Abstract
With the increased reliance on the Pipeline embolization device (PED) for the treatment of complex intracranial aneurysms, our experience in managing intraoperative complications and challenges continues to accumulate amid a scarcity of reports on rescue strategies and innovative techniques. We describe the case of a 50-year-old woman who presented for elective repeat embolization of a right posterior communicating artery aneurysm with some residual aneurysmal filling. During the procedure the patient developed severe vasospasm due to vessel irritation and this led us to proceed to deploy the PED through a biaxial construct composed of the 6 French Envoy MPD DA XB, and the Marksman catheters. The biaxial construct in select patients may provide the required stability while eliminating the need for an intermediate catheter, minimizing embolic risk, and allowing for less irritation to the vessel. Larger studies are required for further validation.
Keywords: Pipeline embolization device
Introduction
As the technology of endovascular management of cerebrovascular diseases continues to advance, safer and more efficacious interventions are now possible with decreased procedural times and improved long-term outcomes.1,2 With the introduction of flexible flow-diverting stents to the neurointerventionalist’s armamentarium, aneurysms that were previously considered technically challenging for endovascular securement have become amenable to treatment via an endovascular approach. Flexible flow-diverting stents such as the Pipeline embolization device (PED; ev3 Neurovascular, Irvine, CA, USA) represent a safe, durable, and feasible option for the management of wide-necked, large aneurysms originating from the petrous to the hypophseal segment of the internal carotid artery (ICA). The low porosity of the internal surface area of the PED is sufficient to disrupt intra-aneurysmal flow to the extent that aneurysms progressively thrombose while allowing continued perfusion of regional branches.3,4
Background and objective
Fundamental to the deployment of a PED in the segment of interest is a stable guide catheter triaxial system. Multiple techniques have been used to construct this stable platform, ranging from using intermediate catheters, on alternative sites of arterial access (brachial, radial or direct carotid approach).5,6 The triaxial systems that are most commonly described are composed of a large-bore guide sheath or catheter, and an intermediate catheter through which the deployment microcatheter is then introduced.7 However in certain cases, creation of a triaxial system is unable to be safely achieved. Newer-generation guide catheters, such as the Envoy MPD DA XB and the Penumbra benchmark catheter, possess both proximal stability, from anchoring the catheter around multiple bends, as well as distal flexibility, thereby obviating the need for a triaxial system. We describe a case of PED deployment using a biaxial system, which provided both safe distal access and sufficient support for PED deployment.
Clinical presentation
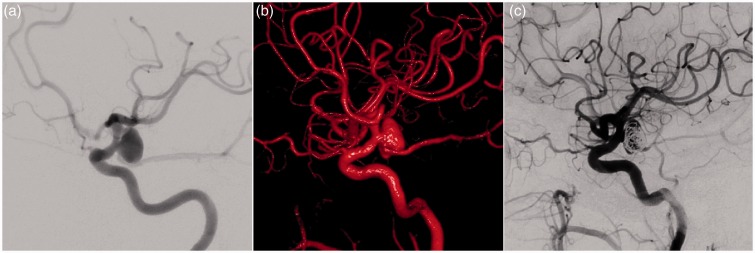
A middle-aged patient presented with complaint of headaches. The workup, which included a computerized tomographic angiography (CTA) and digital subtraction angiography (DSA), revealed multiple unruptured intracranial aneurysms, the largest of which was a right posterior communicating artery aneurysm (Figure 1(a), (b)). The patient underwent primary coil embolization of the right posterior communicating artery aneurysm; however, because of concern about maintaining patency of the posterior communicating artery, the patient was left with residual aneurysmal filling (Figure 1(c)) with intent for future completion of embolization with flow diversion.
Figure 1.
(a) Digital subtraction angiography (DSA) and (b) three-dimensional (3D) volume rendering from rotational angiogram showing a lobulated, right posterior communicating artery aneurysm. (c) DSA after primary coil embolization showing residual aneurysmal filling with maintained patency of posterior communicating artery.
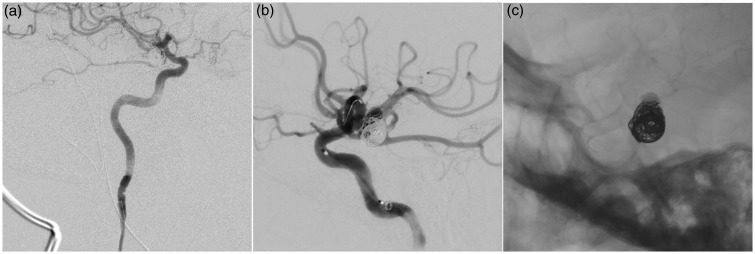
Preoperatively, the patient was loaded with aspirin 325 mg and clopidogrel 600 mg and was placed on aspirin 325 mg and clopidogrel 75 mg daily for six days. Because of the patient’s anatomy, the parent vessel diameter could not safely accommodate anything greater than a 6 French guide catheter. On the initial flow-diversion access attempt, a 6 French Envoy MPD 0.070-inch inner diameter (ID), 100 cm guide catheter was used to access the ICA. However, the catheter was unable to track distally to cervical tortuosity and severe catheter-induced vasospasm resulted (Figure 2(a)). Hence the catheter was removed and intra-arterial verapamil was administered with resolution of spasm.
Figure 2.
(a) Digital subtraction angiography (DSA) at return intervention with 6 French Envoy MPD guide catheter in proximal cervical ICA causing vasospasm. The catheter was unable to be safely advanced further. (b) The 6 French Envoy MPD DA XB within the petrous ICA, with 3.2 French Marksman microcatheter in cavernous ICA prior to PED deployment. The 6 French Envoy MPD DA XB is in optimal deployment position, without vasospasm. (c) Unsubtracted DSA after PED deployment showing adequate deployment of the PED across aneurysm neck and stagnation of contrast within the aneurysm dome. ICA: internal carotid artery; PED: Pipeline embolization device.
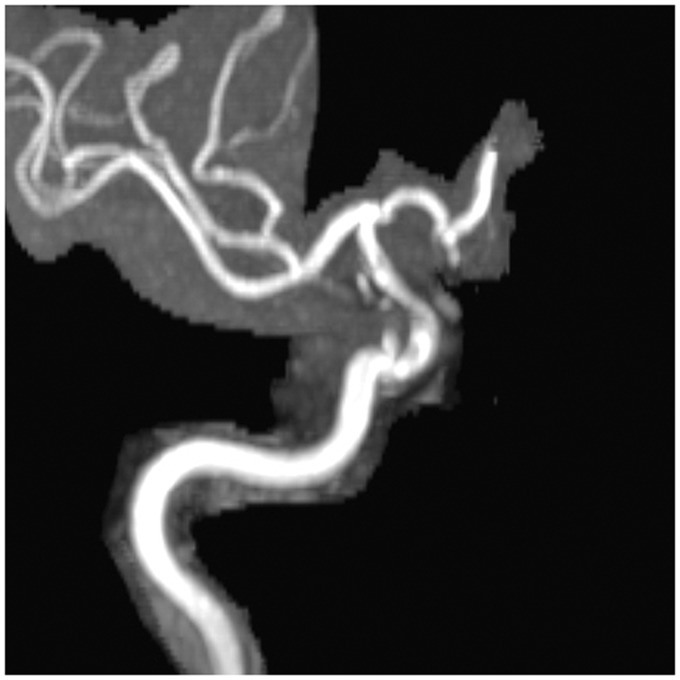
Next, a 6 French Envoy MPD Distal Access (DA) XB, 0.071-inch ID, 105 cm guide catheter was safely navigated across the cervical tortuosity and tracked distally to the horizontal segment of the petrous ICA without any spasm (Figure 2(b)). From here, a 4 mm × 16 mm PED was successfully deployed across the neck of the aneurysm through a 3.2 French Marksman 0.027 inch ID, 150 cm microcatheter. There was good apposition of the stent to the vessel wall with immediate reduction of inflow velocity and stagnation of contrast within the aneurysm (Figure 2(c)). The patient tolerated the procedure well and was discharged in stable condition the following day. At the five-month follow-up she remained asymptomatic with an unchanged neurological exam. A five-month follow-up magnetic resonance angiogram (MRA) with and without gadolinium showed no residual signal intensity or enhancement within the aneurysm neck (Figure 3).
Figure 3.
Five-month follow-up magnetic resonance (MR) angiogram, three-dimensional (3D) time-of-flight, maximum intensity projection (MIP) showing no residual signal intensity or enhancement of aneurysm.
Discussion
Traditionally, neurointerventional procedures were performed using a biaxial system consisting of a rigid guide catheter positioned in the cervical ICA, and a flexible microcatheter that was advanced intracranially to the target of interest. Often the microcatheter had to be advanced a significant distance from the guide catheter, thus reducing the haptic feedback for the operator and increasing unwanted slack in the system. The widespread use of flow-diverting devices, including the PED, for the treatment of intracranial aneurysms has resulted in a need for more substantial access systems. This is mainly because of the larger size of the PED delivery catheter (0.027-inch ID) and the significant deployment manipulations required for proper device placement. Accordingly, there has been a shift in the technique of support systems for cases of PED from a classic biaxial system to a more robust triaxial system.8
The triaxial system that is most commonly described for PED deployment is composed of a Shuttle sheath 0.087-inch ID (Cook Medical, Bloomington, IN, USA) or a Neuron MAX 0.088-inch ID guide catheter (Penumbra, Alameda, CA, USA), a Navien 0.058-inch ID distal intracranial catheter (Covidien Vascular Therapies) and the PED deployment microcatheter— either the Marksman 0.027-inch ID catheter (Covidien Vascular Therapies) or the XT-27 0.027-inch ID catheter (Stryker, Kalamazoo, MI, USA).7,8
However, endovascular embolization of cerebral aneurysms with PEDs in the setting of underlying unfavorable anatomy and cerebral vasospasm can be challenging. In certain cases, the use of a triaxial system is unsuitable because of these situations. Herein we present the only case of PED deployment through biaxial construct composed of the 6 French Envoy MPD DA XB guide catheter and the 3.2 French Marksman delivery microcatheter.
Our patient’s CCA2 and ICAs were small in diameter and unable to accommodate large proximal support such as a 6F Shuttle sheath or NeuronMax 0.088-inch ID guide catheter. On the initial primary coil embolization, a 6 French Envoy MPD 0.070-inch ID, 100 cm guide catheter within the proximal ICA provided sufficient support for primary coil embolization. However, the patient demonstrated mid- and distal cervical ICA tortuosity, which required greater support for proper PED deployment on the second treatment. As such, initial attempts to track a 6 French Envoy MPD 0.070-inch ID guide catheter to the distal ICA resulted in severe vasospasm. Because of the patient’s unfavorable underlying vascular anatomy and ongoing iatrogenic severe cervical vasospasm, the decision was made to track a more flexible guide catheter to the distal cervical ICA, rather than attempting to construct a triaxial system that may have produced more vasospasm in an already narrow-diameter vessel. The biaxial construct composed of the 6F Envoy MPD DA XB and the Marksman catheter provided the required purchase and stability without the resulting vasospasm.
The 6 French Envoy MPD DA XB, 0.071-inch ID is designed with a distal 10 cm hydrophilic coating, making it less traumatic to the vessel wall. Prior case series on the 6 French Envoy MPD DA XB catheter in balloon-assisted coiling have described it as having a stiffer shaft than the regular Envoy, while being able to navigate the arch and provide access to the target vessel and fitting well into smaller vessels.9 In our patient, this catheter was safely positioned in the petrous ICA, which is considered optimal for positioning the intermediate catheter for PED deployment.8
This catheter, along with newer-generation guide and distal access catheters, gains stability from anchoring the catheter around multiple bends rather than the rigidity of traditional catheters. Pipeline deployment requires considerably more manipulations of the system, and thereby more stresses on the distal catheter, than does coiling, stenting and other neurointerventions. This was evident in our case in which a 6 French Envoy MPD 0.070-inch ID was sufficient for the initial primary coil embolization, but was not supportive enough for the subsequent PED deployment. These added stresses are from the multiple pushing and pulling maneuvers performed during Pipeline deployment. Additionally, the larger ID of the 6 French Envoy MPD DA XB catheter helps to accommodate the larger 0.027-inch microcatheter used for flow diverters and also provides additional room for improved flush and contrast injections.
One benefit of using a distal guide catheter placement rather than an intermediate catheter is avoiding triaxial constructs that are known to carry inherent risks for thromboembolic complications.7 The biaxial technique removes an extra step and the need for an intermediate catheter, and in addition to minimizing the embolic risk, it also allows for less irritation to the vessel, which may be crucial in the setting of existing cerebral vasospasm. There is also a likely decrease in procedural device cost with the elimination of the cost of an intermediate catheter.
The PED was deployed safely with no complications and the patient tolerated the procedure well. Although a triaxial platform is well described and may provide more stability, in select patients a biaxial system may carry some advantages over the triaxial system.
It is difficult to quantify the difference in speed and safety between these two techniques since this is largely influenced with operator comfort level and experience. Larger studies are required for further validation.
Conclusion
We present a case in which aneurysmal embolization was achieved via PED deployed through a biaxial construct composed of the 6F Envoy MPD DA XB and the Marksman catheters in the setting of vasospasm. The biaxial construct in select patients may provide the required stability while eliminating the need for an intermediate catheter, minimizing embolic risk, and allowing for less irritation to the vessel. Larger studies are required for further validation.
Acknowledgments
Author contributions: Al-Mufti: acquisition of data, analysis and interpretation, draft of the manuscript, critical revision of the manuscript for important intellectual content; Amuluru: acquisition of data, analysis and interpretation, draft of the manuscript, critical revision of the manuscript for important intellectual content; Singh: acquisition of data, critical revision of the manuscript for important intellectual content; Gandhi: critical revision of the manuscript for important intellectual content, study supervision; Prestigiacomo: critical revision of the manuscript for important intellectual content, study supervision.
There are no additional unpublished data from this study.
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Chalouhi N, McMahon JF, Moukarzel LA, et al. Flow diversion versus traditional aneurysm embolization strategies: Analysis of fluoroscopy and procedure times. J Neurointerv Surg 2014; 6: 291–295. [DOI] [PubMed] [Google Scholar]
- 2.Murthy SB, Shah S, Venkatasubba Rao CP, et al. Treatment of unruptured intracranial aneurysms with the pipeline embolization device. J Clin Neurosci 2014; 21: 6–11. [DOI] [PubMed] [Google Scholar]
- 3.Nelson PK, Lylyk P, Szikora I, et al. The pipeline embolization device for the intracranial treatment of aneurysms trial. AJNR Am J Neuroradiol 2011; 32: 34–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kallmes DF, Ding YH, Dai D, et al. A new endoluminal, flow-disrupting device for treatment of saccular aneurysms. Stroke 2007; 38: 2346–2352. [DOI] [PubMed] [Google Scholar]
- 5.Nii K, Kazekawa K, Onizuka M, et al. Direct carotid puncture for the endovascular treatment of anterior circulation aneurysms. AJNR Am J Neuroradiol 2006; 27: 1502–1504. [PMC free article] [PubMed] [Google Scholar]
- 6.Layton KF, Kallmes DF, Cloft HJ. The radial artery access site for interventional neuroradiology procedures. AJNR Am J Neuroradiol 2006; 27: 1151–1154. [PMC free article] [PubMed] [Google Scholar]
- 7.Turk A, Manzoor MU, Nyberg EM, et al. Initial experience with distal guide catheter placement in the treatment of cerebrovascular disease: Clinical safety and efficacy. J Neurointerv Surg 2013; 5: 247–252. [DOI] [PubMed] [Google Scholar]
- 8.Colby GP, Lin LM, Huang J, et al. Utilization of the Navien distal intracranial catheter in 78 cases of anterior circulation aneurysm treatment with the Pipeline embolization device. J Neurointerv Surg 2013; 5(Suppl 3): iii16–iii21. [DOI] [PubMed] [Google Scholar]
- 9.Luzardo GD, Ross IB, Gal G. Balloon-assisted coiling through a single 6F guiding catheter. AJNR Am J Neuroradiol 2006; 27: 190–191. [PMC free article] [PubMed] [Google Scholar]