Abstract
AIM
To investigate factors associated with breastfeeding duration (BD) in a sample of mothers living in Greece.
METHODS
Four hundred and twenty-eight mothers (438 infants) were initially recruited in a tertiary University Hospital. Monthly telephone interviews (1665 in total) using a structured questionnaire (one for each infant) were conducted until the sixth postpartum month. Cox regression analysis was used to assess factors influencing any BD.
RESULTS
Any breastfeeding rates in the first, third, and sixth month of the infant’s life reached 87.5%, 57.0% and 38.75%, respectively. In the multivariate analysis, maternal smoking in the lactation period [hazard-ratio (HR) = 4.20] and psychological status (HR = 1.72), and the introduction of a pacifier (HR = 2.08), were inversely associated, while higher maternal education (HRuniversity/college vs primary/high school = 0.53, HRmaster’s vs primary/high school = 0.20), and being an immigrant (HR = 0.35) were positively associated with BD.
CONCLUSION
Public health interventions should focus on campaigns against smoking during lactation, target women of lower educational status, and endorse the delayed introduction of pacifiers.
Keywords: Breastfeeding, Exclusive, Formula feeding, Duration, Greece
Core tip: This was a prospective study investigating the factors which are associated with breastfeeding duration (BD) in a sample of mothers living in Greece. Maternal smoking during lactation, the respective psychological status, and the introduction of a pacifier, were inversely associated, while higher maternal education and maternal immigrant status positively associated with BD. Public health interventions should focus on campaigns against smoking during lactation, target women of lower educational status, and endorse the delayed introduction of pacifiers.
INTRODUCTION
Breastfeeding is the natural way to feed infants and young children ensuring optimal growth and development[1-5], while exclusive breastfeeding is recommended for the first six months of life[5]. Nevertheless, breastfeeding is not fully protected and supported as expected, and a number of important international public health initiatives were endorsed by the World Health Organization and United Nations International Children's Emergency Fund in order to protect and support breastfeeding[6-8].
Although some slight improvements have been recorded in breastfeeding rates during the last decade, they continue to fall short of global recommendations, and many mothers, who initially chose to breastfeed, shift to formula-feeding, and finally cease breastfeeding[9-12].
A variety of factors influence and determine breastfeeding initiation and duration, including personal and socio-cultural characteristics of the mother, the child and the family, aspects of the health care system, public health and social policies, as well as advertising and promotion of alternative feeding methods[13]. Some of these factors, such as maternal education and employment, may act on the opposite direction in different populations[11]. The identification of the determinants that influence breastfeeding duration (BD) across countries may provide useful information, which could be used to improve breastfeeding rates at national levels and worldwide.
The aim of the present study is to investigate the factors which are associated with BD in a sample of mothers living in Greece, a typical Southern European country, and explore further how modifiable these factors are.
MATERIALS AND METHODS
Study population and data collection at baseline
Four hundred and twenty-eight mothers, who had given birth to 438 live infants, were recruited in the maternity ward of a tertiary University Hospital between February and December 2009. The hospital provides gynaecological and maternity services to women residing in the Prefecture of Attica, where the capital of Greece, Athens is located, and monitoring of high-risk pregnancies at a nationwide level.
The study design and characteristics of the study population have been described in more detail elsewhere[14]. In brief, during the aforementioned 10-mo period, women, who had delivered a child and were permanent inhabitants of Greece with basic understanding of the Greek language, were approached by the first author after 24 h from delivery, and asked to participate in the study. The mothers were expected to be in good condition to withstand an interview at that time, taking also into account that the average nationwide in-patient stay in the maternity ward is four days.
The study protocol was approved by the Ethics Committee of the Medical School of University of Athens. All participants were asked to sign an informed consent form before being enrolled in the study.
At recruitment, baseline information about medical, lactation-related, and socio-demographic characteristics was collected through a structured baseline questionnaire, by means of an interview conducted by the first author. The baseline questionnaire consisted of five sections: (1) a section associated with the lactation status of the specific newborn/s (seven items); (2) a section associated with the gestation/childbirth of the specific newborn/s (eight items); (3) a section related to the past medical/gynaecological history of the mother (two items); (4) a section for general information (three items); and (5) socio-economic characteristics (12 items).
The selection of the variables included in each section was based on prior knowledge derived from respective studies which had investigated a similar research hypothesis, as well as on our intention to explore further the respective parameters in the Greek setting. The questionnaire included both open-ended and closed questions and the baseline interviews typically lasted for about 30 min. Pre-pregnancy body weight and height were self-reported.
Data collection during follow-up
Telephone interviews for the collection of information about the duration of breastfeeding and/or alternative feeding methods were conducted by the first author with the use of an itemized follow-up questionnaire. The respective phone calls were made every month during the first six months following the child’s birth. In total, 1665 interviews took place within a 14-mo period. The first interview wave involved 400 infants yielding a participation rate of 91.3%.
The follow-up questionnaire, consisting of closed-ended questions, collected information which was grouped in the following sections: (1) topics relating to the infant (number of items 5); (2) issues associated with the mother (number of items 7); (3) approaches of health professionals (number of items 1); and (4) alterations influenced by social/economic factors (number of items 4). The duration of the follow-up interview was approximately 15 min.
Infant feeding definitions
Exclusive breastfeeding comprised of giving breastmilk (or expressed breastmilk) only to the infant, precluding the use of any other liquid or solid food, except vitamin syrups/drops, medication, or mineral supplements. Formula-fed babies were given liquid food from a bottle with a nipple/teat, while no breastmilk was provided[15]. Any other combination of breastmilk with formula and/or additional liquids, or the administration of food and food-based fluids (such as weaning foods) was classified as partial breastfeeding[16].
A mother was considered to be continuing either exclusive or partial breastfeeding when she replied positively to the respective question, during the follow-up phone call.
Statistical analysis
Initial analysis included descriptive statistics. Categorical variables are presented as relative and absolute frequencies. The main variable of interest was BD (exclusive and partial together, henceforth referred as any breastfeeding). BD is a quantitative variable demonstrating right censoring. We employed Cox proportional hazard models to explore the parameters which were associated with any BD, after ascertaining that the respective prerequisite assumptions were met. Univariate models were initially run, in order to detect any potential association between BD (in weeks) and each of the covariates of interest. Potential confounding was addressed with the use of multivariate models. The final multivariate model included all covariates demonstrating a P value of less than 0.1 in the univariate analysis, as well as, a small set of covariates inserted in the model based on prior knowledge from the pertinent literature. These covariates comprised the age of the mother, the pre-pregnancy body mass index (BMI), and the employment status. Maternal age was additionally tested for correlation with the period of active lactation by applying Spearman’s correlation coefficient. Pre-pregnancy BMI was calculated by dividing the weight of the mother (in kilogram) by the square height (in meters).
Available data were processed by using the IBM SPSS Statistics 21.0. Statistical importance was accepted at a level of 0.05 and lower.
RESULTS
Approximately 70% of recruited mothers had Greek nationality, while the mean age was 32 years (min 19, max 44) (Table 1). A high percentage of the mothers were university or college graduates (54.4%) and employed (73.4%). The vast majority of mothers were also married. The mean maternal BMI was 23.4 kg/m2 at the beginning of gestation and 28.6 kg/m2 before delivery. Almost one third of the mothers (30.8%) were smokers before pregnancy. Previous breastfeeding experience was reported in 44.5% of women, whilst the present birth was the first in 50.0% of recruited mothers.
Table 1.
Main socio-demographic characteristics of the mothers at recruitment
| Characteristics | % (n) |
| Maternal age | |
| Mean (SD)1 | 32.0 (4.7) |
| Country of origin | |
| Greece | 71.0 (304) |
| Other | 29.0 (124) |
| Marital status2 | |
| Married | 96.2 (403) |
| Not married | 3.8 (16) |
| Educational status | |
| Primary school | 1.8 (8) |
| Secondary/high school | 37.0 (158) |
| University/college | 54.4 (233) |
| Postgraduate studies | 6.8 (29) |
| Employment status3 | |
| Employed | 73.4 (311) |
| Public sector | 18.6 (79) |
| Private sector | 45.1 (191) |
| Self-employed | 7.8 (33) |
| Other | 1.9 (8) |
| Domestically occupied | 20.5 (87) |
| Unemployed | 6.1 (26) |
In years;
Missing cases n = 9;
Missing cases n = 4. n: Absolute numbers.
With regard to baseline characteristics related to the infant (Table 2), the percentage of babies being delivered via caesarean section was remarkably high (51.0% of all deliveries), although in most cases the reason was a previous caesarean. The majority of infants were full-term (91.0%), had normal birth weight (94.0%), and were born without any health problem (80.5%). A far as the maternity hospital practices were concerned, rooming-in was implemented in 47.0% of newborns and breastfeeding was encouraged by health professionals and/or family in 89.7% of them.
Table 2.
Characteristics of the infant population at recruitment
| Characteristics | % (n) |
| Gender | |
| Female | 45.7 (200) |
| Male | 54.3 (238) |
| Birth weight | |
| Mean (SD)1 | 3215 (493) |
| Delivery mode | |
| Vaginal delivery | 49.0 (218) |
| Caesarean section | 51.0 (220) |
| Multiplicity | |
| Singletons | 95.4 (418) |
| Twins | 4.6 (20) |
| Prematurity (< 37 wk) | |
| No | 91.0 (399) |
| Yes | 9.0 (39) |
| Newborn health problems2 | |
| No | 80.5 (350) |
| Yes | 19.5 (86) |
In grams;
Missing cases n = 2. n: Absolute numbers.
Any breastfeeding initiation rate was high (92.1%), while almost half of the mothers (44.4%) practiced exclusively breastfeeding. Any breastfeeding rates were 87.5% for the first, 57.0% for the third and 38.8% for the sixth postpartum month. Exclusive breastfeeding at the first, third and six month reached 43.5%, 34.0% and 24.5%, respectively (Table 3). The percentages of formula-feeding were 12.5%, 36.5% and 57.3%, for the aforementioned monthly periods, respectively. With respect to BD, the mean duration was 15.3 (± 8.6, min 1 and max 24) wk.
Table 3.
Partial and exclusive breastfeeding rates during the follow-up period by postpartum month
| Postpartum month | Partial breastfeeding n1 (%) | Exclusive breastfeeding n (%) |
| 1 | 175 (43.75) | 174 (43.50) |
| 2 | 125 (31.25) | 154 (38.50) |
| 3 | 92 (23.00) | 136 (34.00) |
| 4 | 75 (18.75) | 118 (29.50) |
| 5 | 58 (14.50) | 106 (26.50) |
| 6 | 57 (14.25) | 98 (24.50) |
Absolute numbers.
Commonly reported problems which led to breastfeeding discontinuation are shown in Table 4. Almost half of the mothers (48.5%), who stopped breastfeeding, reported that the main reason for the cessation of breastfeeding was the production of inadequate milk volume. In addition, a noteworthy percentage of mothers reported “other” (29.3%) (i.e., fatigue, ablactation, general breastfeeding problems), or “other medical” (13.5%) (i.e., health problems of the infant, maternal health problems, medications received by the mother) reasons for breastfeeding cessation.
Table 4.
Reasons for breastfeeding cessation in the postpartum period as reported by mothers (percentages only refer to mothers who have stopped breastfeeding)
| Reason for breastfeeding cessation | Percentage of mothers (%) |
| Not enough milk | 48.5 |
| Other1 | 29.3 |
| Other medical reason2 | 13.5 |
| Return to work | 4.2 |
| Sore/traumatized nipples | 2.4 |
| Mastitis | 1.5 |
| Obstructed mammary ducts | 0.6 |
Includes fatigue, ablactation, general breastfeeding problems;
Includes health problems of the infant, maternal health problems, medications received by the mother.
Exclusive breastfeeding percentage is also presented, as it evolves during the follow-up period, when the monthly samples of the interviewed mothers are examined individually (i.e., a given sample of mothers who continue to breastfeed is compared to the previous or the next interview). The progress of exclusive breastfeeding for each monthly sample is depicted in Figure 1. The percentage of exclusively breastfed babies in the overall population of breastfed babies of each monthly interview was, hence, noted. Exclusive breastfeeding practice, when studied under this approach, demonstrated an increasing trend throughout follow-up, up until the fifth postpartum month (saturation period), after which the respective rates started to fall (Figure 1).
Figure 1.
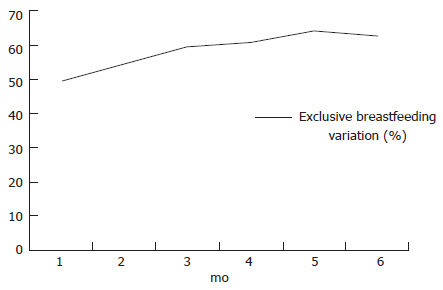
Exclusive breastfeeding evolvement during the postpartum period (monthly samples).
Table 5 presents the fully adjusted Cox regression-derived hazard ratios for any BD by specific characteristics of the mother or the infant. Mothers who smoked during the follow-up period were 4.2 times more likely (95%CI: 2.57-6.89) to stop breastfeeding earlier within the first 6 mo after delivery, compared to women who did not smoke during follow-up (P < 0.001). On the other hand, maternal smoking before pregnancy was not associated with any BD (P = 0.124) in the multivariate analysis, in contrast to the results of the univariate analysis, where it was found to be inversely associated (HR = 2.16, 95%CI: 1.67-2.80) (data not shown).
Table 5.
Adjusted hazard ratios and 95%CI for any breastfeeding duration
| Characteristic | HR | 95%CI | P value |
| Maternal age (per year) | 1.01 | 0.97 to 1.05 | P = 0.779 |
| BMI before pregnancy (per kg/m2) | 1.01 | 0.97 to 1.05 | P = 0.600 |
| Maternal educational status | |||
| High school graduate or lower | 1.00 | ||
| University/college education | 0.53 | 0.37 to 0.76 | P = 0.001 |
| Postgraduate degree | 0.20 | 0.09 to 0.43 | P < 0.001 |
| Maternal employment status | |||
| Unemployed/domestically occupied | 1.00 | P = 0.213 | |
| Employed | 0.76 | 0.50 to 1.17 | |
| Maternal nationality | |||
| Greek | 1.00 | ||
| Immigrant | 0.35 | 0.21 to 0.38 | P < 0.001 |
| Smoking before pregnancy | |||
| No | 1.00 | ||
| Yes | 0.49 | 0.20 to 1.22 | P = 0.124 |
| Smoking during follow-up | |||
| No | 1.00 | ||
| Yes | 4.20 | 2.57 to 6.89 | P < 0.001 |
| Maternal psychological problems | |||
| No | 1.00 | ||
| Yes | 1.72 | 1.23 to 2.41 | P = 0.002 |
| Previous breastfeeding experience | |||
| No | 1.00 | P = 0.069 | |
| Yes | 0.69 | 0.46 to 1.03 | |
| Breastfeeding encouragement | |||
| No | 1.00 | ||
| Yes | 0.98 | 0.60 to 1.58 | P = 0.916 |
| Multiparity | |||
| Singleton | 1.00 | ||
| Twins | 1.83 | 0.89 to 3.74 | P = 0.099 |
| Prematurity | |||
| Full-term | 1.00 | P = 0.088 | |
| Premature | 1.65 | 0.93 to 2.93 | |
| Pacifier introduction | |||
| No | 1.00 | ||
| Yes | 2.08 | 1.40 to 3.08 | P < 0.001 |
The nationality of the mother was found to be important, as immigrant mothers had 0.35 times (95%CI: 0.21-0.58) less chance for earlier breastfeeding discontinuation in comparison with Greek mothers (P < 0.001).
A similar trend was observed regarding the maternal educational status. In addition to having a postgraduate study degree (P < 0.001), which had also been identified as important in the univariate analysis, increased duration of any breastfeeding was also found to be more likely among university/college graduates, compared to mandatory education and high school graduates (P = 0.001). Indeed, having a university/college diploma was associated with a lower risk of earlier breastfeeding cessation (HR = 0.53, 95%CI: 0.37-0.76), and having a postgraduate study degree with an even lower risk of earlier weaning (HR = 0.20, 95%CI: 0.09-0.43), compared with mandatory or high school education.
The psychological status of the mother, reflecting the prevalence of related psychological problems postpartum (including swinging mood, easy change of disposition, bad disposition, anxiety, and easy crying), was inversely associated with the duration of any breastfeeding (P = 0.002). The presence of such problems carried a 1.72 (95%CI: 1.23-2.41) times higher risk of earlier breastfeeding cessation.
Finally, the use of a pacifier was found to affect any BD in a negative manner (P < 0.001, HR = 2.08, 95%CI: 1.40-3.08), a result also observed in the univariate analysis (HR = 2.87, 95%CI: 2.05-4.00).
Previous breastfeeding experience and lack of home support, immigrant status of the father, and low birth weight/prematurity, or multiplicity of the newborns, although found significant in the univariate analysis, did not remain significant in the final multivariate model. In addition, maternal age was neither associated with the duration of breastfeeding in the univariate analysis (P = 0.689), nor was it correlated with the period of active lactation after applying Spearman’s correlation coefficient (ρ = 0.013, P = 0.783).
DISCUSSION
The present study sample comprising mothers, who were recruited in a maternity ward of a tertiary University Hospital, indicated that maternal smoking during the postpartum period was associated with higher risk for the cessation of any breastfeeding, whereas maternal education and immigrant status were positively associated with increased duration of any breastfeeding. The adverse maternal psychological status and the introduction of a pacifier affected the continuation of any breastfeeding in a negative manner.
The initiation of any breastfeeding among the interviewed mothers was high, with almost half of them practicing exclusive breastfeeding. Any breastfeeding rates gradually declined during the follow-up period, reaching 38.75% at the sixth postpartum month, while exclusive breastfeeding exhibited a similar trend and was practiced by the one quarter of the study sample at the sixth postpartum month.
It is interesting to note however, that if we examine each monthly sample of interviewed mothers separately as they evolve during the follow-up period, the progress of exclusive breastfeeding rate for each sample demonstrates an increasing trend throughout the follow-up period, up until the fifth postpartum month (saturation period), after which the respective rates started to fall (Figure 1). That means, in effect, that every month until the fifth postpartum month, the proportion of exclusively breastfed babies in the remaining population increased. In other words, more babies who were partially breastfeeding stop being breastfed, compared to their exclusively breastfed counterparts, from the first until the fifth postpartum month (Table 3). This, in turn, might suggest that promoting exclusive breastfeeding may be a good strategy to avoid early weaning.
Exclusive and any BD rates were also reported in previous Greek studies, but the respective percentages were lower[17-19]. The lack of breastfeeding-friendly hospital practices has been consistently identified as detrimental for BD[18,19]. However, Bakoula et al[18] concluded that women in Greece seemed capable of overcoming formula supplementation in the hospital environment and could revert to exclusive breastfeeding at home. Hence, it can be postulated that mothers, who choose to continue breastfeeding in this study, possess the determination to overcome the related obstacles. The finding that any BD was not affected by previous information about breastfeeding, maternal employment status, or paid leave of absence, may, therefore, not be unrelated.
It should also be mentioned that the majority of mothers in the present study (48.5%) reported that the main reason for the cessation of breastfeeding was the production of inadequate milk volume. This belief is erroneous from a scientific point of view, as various studies have determined that less than 5% mothers do not seem able to meet the goals regarding the appropriate weight gain of their infant, because of inadequate milk production[20-23]. Thus, the length of BD may further increase, if mothers receive appropriate guidance from health professionals[24].
Drawing on the factors, which positively influenced the continuation of any breastfeeding, higher educational level of the mother was positively associated with BD. University/college graduates had about half the risk of premature weaning during the first six months, compared to mandatory education and high school graduates, whereas Master degree holders less than one fifth of that risk. Similar findings were reported by Flacking et al[25] in a prospective population-based cohort study in Sweden. Mothers of term infants with mandatory or upper secondary education in that study had more than twice the risk of premature discontinuation of breastfeeding within the first six postpartum months, compared with mothers of higher educational level. It should be mentioned that the educational level measured in the present analysis was the level of formal education, rather than education about breastfeeding. Further research might discern which aspects of maternal education play the most important role in breastfeeding, and such information may be used in school educational programs.
Immigrant mothers were also more likely to demonstrate increased duration of any breastfeeding. This finding has been previously reported in multi-cultural societies (i.e., United States, United Kingdom), in which lower breastfeeding rates were consistently associated with acculturation[26-29]. It is possible that the association identified in this study, reflects the fact that immigrant mothers in Southern Europe come from families and communities, where breastfeeding is by far the predominant infant feeding method[30]. Moreover, even in societies with multi-cultural backgrounds there seems to be a stark contrast in of breastfeeding by ethnicity[26,27], which, in turn, suggests that different public health approaches need to be adopted in order to increase BD. In contrast, paternal immigrant status was not found to be significant in this study.
Focusing on the factors which adversely affected the continuation of any breastfeeding, smoking during follow-up was found to be important. In particular, mothers who reverted to regular smoking after delivery had a fourfold risk of stopping breastfeeding earlier within the first 6 postpartum months, compared to women who did not smoke. An early weaning risk of similar magnitude was also reported by Rattner et al[31] in a secondary analysis of data from a randomized controlled trial involving 228 women, who had stopped smoking before pregnancy, but reverted to daily smoking thereafter. In contrast, in a retrospective questionnaire-based national survey of a random sample of 24438 Norwegian women, Haug et al[32] reported that women who did not smoke were twice as likely to continue to breastfeed at 6 mo, compared with women who smoked. In addition, the adjusted odds ratio for breastfeeding continuation of more than 6 mo in women who had stopped smoking in pregnancy was 3.7 in the study of Giglia et al[33]. Further to the potential biological mechanisms associated with smoking and lactation[34-36], women who smoke may wean prematurely because of being unsure whether it is still safe to breastfeed. These women may be reluctant to seek the advice of health professionals, or even help for breastfeeding problems, as they could be wary of their reactions[37].
The adverse psychological status of the mother during the first postpartum month proved significant and affected the duration of any breastfeeding in a negative manner. The related postpartum problems which were examined included swinging mood, easy change of disposition, bad disposition, anxiety, and easy crying. As a whole the appearance of such problems postpartum carried a 1.72 times higher risk of earlier breastfeeding cessation. Hence, not only true depression, but also other forms of postnatal distress seem to influence the duration of breastfeeding, and timely identification and intimate knowledge of these factors could assist in recognizing women at risk for early weaning, and constructing programs capable of increasing the length of BD. The importance of psychological factors in predicting BD was also stressed in the study of O’Brien et al[38].
The introduction of a pacifier was found to negatively affect the duration of any breastfeeding. Similar results were reported by Howard et al[39], who had associated the introduction of a pacifier by the sixth week with a significant decline in BD, in a prospective cohort study of 265 breastfeeding mother-infant dyads. However, the duration of breastfeeding up to 3 mo was not affected by the early introduction of a pacifier in that study. In addition, Scott et al[40], in a prospective study of 587 Australian mothers, found that the introduction of a pacifier after 10 wk did not significantly affect the duration of breastfeeding, whilst its use in the first 10 wk increased the risk for the cessation of full breastfeeding by 6 mo and overall breastfeeding by 12 mo. It has been suggested that the decreases in BD associated with pacifier use may be a consequence of less frequent breastfeeding among women who introduce pacifiers to their infants[27]. The reasons for introducing a pacifier in the first place need to be determined. There is also a need to determine whether breastfeeding problems associated with the use of pacifiers precede or follow their introduction. In the former case women need to be advised on how to prevent, identify, and manage breastfeeding problems, as a means of reducing the need for the use of pacifiers. In the latter case, however, women need to be discouraged from introducing pacifiers in order to reduce the risk of breastfeeding problems, and increase the duration of breastfeeding[28].
Limitations
The present study was conducted in a single-centre setting, which may result to the study sample not being strictly representative of the Greek population. Nevertheless, the study population was recruited in the maternity ward of a tertiary University hospital, which is not only serving the Prefecture of Attica, but also accepting referrals of high-risk pregnancies from the entire Greek territory. Hence, the validity of the associations found between BD and various factors under study is not likely to have been affected.
In conclusion, the results of the present study revealed the importance of maternal education and immigrant status regarding the duration of any breastfeeding. In addition, maternal smoking during lactation, as well as the use of a pacifier, were inversely associated with the duration of any breastfeeding. Post-partum psychological status was also found to be inversely associated with any BD in this study sample.
Public health interventions in order to protect, support and promote breastfeeding should include campaigns against smoking during lactation, as a means of increasing BD, as well as, endorsing the delayed introduction of pacifiers. Interventions should also focus on women of low educational status, which obviously consist a high risk group for early breastfeeding cessation.
Findings of this study could also prove useful for comparing factors which are responsible for BD across countries, and providing information that could be used as a tool for the promotion of practices and programs that encourage breastfeeding.
It is becoming increasingly important that public health authorities and health professionals need to identify the factors that influence BD across countries, and aim at creating socio-cultural and economic settings that encourage the continuation of breastfeeding.
COMMENTS
Background
Breastfeeding is the natural way to feed infants and young children ensuring optimal growth and development, while exclusive breastfeeding is recommended for the first six months of life. Although some slight improvements have been recorded in breastfeeding rates during the last decade, they continue to fall short of global recommendations, and many mothers, who initially chose to breastfeed, shift to formula-feeding, and finally cease breastfeeding. A variety of factors influence and determine breastfeeding initiation and duration, including characteristics of the mother, the child and the family, aspects of the health care system, public health and social policies, advertising and promotion of alternative feeding methods. The identification of the determinants that influence breastfeeding duration (BD) across countries may provide useful information, which could be used to improve breastfeeding rates at national levels and worldwide.
Research frontiers
Maternal smoking during the postpartum period is associated with higher risk for earlier breastfeeding discontinuation, as also the adverse maternal psychological status and the early introduction of a pacifier to the infant. Maternal education and immigrant status, on the other hand, are positively associated with increased BD.
Innovations and breakthroughs
In the present study, the authors additionally examined each monthly sample of interviewed mothers separately, as they evolved during the follow-up period. The progress of exclusive breastfeeding rate for each sample demonstrated an increasing trend throughout the follow-up period, up until the fifth postpartum month (saturation period), after which the respective rates started to fall. That means, in effect, that every month until the fifth postpartum month, the proportion of exclusively breastfed babies in the remaining population increased. In other words, more babies who were partially breastfeeding stop being breastfed, compared to their exclusively breastfed counterparts, from the first until the fifth postpartum month. This, in turn, might suggest that promoting exclusive breastfeeding may be a good strategy to avoid early weaning.
Applications
Public health interventions in order to protect, support and promote breastfeeding should include campaigns against smoking during lactation, as a means of increasing BD, as well as, endorsing the delayed introduction of pacifiers. Interventions should also focus on women of low educational status, which obviously consist a high risk group for early breastfeeding cessation. Findings of this study could also prove useful for comparing factors which are responsible for BD across countries, and providing information that could be used as a tool for the promotion of practices and programs that encourage breastfeeding.
Peer-review
In this paper, authors investigated factors associated with BD in a sample of mothers living in Greece. The results of the present study revealed the importance of maternal education and immigrant status regarding the duration of any breastfeeding. Furthermore, authors also found that maternal smoking during lactation and the use of a pacifier, were inversely associated with the duration of any breastfeeding. This is a well written and well conducted study.
Footnotes
Institutional review board statement: The study protocol was approved by the Ethics Committee of the Medical School of the University of Athens.
Clinical trial registration statement: None.
Informed consent statement: All participants were asked to sign an informed consent form before being enrolled in the study.
Conflict-of-interest statement: The authors of this manuscript having no conflicts of interest to disclose. The authors have no financial interests, and have not received any financial support for this article.
Data sharing statement: There is no additional data available.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Manuscript source: Invited manuscript
Specialty type: Pediatrics
Country of origin: Greece
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
Peer-review started: February 1, 2016
First decision: March 21, 2016
Article in press: June 3, 2016
P- Reviewer: Bártová E, Ji Y, Khajehei M, Langdon S, Wang S S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
References
- 1.Binns C, Lee M, Low WY. The Long-Term Public Health Benefits of Breastfeeding. Asia Pac J Public Health. 2016;28:7–14. doi: 10.1177/1010539515624964. [DOI] [PubMed] [Google Scholar]
- 2.Victora CG, Bahl R, Barros AJ, França GV, Horton S, Krasevec J, Murch S, Sankar MJ, Walker N, Rollins NC. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. 2016;387:475–490. doi: 10.1016/S0140-6736(15)01024-7. [DOI] [PubMed] [Google Scholar]
- 3.Davanzo R, Romagnoli C, Corsello G. Position Statement on Breastfeeding from the Italian Pediatric Societies. Ital J Pediatr. 2015;41:80. doi: 10.1186/s13052-015-0191-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Section on Breastfeeding. Breastfeeding and the use of human milk. Pediatrics. 2012;129:e827–e841. doi: 10.1542/peds.2011-3552. [DOI] [PubMed] [Google Scholar]
- 5.WHO/UNICEF. Global strategy for infant and young child feeding. Geneva: Switzerland; 2003. [Google Scholar]
- 6.World Health Assembly. International Code of Marketing of Breastmilk Substitutes. Geneva: WHO; 1981. [Google Scholar]
- 7.WHO/UNICEF. Breastfeeding in the 1990’s: A global initiative meeting in Florence, Italy and New York. Geneva: Switzerland; 1990. Innocenti declaration on the protection, promotion, and support of breastfeeding. [Google Scholar]
- 8.WHO/UNICEF. Baby-Friendly Hospital Initiative and program manual. Geneva: Switzerland; 1992. [Google Scholar]
- 9.Radzyminski S, Callister LC. Mother’s Beliefs, Attitudes, and Decision Making Related to Infant Feeding Choices. J Perinat Educ. 2016;25:18–28. doi: 10.1891/1058-1243.25.1.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Daly A, Pollard CM, Phillips M, Binns CW. Benefits, barriers and enablers of breastfeeding: factor analysis of population perceptions in Western Australia. PLoS One. 2014;9:e88204. doi: 10.1371/journal.pone.0088204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cattaneo A, Burmaz T, Arendt M, Nilsson I, Mikiel-Kostyra K, Kondrate I, Communal MJ, Massart C, Chapin E, Fallon M. Protection, promotion and support of breast-feeding in Europe: progress from 2002 to 2007. Public Health Nutr. 2010;13:751–759. doi: 10.1017/S1368980009991844. [DOI] [PubMed] [Google Scholar]
- 12.Hannula L, Kaunonen M, Tarkka MT. A systematic review of professional support interventions for breastfeeding. J Clin Nurs. 2008;17:1132–1143. doi: 10.1111/j.1365-2702.2007.02239.x. [DOI] [PubMed] [Google Scholar]
- 13.Peters E, Wehkamp KH, Felberbaum RE, Krüger D, Linder R. Breastfeeding duration is determined by only a few factors. Eur J Public Health. 2006;16:162–167. doi: 10.1093/eurpub/cki199. [DOI] [PubMed] [Google Scholar]
- 14.Tavoulari EF, Benetou V, Vlastarakos PV, Andriopoulou E, Kreatsas G, Linos A. Factors affecting breast-feeding initiation in Greece: What is important? Midwifery. 2015;31:323–331. doi: 10.1016/j.midw.2014.10.006. [DOI] [PubMed] [Google Scholar]
- 15.World Health Organization. Division of child health and development. Indicators for assessing breastfeeding practices. Reprinted report of an informal meeting. Switzerland: Geneva; 1991. [Google Scholar]
- 16.UNICEF UK. How to implement baby friendly standards. A guide for maternity settings. UK: London; 2011. [Google Scholar]
- 17.Vassilaki M, Chatzi L, Bagkeris E, Papadopoulou E, Karachaliou M, Koutis A, Philalithis A, Kogevinas M. Smoking and caesarean deliveries: major negative predictors for breastfeeding in the mother-child cohort in Crete, Greece (Rhea study) Matern Child Nutr. 2014;10:335–346. doi: 10.1111/j.1740-8709.2012.00420.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bakoula C, Nicolaidou P, Veltsista A, Prezerakou A, Moustaki M, Kavadias G, Lazaris D, Fretzayas A, Krikos X, Karpathios T, et al. Does exclusive breastfeeding increase after hospital discharge? A Greek study. J Hum Lact. 2007;23:165–173; quiz 174-178. doi: 10.1177/0890334407300384. [DOI] [PubMed] [Google Scholar]
- 19.Theofilogiannakou M, Skouroliakou M, Gounaris A, Panagiotakos D, Markantonis SL. Breast-feeding in Athens, Greece: factors associated with its initiation and duration. J Pediatr Gastroenterol Nutr. 2006;43:379–384. doi: 10.1097/01.mpg.0000228104.97078.bb. [DOI] [PubMed] [Google Scholar]
- 20.Khanal V, da Cruz JL, Karkee R, Lee AH. Factors associated with exclusive breastfeeding in Timor-Leste: findings from Demographic and Health Survey 2009-2010. Nutrients. 2014;6:1691–1700. doi: 10.3390/nu6041691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yarnoff BO, Allaire BT, Detzel P. Associations between Infant Feeding Practices and Length, Weight, and Disease in Developing Countries. Front Pediatr. 2013;1:21. doi: 10.3389/fped.2013.00021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dewey KG, Heinig MJ, Nommsen LA, Lönnerdal B. Adequacy of energy intake among breast-fed infants in the DARLING study: relationships to growth velocity, morbidity, and activity levels. Davis Area Research on Lactation, Infant Nutrition and Growth. J Pediatr. 1991;119:538–547. doi: 10.1016/s0022-3476(05)82401-1. [DOI] [PubMed] [Google Scholar]
- 23.Neville MC, Keller R, Seacat J, Lutes V, Neifert M, Casey C, Allen J, Archer P. Studies in human lactation: milk volumes in lactating women during the onset of lactation and full lactation. Am J Clin Nutr. 1988;48:1375–1386. doi: 10.1093/ajcn/48.6.1375. [DOI] [PubMed] [Google Scholar]
- 24.Li R, Fein SB, Chen J, Grummer-Strawn LM. Why mothers stop breastfeeding: mothers’ self-reported reasons for stopping during the first year. Pediatrics. 2008;122 Suppl 2:S69–S76. doi: 10.1542/peds.2008-1315i. [DOI] [PubMed] [Google Scholar]
- 25.Flacking R, Nyqvist KH, Ewald U. Effects of socioeconomic status on breastfeeding duration in mothers of preterm and term infants. Eur J Public Health. 2007;17:579–584. doi: 10.1093/eurpub/ckm019. [DOI] [PubMed] [Google Scholar]
- 26.Singh GK, Kogan MD, Dee DL. Nativity/immigrant status, race/ethnicity, and socioeconomic determinants of breastfeeding initiation and duration in the United States, 2003. Pediatrics. 2007;119 Suppl 1:S38–S46. doi: 10.1542/peds.2006-2089G. [DOI] [PubMed] [Google Scholar]
- 27.Kelly YJ, Watt RG, Nazroo JY. Racial/ethnic differences in breastfeeding initiation and continuation in the United kingdom and comparison with findings in the United States. Pediatrics. 2006;118:e1428–e1435. doi: 10.1542/peds.2006-0714. [DOI] [PubMed] [Google Scholar]
- 28.Merewood A. Race, ethnicity, and breastfeeding. Pediatrics. 2006;118:1742–1743. doi: 10.1542/peds.2006-2161. [DOI] [PubMed] [Google Scholar]
- 29.Gibson-Davis CM, Brooks-Gunn J. Couples’ immigration status and ethnicity as determinants of breastfeeding. Am J Public Health. 2006;96:641–646. doi: 10.2105/AJPH.2005.064840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tavoulari EF, Benetou V, Vlastarakos PV, Kreatsas G, Linos A. Immigrant status as important determinant of breastfeeding practice in southern Europe. Cent Eur J Public Health. 2015;23:39–44. doi: 10.21101/cejph.a4092. [DOI] [PubMed] [Google Scholar]
- 31.Ratner PA, Johnson JL, Bottorff JL. Smoking relapse and early weaning among postpartum women: is there an association? Birth. 1999;26:76–82. doi: 10.1046/j.1523-536x.1999.00076.x. [DOI] [PubMed] [Google Scholar]
- 32.Haug K, Irgens LM, Baste V, Markestad T, Skjaerven R, Schreuder P. Secular trends in breastfeeding and parental smoking. Acta Paediatr. 1998;87:1023–1027. doi: 10.1080/080352598750031310. [DOI] [PubMed] [Google Scholar]
- 33.Giglia RC, Binns CW, Alfonso HS. Which women stop smoking during pregnancy and the effect on breastfeeding duration. BMC Public Health. 2006;6:195. doi: 10.1186/1471-2458-6-195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hopkinson JM, Schanler RJ, Fraley JK, Garza C. Milk production by mothers of premature infants: influence of cigarette smoking. Pediatrics. 1992;90:934–938. [PubMed] [Google Scholar]
- 35.Vio F, Salazar G, Infante C. Smoking during pregnancy and lactation and its effects on breast-milk volume. Am J Clin Nutr. 1991;54:1011–1016. doi: 10.1093/ajcn/54.6.1011. [DOI] [PubMed] [Google Scholar]
- 36.Andersen AN, Schiøler V. Influence of breast-feeding pattern on pituitary-ovarian axis of women in an industrialized community. Am J Obstet Gynecol. 1982;143:673–677. doi: 10.1016/0002-9378(82)90113-2. [DOI] [PubMed] [Google Scholar]
- 37.Amir LH. Smoking status of breastfeeding women. Acta Paediatr. 1999;88:1412–1413. doi: 10.1080/080352599750030202. [DOI] [PubMed] [Google Scholar]
- 38.O’Brien M, Buikstra E, Hegney D. The influence of psychological factors on breastfeeding duration. J Adv Nurs. 2008;63:397–408. doi: 10.1111/j.1365-2648.2008.04722.x. [DOI] [PubMed] [Google Scholar]
- 39.Howard CR, Howard FM, Lanphear B, deBlieck EA, Eberly S, Lawrence RA. The effects of early pacifier use on breastfeeding duration. Pediatrics. 1999;103:E33. doi: 10.1542/peds.103.3.e33. [DOI] [PubMed] [Google Scholar]
- 40.Scott JA, Binns CW, Oddy WH, Graham KI. Predictors of breastfeeding duration: evidence from a cohort study. Pediatrics. 2006;117:e646–e655. doi: 10.1542/peds.2005-1991. [DOI] [PubMed] [Google Scholar]


