Abstract
Background: Use of a minimally invasive approach for isolated aortic valve surgery is increasing. However, management of the root and/or ascending aorta through a mini-invasive incision is not so frequent. The aim of this study is to report our initial experience with surgery of the ascending aorta through a ministernotomy approach.
Methods: We retrospectively analyzed 102 patients treated for ascending aorta disease through a ministernotomy. Several types of surgeries were performed, including isolated or combined surgical procedures. Pre-operative and operative parameters and in-hospital clinical outcomes were retrospectively analyzed.
Results: Patient mean age was 63.9 ± 13.6 years (range 29–85). There were 33 (32.4%) female and 69 (67.6%) male patients. Preoperative logistic EuroSCORE I was 7.4% ± 2.1%. Mean cardiopulmonary bypass and aortic cross-clamp time were 123.7 ± 36.9 and 100.8 ± 27.5 min, respectively. In-hospital mortality was 0%.
Conclusions: Our experience shows that surgery of the ascending aorta with or without combined procedures can be safely performed through an upper ministernotomy, without compromising surgical results. Although our series is not large, we believe that the experience gained on the isolated aortic valve through a ministernotomy can be safely reproduced in ascending aorta surgery as a routine practice.
Keywords: minimally invasive, ministernotomy, aortic root surgery, ascending aorta surgery
Introduction
Nowadays, a minimally invasive approach through a ministernotomy for isolated aortic valve surgery is finding wide consensus, spreading more and more among the different cardiac surgery centers. However, surgery of the ascending aorta combined or not combined with valve or root surgery is not yet widely performed through a mini-invasive surgical incision. Herein, we report our initial experience for ascending aorta surgery combined or not combined with valve or root surgery through a ministernotomy approach.
Methods
Following Institutional Review Board approval that waived patient consent, data prospectively entered into an institutional surgical database were subsequently retrieved to obtain results from surgeries of the ascending aorta, with or without combined procedures, in patients operated with a minimally invasive approach (upper J-ministernotomy) at the Città di Lecce Hospital GVM Care & Research.
Preoperative assessment
All patients received preoperative multi-modality imaging, including transthoracic ultrasound (US) scan, coronary angiography, aortography and computed (CT) scan with and without contrast medium.
Surgical technique
Intraoperatively, all patients received a trans-esophageal US scan. Under general anesthesia, with the patient in supine position, we performed a 6 cm median skin incision. The incision started at the level of the junction between the manubrium and the sternum body, extending downward. The upper portion of the sternum was transected from the sternal notch vertically to the 4th right intercostal space (upper J ministernotomy) using a conventional vertical saw. A “Massetti mini-sternotomy retractor” (Geister, Tuttlingen, Germany), was used to spread the sternum, together with a soft tissue retractor used to retract the upper portion of the skin incision. Once the pericardium was opened, the ascending aorta was exposed in its full length. Cardiopulmonary bypass was established using direct central aortic and right atrium cannulation (Fig. 1). The left ventricle was vented through the upper right pulmonary vein. Myocardial protection was routinely achieved by an anterograde infusion of warm blood cardioplegia through the aortic root ± selective cannulation of the coronary ostia. CO2 in the surgical field was used to reduce the risk of air embolism. Surgery of the ascending aorta, with or without concomitant aortic valve and root surgery, was routinely performed as per surgeon preference (Fig. 2). Circulatory arrest was never used. During the de-airing procedure, a trans-esophageal ultrasound scan was used to help evaluate the efficacy of the procedure before aortic declamping. Ventricular pacing wires were inserted before declamping the aorta to better allow for exposure of the ventricular wall through the minimal surgical access. Through sub-xyphoideal incisions we inserted one straight 32 Fr/Ch thoracic catheter connected to a water seal multi-chamber thoracic drainage device. We inserted also one flat drain type Jackson Pratt® (Redax, Poggio Rusco MN, Italy) connected with the low continuous self suction system “Emodren” (Medicalplastic s.r.l., Milano, Italy). The sternum was reconstructed with three single steel wires.
Fig. 1.
Central cannulation through the ministernotomy approach.
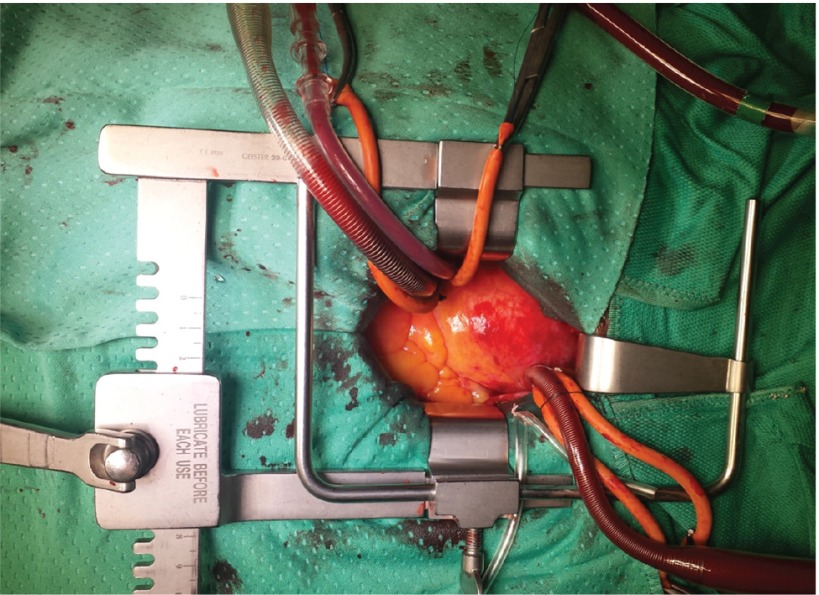
Fig. 2.
The ascending aorta has been resected, the aortic valve exposed and aortic interleaflet triangles reshaping performed through the ministernotomy approach.
Statistical analysis
Continuous variables are expressed as mean ± standard deviation (and median when appropriate) and categorical variables as percentages.
Patients
From April 2011 to October 2014, among 304 aortic surgical procedures performed through an upper J ministernotomy, 102 patients met the inclusion criteria of our retrospective observational study.
Exclusion criteria for minimal access were represented by the need for circulatory arrest and the need for concomitant coronary surgical revascularization. Imaging studies preoperatively guided the indication for circulatory arrest. Therefore, patients with larger distal ascending aorta or proximal aortic arch needing open distal anastomosis with circulatory arrest were not scheduled for minimal access. Operative parameters and early post-operative outcome were analyzed. Follow-up at one month was completed for all patients at the hospital out-patient clinic through clinical, laboratory and instrument (EKG, echocardiogram and chest X-ray) examinations.
Results
We report the results on 102 patients who underwent ascending aorta surgery combined or not combined with valve or root procedures using an upper J ministernotomy. All patients preoperatively scheduled for ministernotomy were operated with this approach. Patient demographics and major comorbidities are tabulated in Table 1. Patients had surgery of the ascending aorta either isolated or concomitant with aortic valve or aortic root surgery. There were: 34 isolated ascending aorta replacements, 25 ascending aorta replacements associated with aortic valve repair and 36 associated with aortic valve replacement (of these one was associated with root repair with a patch technique), five Bentall-De Bono procedures, one Tirone David procedure and one ascending aorta plasty associated with aortic valve replacement (Table 2). Patient mean age was 63.9 ± 13.6 years (range 29–85). There were 33 (32.4%) female and 69 (67.6%) male patients. Preoperative logistic EuroSCORE I was 7.4% ± 2.1%. Mean cardiopulmonary bypass and aortic cross-clamp time were 123.7 ± 36.9 and 100.8 ± 27.5 min, respectively. No patient needed conversion to full sternotomy. One patient (1%) needed surgical re-exploration for post-operative bleeding. The mean intensive care unit (ICU) stay was 2.2 ± 2.0 days. The mean postoperative mechanical ventilation time was 14.3 ± 29.5 h (median 10). The mean hospital stay was 7.8 ± 4.6 days (median 7). The hospital stay was longer than 10 days in 16 patients (15.7%)). Incidence of post-surgery atrial fibrillation was 17.6%. Three patients (2.9%) had postoperative neurological events with full recovery. There were no post-operative acute myocardial infarctions, nor hemodynamic or renal complications nor systemic infections. No patient required permanent pace-maker implantation. One patient (1%) had wound dehiscence and three patients (2.9%) had pericardial effusion needing subxyphoid drainage. In-hospital mortality was 0%. (Table 2). At one month follow-up all patients were doing well with no major complaints.
Table 1.
Preoperative demographics and comorbidities
| Patients | 102 |
| Gender | |
| Male | 69 (67.6%) |
| Female | 33 (32.4%) |
| Age (years) | 63.9 ± 13.6 (29–85) |
| Diabetes | 7 (6.8%) |
| Renal failure | 2 (1.9%) |
| Previous neurologic events | 4 (3.9%) |
| Haemodialysis | 1 (0.9%) |
| Previous neoplasms | 5 (4.9%) |
| COPD | 12 (11.7%) |
| Hypertension | 75 (73.5%) |
| Smoking | 26 (25.4%) |
| Atrial fibrillation | 8 (7.8%) |
| Dyslipidemia | 35 (34.3%) |
| Previous MI | 0 (0%) |
| Logistic EUROscore (%) | 7.4 ± 2.1 |
COPD: chronic obstructive pulmonary disease; MI: myocardial infarction
Table 2.
Operative and postoperative parameters
| Patients | 102 |
| Type of operation | |
| Isolated ascending aorta replacement | 34 |
| Ascending aorta replacement + aortic valve replacement | 35 |
| Ascending aorta replacement + aortic valve replacement + root repair with patch plasty | 1 |
| Ascending aorta replacement + aortic valve repair | 25 |
| Ascending aorta plasty + aortic valve replacement | 1 |
| Bentall-De Bono procedure | 5 |
| Tirone David procedure | 1 |
| CPB time (min) | 123.7 ± 36.9 |
| Cross clamp time (min) | 100.8 ± 27.5 |
| ICU stay (days) | 2.2 ± 2.0 |
| Hospital stay (days) | 7.8 ± 4.6 |
| >10 days | 16 pts (15.7%) |
| Post-operative complications | |
| Atrial fibrillation | 18 (17.6%) |
| Neurological events | 3 (2.9%) |
| Renal failure | 0% |
| Systemic infections | 0% |
| Wound dehiscence | 1 (0.1%) |
| Pericarial tamponade | 3 (2.9%) |
| Surgical reexploration for bleeding | 1 (0.1%) |
| Pneumothorax | 2 (1.9%) |
| 30-days mortality | 0% |
CPB: cardiopulmonary bypass; ICU: intensive care unit
Discussion
Surgery of the aortic root and ascending aorta has been traditionally performed through conventional median full sternotomy. Nowadays, the development of minimally invasive surgery techniques allows excellent results for isolated heart valve disease. Beyond the cosmetic benefits, a mini-invasive approach for valvular surgery has been shown to improve post-operative outcomes and reduce surgical trauma, length of mechanical ventilation and ICU stay.1)
A recent propensity score study demonstrated shorter ventilation times, reduced need of blood transfusion and lower incidence of respiratory failure in patients undergoing aortic valve surgery via the ministernotomy approach compared to the full sternotomy.2)
Theoretically, a minimally invasive approach may be especially useful in a group of patients undergoing major surgery such as on the ascending aorta. Different minimally invasive approaches have been proposed for cardiac surgery.3) The upper J ministernotomy finds wide consensus for the treatment of aortic disease.4,5) The indication for surgery, initially restricted only to selected elective patients, is now extended to more complex surgeries, including both the aortic root, the ascending aorta and redo-operations.4–12) Especially in complex aortic surgery and in high risk patients, a ministernotomy approach can improve respiratory function recovery and allow earlier extubation, reducing ICU and hospital stay.6)
Other authors have previously reported on surgery of the aortic root or ascending aorta through a ministernotomy.
Tabata and co-workers reported in 2007 on 79 patients, comparing them with a cohort undergoing surgery through full sternotomy. This work was remarkable for the variety of different procedures completed using the ministernotomy approach.13)
Perrotta et al. in 2008 reported on 40 patients treated by a Bentall procedure with ministernotomy, using this approach on both elective and emergency patients, and in redo surgery.7)
Svensson et al. in 2001, reporting on a total of 54 patients undergoing minimal valve surgery, included in their study 36 patients operated for ascending aorta replacement, of whom 18 had aortic arch repair through ministernotomy.14)
Preoperative imaging studies are essential for examining the morphological parameters in ascending aortic pathology, in particular the distal ascending diameter guides the need for circulatory arrest, which we believe argues against a minimally invasive approach. In our experience, when scheduling a ministernotomy, we ask for a computed CT scan with contrast medium and also without contrast to better visualize any presence of calcified aortic plaques in the area of distal anastomosis. In our series of patients, we never used circulatory arrest. We believe the minimal skin incision of about 6 cm would not allow an easy manipulation of the aortic arch if selective antegrade cerebral perfusion is planned. However, we should also mention that even maintaining the ministernotomy approach, the soft tissue incision in the upper portion can be extended towards the neck vessels, as previously reported, allowing an easier exposure of the aortic arch.14–16)
Another exclusion criteria in our group of patients was represented by the need of concomitant coronary surgical revascularization. However, we have to mention that we recently started to add coronary revascularization with saphenous vein graft on the main right coronary artery in a few patients treated for aortic valve replacement with a ministernotomy approach (unpublished data).
In fact, with the aorta clamped and the left ventricle vented, it is possible to mobilize the ventricular wall toward the minimal access to allow coronary surgical revascularization on the anterior aspect of the heart. Concerning cannulation strategies, we always cannulated the proximal aortic arch and the right atrium with a double stage cannula. However, in selected cases, femoral cannulation could be used in case of need. Recently, superior vena cava cannulation has been proposed as an alternative strategy for ministernotomy approach.17)
We also would mention that in our group of patients, the low surgical re-exploration rate of 1% was compromised by a 3% rate of sub-xiphoid drainage for late pericardial tamponade. We have no answer at the moment to explain this. We use the same drainage catheters and the same removal protocol that we use in patients operated with full sternotomy.
We started to use the ministernotomy approach for isolated aortic valve replacement in 2011. We then extended this approach also to patients with ascending aorta pathology, and since then this approach has been used more and more in our institution.
In our series of patients, the good outcome (0% mortality at 30 days), the absence of major complications, the length of mechanical ventilation and hospital stay, together with the results reported by others, makes the ministernal technique for the ascending aorta and aortic root a feasible approach. It should also be considered that in our experience we never needed to convert the minimal approach to a full sternotomy in this group of patients.
However, the authors are well aware of the limitations of the present study, the main one being its retrospective and descriptive nature. Considering the non-randomized design, the study may be affected by undetected confounders and procedure bias. The results were also affected by the initial experience in our center. Nevertheless, the lack of a comparison group of patients undergoing the procedure via a conventional full sternotomy would prevent reaching decisive conclusions. A randomized study comparing both surgical approaches would in the future help to draw more meaningful conclusions about the advantages and drawbacks of the ministernotomy approach in this group of patients.
Conclusions
We believe the ministernotomy should be considered a safe alternative approach, not only for isolated aortic valve surgery, but also for more complex surgery involving the root and the ascending aorta. Therefore, despite the limitations of the present study, we thought it useful to report our experience to the surgical community to draw attention to this surgical approach, which could represent a research topic for other surgical groups.
Disclosure Statement
The authors declare no conflicts of interest.
References
- 1).Gilmanov D, Solinas M, Farneti PA, et al. Minimally invasive aortic valve replacement: 12-year single center experience. Ann Cardiothorac Surg 2015; 4: 160-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2).Shehada SE, Öztürk Ö, Wottke M, et al. Propensity score analysis of outcomes following minimal access versus conventional aortic valve replacement. Eur J Cardiothorac Surg 2015; pii: ezv061. [DOI] [PubMed] [Google Scholar]
- 3).Morisaki A, Hattori K, Kato Y, et al. Evaluation of aortic valve replacement via the right parasternal approach without rib removal. Ann Thorac Cardiovasc Surg 2015; 21: 139-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4).Brown ML, McKellar SH, Sundt TM, et al. Ministernotomy versus conventional sternotomy for aortic valve replacement: a systematic review and meta-analysis. J Thorac Cardiovasc Surg 2009; 137: 670-9.e5. [DOI] [PubMed] [Google Scholar]
- 5).Perrotta S, Lentini S. Ministernotomy approach for surgery of the aortic root and ascending aorta. Interact Cardiovasc Thorac Surg 2009; 9: 849-58. [DOI] [PubMed] [Google Scholar]
- 6).Bonacchi M, Prifti E, Giunti G, et al. Does ministernotomy improve postoperative outcome in aortic valve operation? A prospective randomized study. Ann Thorac Surg 2002; 73: 460-5; discussion 465-6. [DOI] [PubMed] [Google Scholar]
- 7).Perrotta S, Lentini S, Rinaldi M, et al. Treatment of ascending aorta disease with Bentall-De Bono operation using a mini-invasive approach. J Cardiovasc Med (Hagerstown) 2008; 9: 1016-22. [DOI] [PubMed] [Google Scholar]
- 8).Viganò M, Rinaldi M, D’Armini AM, et al. Ascending aortic aneurysms treated by cuneiform resection and end-to-end anastomosis through a ministernotomy. Ann Thorac Surg 2002; 74: S1789-91; discussion S1792-9. [DOI] [PubMed] [Google Scholar]
- 9).Totaro P, Carlini S, Pozzi M, et al. Minimally invasive approach for complex cardiac surgery procedures. Ann Thorac Surg 2009; 88: 462-6; discussion 467. [DOI] [PubMed] [Google Scholar]
- 10).Dell’Amore A, Del Giglio M, Calvi S, et al. Mini re-sternotomy for aortic valve replacement in patients with patent coronary bypass grafts. Interact Cardiovasc Thorac Surg 2009; 9: 94-7. [DOI] [PubMed] [Google Scholar]
- 11).Mikus E, Calvi S, Tripodi A, et al. Upper ‘J’ ministernotomy versus full sternotomy: an easier approach for aortic valve reoperation. J Heart Valve Dis 2013; 22: 295-300. [PubMed] [Google Scholar]
- 12).Gaeta R, Lentini S, Raffa G, et al. Aortic Valve replacement by ministernotomy in redo patients with previous left internal mammary artery patent grafts. Ann Thorac Cardiovasc Surg 2010; 16: 181-6. [PubMed] [Google Scholar]
- 13).Tabata M, Khalpey Z, Aranki SF, et al. Minimal access surgery of ascending and proximal arch of the aorta: a 9-year experience. Ann Thorac Surg 2007; 84: 67-72. [DOI] [PubMed] [Google Scholar]
- 14).Svensson LG, Nadolny EM, Kimmel WA. Minimal access aortic surgery including re-operations. Eur J Cardiothorac Surg 2001; 19: 30-3. [DOI] [PubMed] [Google Scholar]
- 15).Svensson LG. Progress in ascending aorta and aortic arch surgery: minimally invasive surgery, blood conservation, and neurological deficit prevention. Ann Thorac Surg 2002; 74: S1786-8; discussion S1792-9. [DOI] [PubMed] [Google Scholar]
- 16).Lentini S, Spinelli D, Pipitò N, et al. Ministernotomy with subclavian extension for the management of a large intrathoracic pseudoaneurysm. J Card Surg 2012; 27: 368-70. [DOI] [PubMed] [Google Scholar]
- 17).Pfeiffer S, Fischlein T, Vogt F, et al. Superior vena cava cannulation in aortic valve surgery: an alternative strategy for a hemisternotomy approach. Interact Cardiovasc Thorac Surg 2015; 20: 863-5. [DOI] [PubMed] [Google Scholar]