and proteinuria were similar between both groups (Table 2).
Table 2.
Evolution of serum calcium, phosphate, iPTH, biomarkers of bone turnover, renal function, and vascular calcification
| Variable | Cinacalcet | Subtotal Parathyroidectomy | ||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | Month 3 | Month 6 | Month 12 | Baseline | Month 3 | Month 6 | Month 12 | |
| Albumin, g/L | 43.9±2.8 | 44.1±1.9 | 43.9±2.5 | 43.7±3.1 | 44.5±2.4 | 44.4±2.8 | 44.1±3.3 | 43.4±3.0 |
| Calcium, mmol/L | 2.72±0.1 | 2.42±0.2a | 2.42±0.2a | 2.37±0.2a | 2.78±0.2 | 2.28±0.2b | 2.26±0.2b | 2.22±0.2b |
| iPTH, pmol/L | 25±12 | 18±7a | 20±9a | 22±11 | 37±18 | 9±10b | 7±6b | 6±5b |
| Phosphorus, mmol/L | 0.92±0.2 | 1.1±0.1a | 1.0±0.2a | 1.1±0.1a | 0.93±0.2 | 1.3±0.2b | 1.3±0.2b | 1.3±0.3b |
| 25(OH)D3 for calcidiol, nmol/L | 51±24 | 57±21 | 59±21 | 53±15 | 41±14 | 90±32b | 79±31b | 70±30b |
| Bone resorption biomarker | ||||||||
| C-terminal telopeptide, μg/L | 0.48±0.22 | 0.72±0.44a | 0.72±0.35a | 0.71±0.45a | 0.48±0.27 | 0.26±0.24b | 0.13±0.14b | 0.33±0.35b |
| Bone formation biomarkers | ||||||||
| Alkaline phosphatase, μKat/L | 2.2±1.7 | 2.2±1.1 | 2.2±1.2 | 1.5±0.5a | 1.9±0.9 | 2.2±1.6 | 1.8±1.2 | 1.7±1.1b |
| Osteocalcin, μg/L | 32±16 | 41±23 | 37±17 | 40±27 | 28±19 | 25±18 | 25±8 | 22±13b |
| Renal function | ||||||||
| eGFR, ml/min | 57±11 | 54±16 | 53±6 | 48±14a | 57±16 | 52±14 | 53±17 | 53±14 |
| Proteinuria, mg/d | 195±150 | 144±110 | 171±135 | 200±169 | 243±150 | 264±273 | 234±229 | 251±362 |
| Vascular calcification | ||||||||
| Abdominal aorta calcification score | 4.9±3.4 | — | 5.1±3.8 | 5.2±3.9 | 4.9±3.8 | — | 5.0±3.8 | 5.0±3.8 |
| Vascular calcification score | 17.0±13.5 | — | 18.6±13.8 | 18.8±14.2 | 17.7±12.7 | — | 17.3±13.7 | 17.6±13.7 |
25(OH)D3, 25-hydroxy vitamin D (calcidiol); μKat, katal; —, not done as per protocol.
P<0.05 versus baseline in the cinacalcet group.
P<0.05 versus baseline in the subtotal parathyroidectomy group.
Primary End Point
The proportion of patients achieving the objective of normocalcemia (serum calcium within 2.22–2.55 mmol/L) at 12 months was ten of 15 (67%) in the cinacalcet group and 15 of 15 (100%) in the parathyroidectomy group (P=0.04). The evolution of calcium serum levels is depicted in Figure 2A and Table 2. A major limitation to increase cinacalcet dose to achieve normocalcemia in the cinacalcet group was digestive intolerance.
Figure 2.
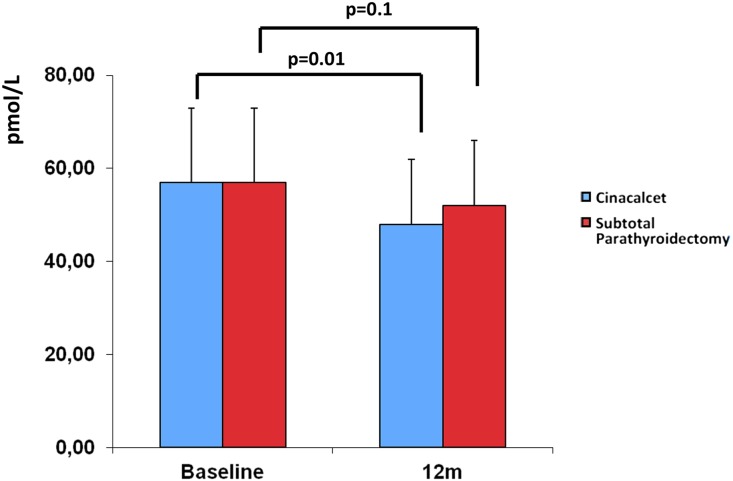
Subtotal parathyroidectomy was associated with a higher proportion of patients achieving normocalcemia and iPTH normalization. (A) Serum calcium, (B) iPTH, and (C) phosphate evolution in the cinacalcet and subtotal parathyroidectomy groups. Both treatments was associated with correction of calcium and phosphate, although the reduction of iPTH was greater in the parathyroidectomy group than in the cinacalcet group.
Secondary End Points
The evolution of serum iPTH is shown in Figure 2B. iPTH was similar in both groups at baseline. The reduction of iPTH was significantly greater in the parathyroidectomy group than in the cinacalcet group. Normalization of iPTH (serum iPTH within 1.13–7.11 pmol/L) at 12 months was accomplished in zero pf 15 in the cinacalcet group versus ten of 15 after subtotal parathyroidectomy (P=0.002). iPTH values in five patients in the parathyroidectomy group who did not achieve a normal level were 0.32, 7.9, 8.9, 17.3, and 15.48 pmol/L. Normalization of serum phosphate at month 12 (0.85–1.5 mmol/L) was achieved in 14 of 15 in the cinacalcet group and 15 of 15 in the parathyroidectomy group, although serum phosphate values at 3, 6, and 12 months were higher in the parathyroidectomy group (Figure 2C).
Markers of bone turnover are shown in Table 2. Bone–specific alkaline phosphatase decreased over time in both groups, whereas osteocalcin decreased at 12 months only after subtotal parathyroidectomy. The bone resorption biomarker C–terminal telopeptide was significantly reduced only after subtotal parathyroidectomy. Also, calcidiol levels increased over time only after subtotal parathyroidectomy, because the majority of patients received oral calcium and vitamin D supplementation early after surgery to prevent hypocalcemia caused by hungry bone syndrome. Nevertheless, in the cinacalcet group, mean levels of calcidiol were >50 nmol/L during all of the study follow-up. Interestingly, only subtotal parathyroidectomy was associated with a significant improvement in BMD at 12 months, in particular in the femoral neck as shown in Table 3.
Table 3.
BMD at baseline and month 12 with percentage changes of BMD calculated in the study groups
| Variable | Subtotal Parathyroidectomy | Cinacalcet | P Value |
|---|---|---|---|
| BMD baseline, g/cm2 | |||
| Femoral neck | 0.819±0.164 | 0.723±0.089 | 0.12 |
| Lumbar spine | 0.993±0.227 | 0.904±0.106 | 0.25 |
| Distal 1/3 radius | 0.613±0.097 | 0.661±0.116 | 0.30 |
| BMD month 12, g/cm2 | Article I. | ||
| Femoral neck | 0.846±0.149 | 0.700±0.081 | 0.01 |
| Lumbar spine | 1.015±0.213 | 0.896±0.109 | 0.11 |
| Distal 1/3 radius | 0.630±0.086 | 0.658±0.114 | 0.52 |
| Change at month 12, % | |||
| Femoral neck | +3.8±6.1 | −3.0±5.1 | 0.01 |
| Lumbar spine | +2.7±7.8 | −0.9±4.7 | 0.21 |
| Distal 1/3 radius | +3.3±6.6 | −0.4±2.6 | 0.10 |
Data is displayed as means±standard deviation.
Evolution of eGFR and proteinuria is shown in Table 2. There was some degree of eGFR loss in both groups without increase in proteinuria. During the 12-month follow-up, eGFR decline was 9 ml/min in the cinacalcet group (P=0.01) and 4 ml/min in the parathyroidectomy group (P=0.10) (Figure 3). However, no statistically significant differences were observed in GFR between both groups.
Figure 3.
There was some degree of eGFR loss in the cinacalcet and subtotal parathyroidectomy groups. eGFR at baseline and month 12 in the cinacalcet and subtotal parathyroidectomy groups. Decline in renal function was greater in the cinacalcet group than in the parathyroidectomy group.
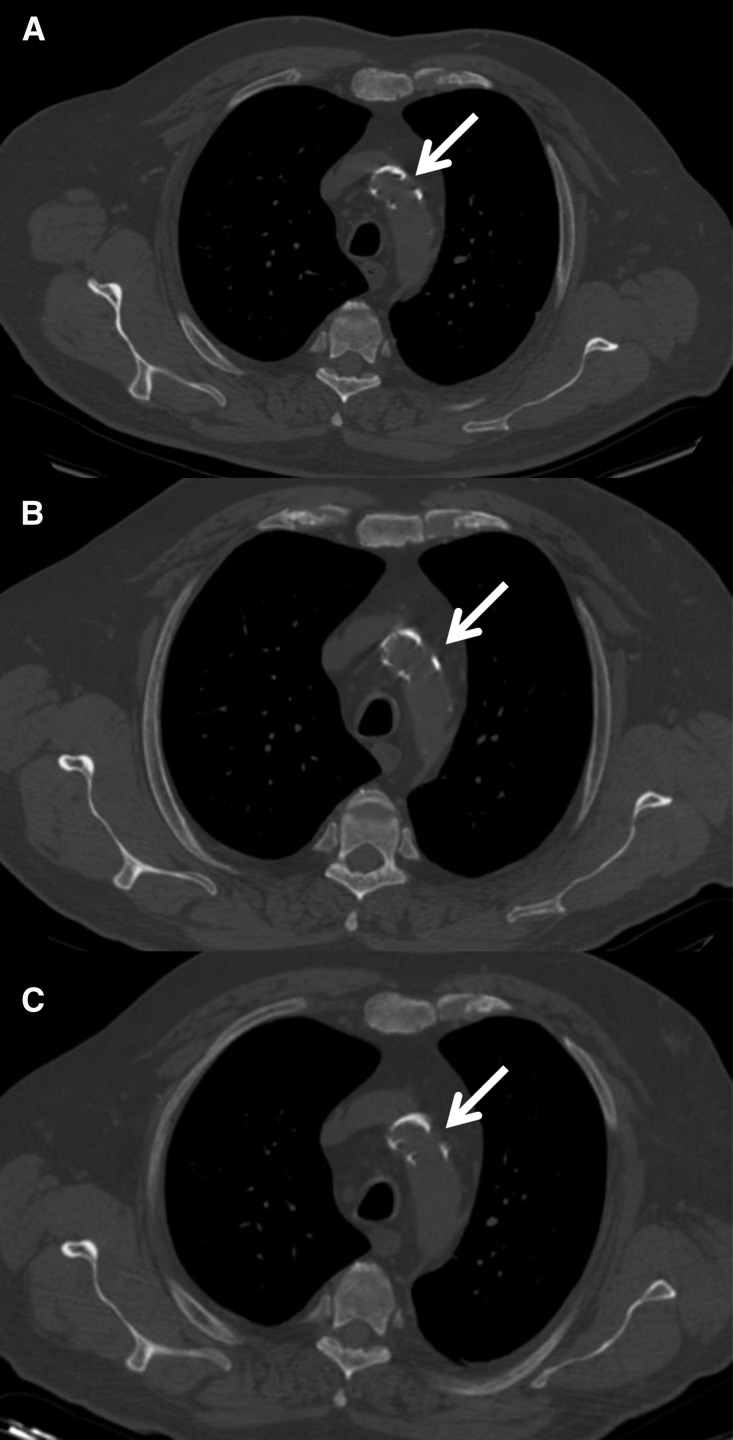
We performed assessment of vascular calcification by computed tomography (CT) at baseline and 6 and 12 months. No differences were observed between groups at baseline, and calcification score remained unchanged during follow-up (Figure 4, Table 2).
Figure 4.
Vascular calcification score remained unchanged in the cinacalcet and subtotal parathyroidectomy groups. A representative patient to assess changes in vascular calcification. Unenhanced CT scan at the level of the aortic arch in the same patient at (A) baseline, (B) 6 months, and (C) 12 months. Multiple plaques are seen (arrows), with no variation during the follow-up. Calcification value at this level was three at all three time points.
Safety
One patient in the cinacalcet group discontinued the drug because of digestive intolerance and severe xerostomia. Adverse events in the cinacalcet arm were diarrhea (n=2), nausea/vomiting (n=2), edema (n=2), urinary tract infection (n=2), and renal dysfunction (n=2). Adverse events in the parathyroidectomy group were hypocalcemia (n=4), traumatic tibial fracture (n=1), diarrhea (n=3), transient dysphonia (n=2), and intraductal breast cancer (n=1). There were two patients requiring hospitalization because of severe hypocalcemia after parathyroidectomy, whereas one patient in the cinacalcet group was admitted to the hospital because of severe diarrhea. During the course of the study, no acute rejection episodes, cytomegalovirus, or BK virus infections were observed. All patients were alive with a functioning graft at the end of follow-up.
Economic Study
The cost of both therapies for the Catalan Health Service was calculated. In the parathyroidectomy group, we included parathyroid gland scintigraphy; neck ultrasound; preoperative assessment; surgical, anesthetic, and hospitalization costs; pathologic report; rehospitalization cost; and calcium and vitamin D supplies. In the cinacalcet group, we included parathyroid gland scintigraphy, rehospitalization cost, and cinacalcet therapy. One-year cost per patient was 3712 euros in the parathyroidectomy group and 3258 euros in the cinacalcet group (12% higher in parathyroidectomy). The 1-year cost of cinacalcet drug was 3003 euros per patient (1-month cost per patient was 250 euros). Therefore, if cinacalcet treatment duration reached at least 14 months, subtotal parathyroidectomy would be considered superior in terms of cost-effectiveness.
Discussion
This study shows that standard of care subtotal parathyroidectomy is superior to cinacalcet to correct hypercalcemia in renal allograft recipients with persistent hyperparathyroidism. All patients with subtotal parathyroidectomy and ≤70% with cinacalcet achieved normocalcemia. Moreover, the reduction of iPTH was greater in the parathyroidectomy group than in the cinacalcet group. Accordingly, only subtotal parathyroidectomy was associated with a significant improvement in BMD in femoral neck.
A recent clinical trial showed that cinacalcet compared with placebo is a highly effective treatment option for correcting serum calcium levels among this population.20 Our results in the cinacalcet arm were similar, because the majority of patients achieved normal serum calcium and phosphate levels. Also, in both studies, cinacalcet reduced iPTH, although it persisted above normal range in a high proportion of patients. It is postulated in experimental studies that cinacalcet increases calcitonin levels and thus, decreases blood calcium levels21; this could be explained by the activation of sensitive calcium receptors present in the C cells of the thyroid gland. This theory could explain why, in many studies involving cinacalcet treatment of hypercalcemia in secondary hyperparathyroidism, serum calcium levels significantly decrease without a parallel decrease in PTH. In fact, the high level of the bone turnover biomarker C–terminal telopeptide throughout the study in the cinacalcet group suggests that persistence of hyperparathyroidism could be the potential explanation for the lack of improvement in BMD in patients treated with this drug.20 Alternatively, given the high prevalence of low bone turnover in transplant recipients with hypercalcemia and hyperparathyroidism, it has been suggested that cinacalcet or even parathyroidectomy may exacerbate adynamic bone disease.22 Adynamic bone disease can be indirectly assessed by bone turnover biomarkers.23 Among them, alkaline phosphatase is the best. In this regard, alkaline phosphatase levels, although with some decline, were maintained above normal range. In theory, normal range alkaline phosphatase makes the presence of adynamic bone disease unlikely. Moreover, the performance of osteocalcin was similar. Therefore, it seems that, at least after 1-year follow-up, the assessment of bone synthesis biomarkers does not suggest the presence of adynamic bone disease in cinacalcet and parathyroidectomy groups. Instead, in our study, subtotal parathyroidectomy was associated with improvement in BMD and regulation of biomarkers of high bone turnover. The cause would be iPTH normalization and/or the oral calcium and vitamin D supplementation given after parathyroidectomy to prevent hypocalcemia associated with hungry bone syndrome, which was confirmed by a significant increase in calcidiol levels.14,24 Additional studies with cinacalcet combined with vitamin D in which iPTH correction would be the primary end point are needed to ask this question properly.
Vascular calcification is an important complication in patients with secondary hyperparathyroidism.25 We observed similar results in cinacalcet and parathyroidectomy groups, and both treatments were associated with no progression in vascular calcification. Subtotal parathyroidectomy was not associated with regression of vascular calcification, although nearly full correction of serum calcium and iPTH was achieved. This fact suggests that vascular calcification is not reversible, at least in the short term, and reinforces the importance of preventing bone mineral disorders in early stages of CKDs.
There are some previous studies suggesting that both cinacalcet and parathyroidectomy are associated with a decrease in renal function.17,26 However, this effect was not observed in the previous cinacalcet clinical trial,20 and long–term graft outcome was not affected by parathyroidectomy.26 A renal hemodynamic mechanism was suggested, because iPTH has a known positive regulatory effect on renal perfusion and GFR that can be abrogated by intervention therapies.27 In our study, a 12-month GFR decline was observed in both groups, although it was greater in the cinacalcet group than in the parathyroidectomy group. There were no rejection episodes to explain this finding. The gastrointestinal adverse events observed in some patients treated with cinacalcet could be associated with hypovolemia and renal dysfunction. Previous studies showed association between high iPTH levels, kidney allograft interstitial calcification, and loss of renal function, providing a rationale to our finding.28 However, we did not perform protocol biopsies to corroborate this hypothesis.
As previously reported, the most frequently reported adverse event in the cinacalcet group was digestive intolerance,29 being a limitation to increasing the cinacalcet dose sufficiently to achieve serum calcium correction in some patients. Complications of subtotal parathyroidectomy depend on both surgical experience and the procedure itself.16 A recent study reviewed early outcomes of 4435 patients on dialysis who underwent parathyroidectomy30 and reported 2% mortality and 23.8% rehospitalization 30 days after discharge. Nevertheless, other studies have shown that successful parathyroidectomy may reduce the risk for all-cause and cardiovascular mortality in patients on dialysis.31,32 To minimize surgical bias, the same surgical team performed all parathyroid surgeries. A minimal invasive procedure with assessment of early drop in iPTH to ascertain that enough parathyroid gland tissue had been removed was carried out. In our study, early rehospitalization was 13% after parathyroidectomy and 7% in the cinacalcet group. As expected, the main complication after subtotal parathyroidectomy was hypocalcemia, some of which was related to oral intolerance caused by high calcium doses and some of which was related to transient dysfonia caused by recurrent laryngeal nerve mild surgical traumatism.
There is a paucity of data regarding the optimal management of tertiary hyperparathyroidism.22 A cost-utility analysis has been reported comparing subtotal parathyroidectomy with cinacalcet in patients on dialysis with severe hyperparathyroidism.33 This study concluded that surgery was more cost effective if cinacalcet treatment duration reached 16 months. Our study provides similar results in the renal transplantation setting, because the 1-year economic cost associated with both treatments is similar, suggesting that subtotal parathyroidectomy is more cost effective in the long term. However, this estimate applies in Spain and should be considered cautiously in other countries.
Our study has some limitations. First, follow-up is probably too short to provide relevant information about fracture risk, vascular calcification, and recurrence of hyperparathyroidism after subtotal parathyroidectomy. Second, cinacalcet dosage was adjusted to achieve normocalcemia without taking into account iPTH reduction. Third, the fact that the same surgeon performed all parathyroid surgeries could be a limitation to making a general recommendation. Fourth, in the absence of bone biopsies, it may be difficult to ascertain bone turnover in patients with renal transplants.34 Nevertheless, taking into account that our results in the cinacalcet arm are similar to those previously reported20 and that extended minimally invasive subtotal parathyroidectomy is a feasible approach,35 our results could reasonably be reproduced in a big clinical trial.
In conclusion, both cinacalcet and subtotal parathyroidectomy are effective to control hypercalcemia caused by persistent hyperparathyroidism after kidney transplantation. However, subtotal parathyroidectomy is superior to cinacalcet in terms of the proportion of patients achieving calcium (100% versus 67%; P=0.04) and iPTH (67% versus 0%; P<0.001) normalization, increase in BMD in the femoral neck (+3.8% versus −3%; P=0.01), and cost-effectiveness.
Concise Methods
Study Population
This was an investigator–promoted, prospective, multicenter, open–label, and randomized study performed in renal allograft recipients with hypercalcemia caused by post–transplant persistent hyperparathyroidism. The study was approved by The Spanish Drug Agency (EudraCT 2008–007017–76) and registered at ClinicalTrials.gov (NCT01178450).
Inclusion criteria were defined as follows: a functioning renal graft with an eGFR≥30 ml/min, at least 6 months after kidney transplantation, serum iPTH level ≥15 pmol/L, corrected total serum calcium level ≥2.63 mmol/L, and serum phosphate level ≤1.2 mmol/L. Before inclusion, patients were managed according to clinical guidelines and local clinical practice. Subjects were required to have a 16-week washout if they received cinacalcet. Use of vitamin D analogs and/or biphosphonates was not allowed during the study. Patients who did not meet the inclusion criteria or had a contraindication for surgery or cinacalcet treatment were excluded from the trial. Patients were included in the trial after providing written informed consent by signing an Ethics Committee–approved document in accordance to Good Clinical Practices. During the screening period, a complete laboratory assessment was performed (including iPTH and calcium and phosphate serum levels) to verify that patients met inclusion/exclusion criteria. At baseline, a parathyroid gammagraphy was performed to identify ectopic parathyroid tissue. Women of child-bearing potential were tested for pregnancy at the screening visit and informed to avoid pregnancy during the study. Patients who did not meet inclusion/exclusion criteria after the screening period were considered as screening failures and were not included in the statistical analysis.
Study Groups
Patients were randomized 1:1 to receive cinacalcet oral treatment or undergo a subtotal parathyroidectomy. Parathyroidectomy was performed in all patients by the same surgeon (P.M.) at Bellvitge Hospital. Briefly, the neck was explored bilaterally, and all parathyroid glands were identified and tissue was removed, leaving a remnant equivalent to one normal gland in size (50 mg). A perioperatively pathologic assessment was performed in all patients. A systematic transcervical thymectomy was also added to prevent persistent disease secondary to a fifth gland that could be present in ≤15% of patients. Intraoperative iPTH assessment was measured at baseline and 10 minutes after subtotal parathyroidectomy.
Patients assigned to the cinacalcet group started with 30 mg/d, and then, the dose was adjusted to achieve the objective of normocalcemia. Patients assigned to the subtotal parathyroidectomy group were scheduled to undergo surgery within 3 months with a previous neck ultrasound and preoperative screening. Patients were followed during 12 months after the initiation of the cinacalcet treatment or parathyroidectomy. Study visits were performed at baseline and 3, 6, and 12 months.
Primary and Secondary Efficacy End Points
The primary end point was the proportion of patients with normocalcemia at 12 months. Secondary end points were serum iPTH, serum phosphate, bone turnover biomarkers of BMD and vascular calcification, renal function, patient and graft survival, and economic cost associated with each treatment.
Serious and nonserious adverse events were monitored throughout the length of the study and reported accordingly. BMD was evaluated at baseline and month 12 at the femoral neck, lumbar spine, and distal 1/3 radius by dual x-ray absorptiometry centrally at Bellvitge Hospital. Vascular calcification evaluation was performed at baseline and 6 and 12 months and centralized at Bellvitge Hospital. Patients underwent thoracic, abdominal, and pelvis unenhanced CT scans. The images obtained were assessed for calcification detection and scoring by a radiologist (R.M.) who was blinded to therapy and timing of the CT scans. Imaging was performed using a 16– or 64–slice CT system (General Electric); 1.25-mm slices were obtained from the thorax, abdomen, and pelvis with posterior 0.625-mm-thick reconstructions. All of the images generated were analyzed using a GE Workstation. Images were analyzed using a window preset of bone. The level of the aortic arch was chosen as the starting point. From that point, we analyzed the supra-aortic trunks (origin of subclavia and carotid arteries); ascending aorta; descending thoracic aorta; diaphragmatic aorta; origin of the celiac trunk and superior mesenteric artery; suprarenal, renal, and infrarenal aortic bifurcation; right and left iliac bifurcation; and both proximal femoral arteries. The score was obtained on axial CT images. For each section, a value of zero was given for the absence of calcification deposit, one was given for presence of plaques, and two was given if more than four plaques were detected. An extra point was given when the plaque occupied >50% of the arterial circumference, and an extra two points were given when it was covering the entire circumference. Finally, one extra point was assigned when the thickness of the plaque was >4 mm in any of the deposits detected. On the basis of this system, the final score could be between 0 and 80. Stability or progression of calcifications deposits was achieved comparing the three CT scans performed for each patient.
Statistical Analyses
A sample size of 30 subjects (15 per arm) was estimated to provide 80% power to achieve a statistical significance of 0.05 (one sided) using the chi-squared test. This assumed a response rate for normocalcemia of 65% in cinacalcet and 95% in subtotal parathyroidectomy. An intention to treat analysis was performed. Differences in the categorical variables between both groups were calculated by means of the chi-squared test or the Fisher exact test. The differences in the quantitative variables, including the main variable between groups, were calculated by means of the t test or the Mann–Whitney U test. A P value <0.05 was considered significant for all tests. Results were depicted as means±SDs.
Disclosures
None.
Acknowledgments
We thank Pau Cruzado-Boix for assistance with English language revision.
This research was supported by Spanish Government Instituto de Salud Carlos III (ISCIII) Grants EC08/00237 and INT13/00126 (ClinicalTrials.gov identifier NCT01178450) under the auspices of The Red de Investigación Renal (European Regional Development Funds ISCIII Red Temática de Investigación Cooperativa en Salud Red de Investigación Renal; RD12/0021/0003).
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
See related editorial, “Parathyroidectomy or Calcimimetic to Treat Hypercalcemia after Kidney Transplantation?,” on pages 2221–2224.
References
- 1.Wolfe RA, Ashby VB, Milford EL, Ojo AO, Ettenger RE, Agodoa LY, Held PJ, Port FK: Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant. N Engl J Med 341: 1725–1730, 1999 [DOI] [PubMed] [Google Scholar]
- 2.Morris PJ: Transplantation--a medical miracle of the 20th century. N Engl J Med 351: 2678–2680, 2004 [DOI] [PubMed] [Google Scholar]
- 3.Gondos A, Döhler B, Brenner H, Opelz G: Kidney graft survival in Europe and the United States: Strikingly different long-term outcomes. Transplantation 95: 267–274, 2013 [DOI] [PubMed] [Google Scholar]
- 4.Schwarz A, Mengel M, Gwinner W, Radermacher J, Hiss M, Kreipe H, Haller H: Risk factors for chronic allograft nephropathy after renal transplantation: A protocol biopsy study. Kidney Int 67: 341–348, 2005 [DOI] [PubMed] [Google Scholar]
- 5.Pihlstrøm H, Dahle DO, Mjøen G, Pilz S, März W, Abedini S, Holme I, Fellström B, Jardine AG, Holdaas H: Increased risk of all-cause mortality and renal graft loss in stable renal transplant recipients with hyperparathyroidism. Transplantation 99: 351–359, 2015 [DOI] [PubMed] [Google Scholar]
- 6.Bleskestad IH, Bergrem H, Leivestad T, Hartmann A, Gøransson LG: Parathyroid hormone and clinical outcome in kidney transplant patients with optimal transplant function. Clin Transplant 28: 479–486, 2014 [DOI] [PubMed] [Google Scholar]
- 7.Kumar R, Thompson JR: The regulation of parathyroid hormone secretion and synthesis. J Am Soc Nephrol 22: 216–224, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Isaksson E, Sterner G: Early development of secondary hyperparathyroidism following renal transplantation. Nephron Clin Pract 121: c68–c72, 2012 [DOI] [PubMed] [Google Scholar]
- 9.Evenepoel P, Claes K, Kuypers D, Maes B, Bammens B, Vanrenterghem Y: Natural history of parathyroid function and calcium metabolism after kidney transplantation: A single-centre study. Nephrol Dial Transplant 19: 1281–1287, 2004 [DOI] [PubMed] [Google Scholar]
- 10.Roodnat JI, van Gurp EA, Mulder PG, van Gelder T, de Rijke YB, de Herder WW, Kal-van Gestel JA, Pols HA, Ijzermans JN, Weimar W: High pretransplant parathyroid hormone levels increase the risk for graft failure after renal transplantation. Transplantation 82: 362–367, 2006 [DOI] [PubMed] [Google Scholar]
- 11.Bhan I, Shah A, Holmes J, Isakova T, Gutierrez O, Burnett SM, Jüppner H, Wolf M: Post-transplant hypophosphatemia: Tertiary ‘Hyper-Phosphatoninism’? Kidney Int 70: 1486–1494, 2006 [DOI] [PubMed] [Google Scholar]
- 12.Mazzaferro S, Pasquali M, Taggi F, Baldinelli M, Conte C, Muci ML, Pirozzi N, Carbone I, Francone M, Pugliese F: Progression of coronary artery calcification in renal transplantation and the role of secondary hyperparathyroidism and inflammation. Clin J Am Soc Nephrol 4: 685–690, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Perrin P, Caillard S, Javier RM, Braun L, Heibel F, Borni-Duval C, Muller C, Olagne J, Moulin B: Persistent hyperparathyroidism is a major risk factor for fractures in the five years after kidney transplantation. Am J Transplant 13: 2653–2663, 2013 [DOI] [PubMed] [Google Scholar]
- 14.Courbebaisse M, Thervet E, Souberbielle JC, Zuber J, Eladari D, Martinez F, Mamzer-Bruneel MF, Urena P, Legendre C, Friedlander G, Prié D: Effects of vitamin D supplementation on the calcium-phosphate balance in renal transplant patients. Kidney Int 75: 646–651, 2009 [DOI] [PubMed] [Google Scholar]
- 15.Amer H, Griffin MD, Stegall MD, Cosio FG, Park WD, Kremers WK, Heilman RL, Mazur MJ, Hamawi K, Larson TS, Kumar R: Oral paricalcitol reduces the prevalence of posttransplant hyperparathyroidism: Results of an open label randomized trial. Am J Transplant 13: 1576–1585, 2013 [DOI] [PubMed] [Google Scholar]
- 16.Madorin C, Owen RP, Fraser WD, Pellitteri PK, Radbill B, Rinaldo A, Seethala RR, Shaha AR, Silver CE, Suh MY, Weinstein B, Ferlito A: The surgical management of renal hyperparathyroidism. Eur Arch Otorhinolaryngol 269: 1565–1576, 2012 [DOI] [PubMed] [Google Scholar]
- 17.Evenepoel P, Claes K, Kuypers DR, Debruyne F, Vanrenterghem Y: Parathyroidectomy after successful kidney transplantation: A single centre study. Nephrol Dial Transplant 22: 1730–1737, 2007 [DOI] [PubMed] [Google Scholar]
- 18.Torregrosa JV, Barros X: Management of hypercalcemia after renal transplantation. Nefrologia 33: 751–757, 2013 [DOI] [PubMed] [Google Scholar]
- 19.Block GA, Martin KJ, de Francisco AL, Turner SA, Avram MM, Suranyi MG, Hercz G, Cunningham J, Abu-Alfa AK, Messa P, Coyne DW, Locatelli F, Cohen RM, Evenepoel P, Moe SM, Fournier A, Braun J, McCary LC, Zani VJ, Olson KA, Drüeke TB, Goodman WG: Cinacalcet for secondary hyperparathyroidism in patients receiving hemodialysis. N Engl J Med 350: 1516–1525, 2004 [DOI] [PubMed] [Google Scholar]
- 20.Evenepoel P, Cooper K, Holdaas H, Messa P, Mourad G, Olgaard K, Rutkowski B, Schaefer H, Deng H, Torregrosa JV, Wuthrich RP, Yue S: A randomized study evaluating cinacalcet to treat hypercalcemia in renal transplant recipients with persistent hyperparathyroidism. Am J Transplant 14: 2545–2555, 2014 [DOI] [PubMed] [Google Scholar]
- 21.Colloton M, Shatzen E, Wiemann B, Starnes C, Scully S, Henley C, Martin D: Cinacalcet attenuates hypercalcemia observed in mice bearing either Rice H-500 Leydig cell or C26-DCT colon tumors. Eur J Pharmacol 712: 8–15, 2013 [DOI] [PubMed] [Google Scholar]
- 22.Coyne DW, Delos Santos R: Evaluating the safety and rationale for cinacalcet posttransplant hyperparathyroidism and hypercalcemia. Am J Transplant 14: 2446–2447, 2014 [DOI] [PubMed] [Google Scholar]
- 23.Guañabens N, Filella X, Monegal A, Gómez-Vaquero C, Bonet M, Buquet D, Casado E, Cerdá D, Erra A, Martinez S, Montalá N, Pitarch C, Kanterewicz E, Sala M, Surís X, Torres F; LabOscat Study Group: Reference intervals for bone turnover markers in Spanish premenopausal women [published online ahead of print June 18, 2015]. Clin Chem Lab Med 10.1515/cclm-2015-0162 [DOI] [PubMed] [Google Scholar]
- 24.Kalantar-Zadeh K, Molnar MZ, Kovesdy CP, Mucsi I, Bunnapradist S: Management of mineral and bone disorder after kidney transplantation. Curr Opin Nephrol Hypertens 21: 389–403, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cunningham J, Locatelli F, Rodriguez M: Secondary hyperparathyroidism: Pathogenesis, disease progression, and therapeutic options. Clin J Am Soc Nephrol 6: 913–921, 2011 [DOI] [PubMed] [Google Scholar]
- 26.Henschkowski J, Bischoff-Ferrari HA, Wüthrich RP, Serra AL: Renal function in patients treated with cinacalcet for persistent hyperparathyroidism after kidney transplantation. Kidney Blood Press Res 34: 97–103, 2011 [DOI] [PubMed] [Google Scholar]
- 27.Schwarz A, Rustien G, Merkel S, Radermacher J, Haller H: Decreased renal transplant function after parathyroidectomy. Nephrol Dial Transplant 22: 584–591, 2007 [DOI] [PubMed] [Google Scholar]
- 28.Gwinner W, Suppa S, Mengel M, Hoy L, Kreipe HH, Haller H, Schwarz A: Early calcification of renal allografts detected by protocol biopsies: Causes and clinical implications. Am J Transplant 5: 1934–1941, 2005 [DOI] [PubMed] [Google Scholar]
- 29.Ballinger AE, Palmer SC, Nistor I, Craig JC, Strippoli GF: Calcimimetics for secondary hyperparathyroidism in chronic kidney disease patients. Cochrane Database Syst Rev 12: CD006254, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ishani A, Liu J, Wetmore JB, Lowe KA, Do T, Bradbury BD, Block GA, Collins AJ: Clinical outcomes after parathyroidectomy in a nationwide cohort of patients on hemodialysis. Clin J Am Soc Nephrol 10: 90–97, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Costa-Hong V, Jorgetti V, Gowdak LH, Moyses RM, Krieger EM, De Lima JJ: Parathyroidectomy reduces cardiovascular events and mortality in renal hyperparathyroidism. Surgery 142: 699–703, 2007 [DOI] [PubMed] [Google Scholar]
- 32.Komaba H, Taniguchi M, Wada A, Iseki K, Tsubakihara Y, Fukagawa M: Parathyroidectomy and survival among Japanese hemodialysis patients with secondary hyperparathyroidism. Kidney Int 88: 350–359, 2015 [DOI] [PubMed] [Google Scholar]
- 33.Narayan R, Perkins RM, Berbano EP, Yuan CM, Neff RT, Sawyers ES, Yeo FE, Vidal-Trecan GM, Abbott KC: Parathyroidectomy versus cinacalcet hydrochloride-based medical therapy in the management of hyperparathyroidism in ESRD: A cost utility analysis. Am J Kidney Dis 49: 801–813, 2007 [DOI] [PubMed] [Google Scholar]
- 34.Borchhardt K, Sulzbacher I, Benesch T, Födinger M, Sunder-Plassmann G, Haas M: Low-turnover bone disease in hypercalcemic hyperparathyroidism after kidney transplantation. Am J Transplant 7: 2515–2521, 2007 [DOI] [PubMed] [Google Scholar]
- 35.Lebastchi AH, Donovan PI, Udelsman R: Paradigm shift in the surgical management of multigland parathyroid hyperplasia: An individualized approach. JAMA Surg 149: 1133–1137, 2014 [DOI] [PubMed] [Google Scholar]