Abstract
This study examined how various types of resources influence perceived health of caregivers. Guided by the conservation of resources theory, a caregiver health model was built and tested using structural equation modeling. The caregiver health model consisted of caregiving situations (functional limitations and cognitive impairments of older adults and caregiving time), resources (financial resources, mastery, social support, family harmony, and service utilization), caregiver burden, and perceived health of caregivers. The sample included 1,837 unpaid informal caregivers drawn from the 2004 National Long-Term Caregiver Survey. The model fit indices indicated that the first structural model did not fit well; however, the revised model yielded an excellent model fit. More stressful caregiving situations were associated with fewer resources and higher burden, whereas greater resources were associated with lower burden and better perceived health of caregivers. The results suggest explicit implications for social work research and practice on how to protect the health of caregivers.
Keywords: caregiver health, caregiving burden, conservation of resources theory, informal caregiving, structural equation modeling
Approximately 43.5 million people (18 percent of the population) in the United States care for family members or friends age 50 or older (National Alliance for Caregiving & AARP, 2009) and play a major role in providing long-term care (LTC) for older adults. These informal caregivers, caring for their family members or friends with disability or illness, are characterized as hidden patients because of their high health risks (Roche, 2009). Despite numerous caregiving studies, evidence about the influence of resources on the health of informal caregivers tends to be fragmented, possibly because of the relative lack of attention on perceived health rather than caregiver burden or depression (Anderson & Elmståhl, 2008) and the reliance on stress and coping models in caregiving research. In the 1990s, several researchers argued for the necessity of resource-oriented perspectives in framing and understanding caregiving experiences (see, for example, Clair, Fitzpatrick, & La Gory, 1995; Rapp, Shumaker, Schmidt, Naughton, & Anderson, 1998). However, most caregiver stress and coping models frame resources as moderators focusing on the cognitive process of caregiving experiences (Rapp et al., 1998), thereby underestimating the environmental effects of resources (Hobfoll, 1989). A comprehensive examination of the effects of different types of resources on perceived health of caregivers is needed to better understand the role of resources in caregiving and to inform interventions by identifying critical resources and their relationships with perceived health.
Conservation of Resources (COR) Theory and Caregiver Health
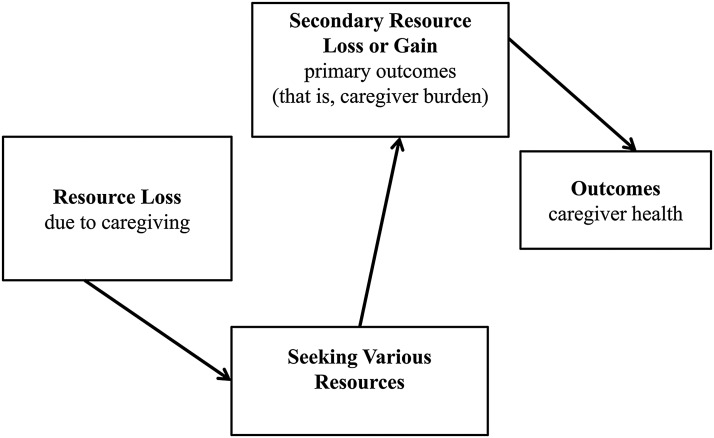
The COR theory addresses the call to examine resource-oriented perspectives. The COR theory is an integrated stress theory that suggests a balanced emphasis on the environmental and internal aspects of the stress process (Hobfoll, 1989). The COR theory defines resources as “those objects, characteristics, conditions, or energies that are valued by the individual” (Hobfoll, 1989, p. 517). Despite some variations, resources have been conceptualized as something that can protect caregivers from stressful caregiving experiences, which is in accordance with the COR theory’s definition of resources. The basic principle of the COR theory is that “individuals strive to retain, protect, and build resources” (Hobfoll, 2001, p. 341). When a loss of resources is anticipated or actual loss of resources occurs, individuals experience stress and then try to offset net loss by turning to other resources (Hobfoll, 1989, 2001). In this process, “successful adaptation of resource conservation strategies” leads to a gain in “secondary resources,” whereas “unsuccessful adaptation of resource conservation strategies” results in “secondary losses” (Hobfoll, 2001, p. 358). This resource-maintaining process can be applied to caregiving. For example, while caring for older adults, caregivers experience resource losses in terms of time. Caregivers then try to restore lost resources by seeking help from their friends. If caregivers successfully gain support from friends, they offset their lost resources. However, if not, stressful caregiving situations worsen. This process of resource gain or loss ultimately affects caregivers’ health; continued gain in resources may maintain caregivers’ health, whereas constant losses in resources may lead to a deterioration of health (see Figure 1). Recently, Li, Shaffer, and Bagger (2015) used the COR theory to examine work–caregiving conflict and found that supervisory support and family strain moderated the relationship between caregiving demands and psychological well-being of caregivers of people with disabilities.
Figure 1:
Application of the Conservation of Resources Theory to Caregiving
Caregiving Situations
Within the COR theory, caregiving conditions refer to objective caregiving situations such as the health status of the older adults or caregiving time, which are believed to result in resource loss and therefore prompt resource-seeking behaviors. Functional limitations and cognitive impairments of older adults have been found to be related to caregiver burden (Casado & Sacco, 2012; Kim, Chang, Rose, & Kim, 2012), and as time spent in caregiving increases, perceived burden rises (Kim et al., 2012) and health deteriorates (Pinquart & Sörensen, 2011). More functional limitations of older adults were related to increased use of formal services (Hong, 2009).
Resources
Hobfoll (1989) conceptualized resources as all visible or invisible assets that individuals possess or use to improve situations. Guided by the COR theory, this study approaches resources from a broad perspective, including financial, psychological (caregivers’ mastery), informal (social support and family harmony), and formal resources (service utilization) that relieve caregivers’ stressful caregiving situations. Perceived economic hardship, a measure of limited financial resources, was associated with burden (Tilden, Tolle, Drach, & Perrin, 2004). In addition, greater caregiver mastery was associated with increased use of formal services (Keith, Wacker, & Collin, 2009), lower burden (Cheng, Lam, Kwok, Ng, & Fung, 2013), and better health (Ducharme et al., 2007). Because caregiving is demanding, caregivers often face situations in which they need and seek help from others such as family or friends; higher levels of social support were associated with lower burden (Wilk & Croom, 2008). Furthermore, cooperation and harmony among family members in caring for older adults serve as an informal resource for caregivers; when caregivers experienced increased family conflict, they were more likely to report greater burden (Casado & Sacco, 2012). Use of formal service was also associated with better psychological well-being of caregivers (Nakagawa & Nasu, 2011).
Caregiving Outcome: Burden and Perceived Health
Caregiving burden and self-rated health often have been investigated as caregiving outcomes (see, for example, Casado & Sacco, 2012; Kim et al., 2012). Zarit, Todd, and Zarit (1986) defined caregiver burden as the extent to which caregivers suffer from caregiving emotionally, physically, or socially. More functional limitations of older adults were associated with more caregiver burden (Casado & Sacco, 2012; Kim et al., 2012). Moreover, a decline in health has been found among caregivers. Caregivers reported poorer perceived health status than noncaregivers (Pinquart & Sörensen, 2003) and were more likely to be susceptible to developing a chronic disease such as heart disease or high blood pressure (Vitaliano, Zhang, & Scanlan, 2003). Increased caregiver burden was associated with poorer health of caregivers (Anderson & Elmståhl, 2008).
Conceptual Model and Hypotheses
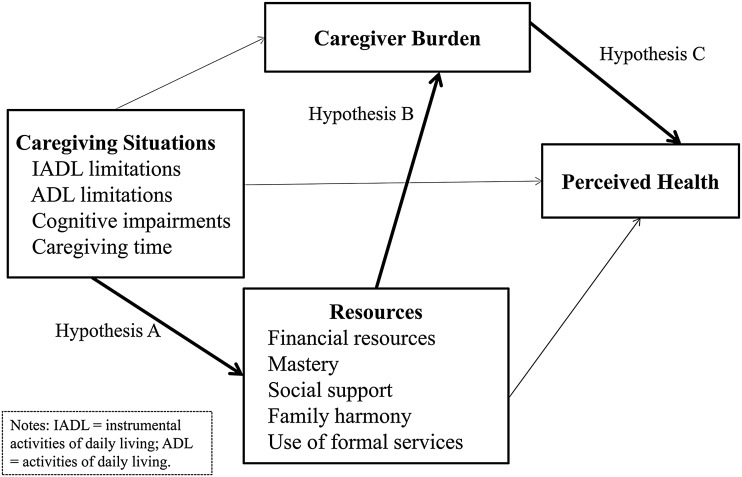
Despite the call for a focus on resources almost two decades ago (Clair et al., 1995; Rapp et al., 1998), to our knowledge no studies have examined how various types of resources affect perceived health of people caring for older adults. In addition, tests of theory-driven health models can contribute to health care practice by providing empirical evidence to select key components needed for implementation of effective health interventions (Michie & Prestwich, 2010). Thus, this study aims to present and test a structural model based on resource-oriented theory of caregivers’ health. Based on the literature review and the COR theory, the following relationships are hypothesized: (a) More stressful caregiving situations are associated with greater resources; (b) greater resources are associated with lower burden; and (c) greater resources are associated with better health of caregivers (see Figure 2).
Figure 2:
Conceptual Caregiver Health Model
Method
Data Source and Sample
The data for the study were extracted from a Caregiver Survey in the 2004 National Long-Term Care Survey (NLTCS) (Manton, 2010). The NLTCS was sponsored by the National Institute on Aging and conducted by the Duke University Center for Demographic Studies (Grant No. U01-AG007198). The NLTCS Caregiver Survey involved primary caregivers of older adults with any activities of daily living (ADL) or instrumental activities of daily living (IADL) limitations of at least three-month duration. For this study, two inclusion criteria were applied to select a NLTCS caregiver sample: survey completion and unpaid informal caregiving. Of a total of 2,292 caregivers, 369 incomplete cases and 85 paid caregiver cases were excluded, resulting in a sample of 1,838. Because no systematic sampling strategy was used, the NLTCS caregivers sample should be considered a convenience sample (Manton, 2010). The current study was determined to be not human subject research due to the de-identified data by the institutional review board of the coauthor’s university.
Measures
Perceived Health of Caregivers
A single item was used to assess perceived health status of caregivers. The item asks caregivers to rate their perceived health status on a four-point scale (ranging from 1 = excellent to 4 = poor). Higher scores represent worse perceived health status. A single general self-rated health measure (SRH) has been widely used and valued in health research because of its simplicity and validity (Meng, Xie, & Zhang, 2014). A longitudinal study found that SRH was associated with objective (for example, developing a chronic disease) and subjective (for example, loneliness) health status (Shadbolt, 1997). Furthermore, a systematic review found that SRH predicted mortality (DeSalvo, Bloser, Reynolds, He, & Muntner, 2006).
Functional Limitations of the Older Adults
Two items were used to assess functional limitations of the older adults being cared for: the number of ADL and IADL limitations. ADL limitations include nine items: eating, getting in or out of bed, getting in or out of chairs, walking around inside, going outside, dressing, bathing, getting to the bathroom, and controlling bowel movement or urination; possible scores range from 0 to 9. IADL limitations consist of seven items: the ability to prepare meals, do laundry, do light housework, grocery shop, manage money, make phone calls, and take medications; possible scores range from 0 to 7.
Cognitive Impairment of the Older Adults
A dichotomous variable was used to assess cognitive impairment of older adults by combining the Short Portable Mental Status Questionnaire (SPMSQ) (Pfeiffer, 1975) and six questions. The SPMSQ with 10 items gauges the older adults’ ability to answer simple questions regarding their age and address. In addition, based on the skip patterns used in the NLTCS survey, questions about whether older adults had Alzheimer’s disease, mental retardation, and dementia were combined. Because the majority of older adults have no cognitive impairment in this combined scale, a dichotomous variable was created (1 = some cognitive impairment, 0 = no cognitive impairment).
Caregiving Time
A single open-ended question, “How many hours do you spend helping your older adult in a typical week?” was used to measure time spent on caregiving.
Financial Resources
A single item asking the caregiver to rate the degree of perceived financial hardship for caring on a five-point scale (ranging from 1 = no hardship at all to 5 = a great deal of hardship) was used to measure perceived financial resources. This item was recoded so that a higher score indicates more financial resources (that is, less hardship).
Mastery
Two items were used to assess caregiving mastery. These two items ask the caregivers to what degree each statement describes the caregivers themselves on a four-point scale (ranging from 1 = not at all to 4 = completely): “You work hard as caregivers but never seem to make any progress” and “You have more things to do than you can handle.” These items were selected because they are similar to those on the caregiver mastery subscale in the revised caregiver appraisal scale (Lawton, Moss, Hoffman, & Perkinson, 2000), capturing caregivers’ perceived ability in caring. The internal consistency reliability was good (α = .76) in this sample.
Social Support
Eight items were used to measure perceived social support. The items ask caregivers about the extent to which they disagree or agree with each statement on a four-point scale (ranging from 1 = strongly disagree to 4 = strongly agree). Statements include whether respondents have a friend or relative who can be trusted, confided in, and who encourages them. Possible scores range from 8 to 32; the internal consistency reliability was very good (α = .89) in this sample.
Family Harmony
The eight-item scale about family conflict was used to measure family harmony. This scale asks the caregivers about other family members’ involvement in caregiving and their attitude toward their older adults on a four-point scale (ranging from 1 = quite a bit of disagreement to 4 = no disagreement), with scores ranging from 8 to 32. The scale was scored so that a higher score indicates less family conflict (that is, greater family harmony). The internal consistency reliability was excellent (α = .93) in this sample.
Service Utilization
The NLTCS has seven questions that ask whether the older adult has ever used home and community-based services such as temporary care service, outside home program, home-based care, home-delivered meal service, housekeeping services, transportation services, and support group services. Due to the lack of variability on the individual items, a single dichotomous item was created to assess service utilization (0 = no use of any services, 1 = use of at least one service).
Caregiving Burden
Four items were used to measure perceived burden. The items ask caregivers to choose “true” or “false” for each statement such as “I don’t have as much privacy when I take care of the older adult” and “Taking care of the older adult has caused my health to get worse” (0 = false, 1 = true). With a possible score ranging from 0 to 4, the internal consistency reliability was good (α = .83) in this sample.
Data Analysis
Structural equation modeling was conducted to examine the caregiver health model of the relations among caregiving situations, caregiving resources, burden, and perceived health using Mplus Version 6.0 (Muthén & Muthén, 2010). Because of two dichotomous variables (that is, cognitive impairment and service utilization), weighted least squares means and variance–adjusted estimation was used. Missing values on scale items were addressed by applying ipsative mean imputation procedures following Schafer and Graham’s (2002) recommendations. The distribution of univariate normality was examined to check the assumption of multivariate normality (Kline, 2005). The greatest absolute values of skewness and kurtosis were 1.87 and 4.95 for caregiving time, respectively, suggesting that the assumption of multivariate normality was adequately met. Correlations among individual variables were also examined to check bivariate multicollinearity, and it was adequately met. In addition to the hypothesized relationships, other possible paths (that is, caregiving situations to caregiver burden, caregiving situations to perceived health, and resources to perceived health) were also added and examined to further understand relationships between variables.
Results
Table 1 presents the sample characteristics of NLTCS caregivers in this study. The majority of caregivers were female (65 percent) and married (70 percent). Most caregivers were white (87 percent) and almost half of them had more than a high school education (47 percent). Caregivers on average spent 24 hours (SD = 35.1) in a typical week caring for their older adults. Age is not available in the NLTCS, but Hong (2009) reported a mean age of 61 and a range of 15 to 97 in a similar sample.
Table 1:
National Long-Term Care Survey Demographic Characteristics
| Variable | % |
|---|---|
| Gender (n = 1,837) | |
| Male | 35.0 |
| Female | 65.0 |
| Race (n = 1837) | |
| White | 87.4 |
| Black | 8.9 |
| Other | 3.7 |
| Marital status (n = 1,821) | |
| Never married | 10.3 |
| Married | 69.8 |
| Separated/divorced/widowed | 18.7 |
| Education (n = 1,799) | |
| Less than high school | 19.8 |
| High school | 33.3 |
| Associate/vocational degree | 27.1 |
| Bachelor degree | 12.5 |
| Graduate degree | 7.4 |
| Relationship (n = 1,834) | |
| Spouse | 33.8 |
| Son/daughter | 48.1 |
| Son-in-law/daughter-in-law | 3.2 |
| Brother/sister | 3.1 |
| Other relatives or friends | 12.6 |
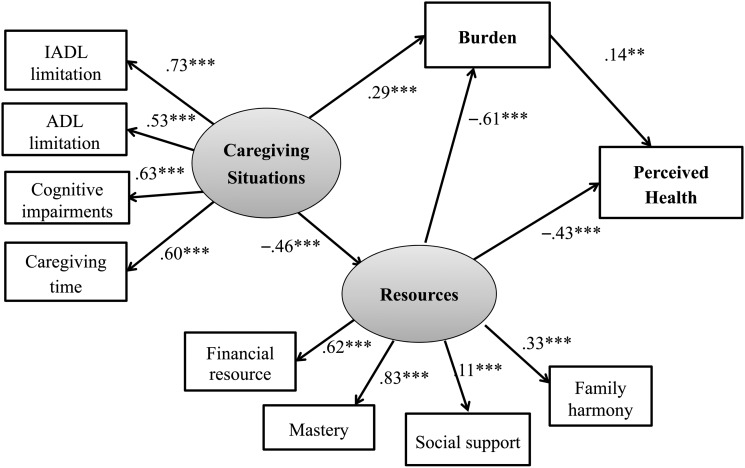
Structural Model
First, we tested the caregiver health model that includes all indicators for caregiving situations (that is, IADL and ADL limitations, cognitive impairment, and caregiving time) and resources (perceived financial resource, mastery, social support, family harmony, and services utilization), caregiver burden, and perceived health; however, this yielded a poor model fit, χ2(41) = 259.734 (p < .001), Tucker–Lewis index (TLI) = .892, Comparative Fit Index (CFI) = .920, root mean square error of approximation (RMSEA) = .054 (90% confidence interval [CI]: .048, .060, probability RMSEA ≤ 05 = .147). As the poor model fit suggests, one indicator behaved unacceptably. Contrary to prior research, the indicator of service utilization negatively loaded on resources (loading = –.40, p < .001). Therefore, the revised caregiver health model (see Figure 2) was developed by deleting service utilization. The revised model yielded an excellent model fit, χ2 (32) = 129.606 (p < .001), TLI = .941. CFI = .958, RMSEA = .040 (90% CI: .033, .048, probability RMSEA ≤ .05 = .984). Standardized factor loadings for all indicators were significant at p < .001, ranging from .11 to .83. More negative caregiving situations were associated with fewer resources (β = –.46) and higher burden (β = .26). Fewer resources were associated with higher caregiver burden (β = –.61) and poorer health of caregivers (β = .43), and higher burden was also related to poorer perceived health (β = –.14). In addition, a small indirect relationship between caregiving situations and perceived health of caregivers was found through resources (β = .19); more difficult caregiving situations were associated with lower levels of caregiver perceived health through lower resources. The indicators with the smallest factor loading and the greatest factor loading were social support (.11) and mastery (.83) for the resources latent variable. The revised model accounted for 60 percent of the variance in burden and 11 percent of the variance in caregivers’ perceived health. Figure 3 presents the revised model with significant paths only.
Figure 3:
Revised Caregiver Health Model
Notes: IADL = instrumental activities of daily living; ADL = activities of daily living. Standardized coefficients are presented.
**p < .01. ***p < .001.
Discussion
Despite the critical role of resources, there is a lack of research examining the various aspects and functions of resources on perceived health of caregivers. The findings indicated that the latent variable of resources was the only component that has substantial relationships with other variables in this structural model. Furthermore, the relationship between resources and perceived health (β = –.43, p < .001) was stronger than the relationship between caregiver burden and perceived health (β = .14, p = .002), indicating the significant direct effect of resources on caregivers’ perceived health. As the COR theory predicted, lower resources were related to higher burden and poorer perceived health. Resources measured by financial hardship, mastery, social support, and family harmony were negatively associated with burden and caregiver health. These findings are consistent with prior studies that found positive effects of financial resources (Tilden et al., 2004), self-efficacy (Cheng et al., 2013), social support (Wilk & Croom, 2008), and family cooperation (Casado & Sacco, 2012) on caregiver well-being or burden.
However, a negative relationship between caregiving situations and resources was found, which is inconsistent with the COR theory. According to the COR theory, more stressful caregiving situations should lead to greater resources to make up for the resource loss arising from caregiving (Hobfoll, 1989). There are two plausible explanations for this finding. First, because a cross-sectional design was used, this study could not capture how caregivers in more stressful caregiving situations react to their loss of resources. Instead, this study might only present the cross-sectional correlates of stressful situations and resources of caregivers. Second, because of the limitation of secondary data used in this study, all indicators for the resources latent variable were perceived rather than actual resource-seeking behaviors or acquisition of resources. Thus, the findings only suggest that as health of the older adults deteriorates and caregiving time increases, perceived resources such as caregiver mastery and social support decrease. This might imply that caregivers perceived decreases in the resources even if resources have remained stable, thereby indicating growing needs of caregivers.
Limitations
This study has several limitations. The NLTCS used a convenience sample, so findings from this study may not be generalizable to the entire caregiver population. In addition, because of the cross-sectional research design, casual relationships between variables could not be tested, which may account for the inconsistent findings with the COR theory as discussed.
Implications for Research and Practice
Despite its limitations, this study contributes to the literature by providing practical implications for research and practice. First, longitudinal designs are needed to clarify causal relationships among variables in this model. As caregivers provide care, the health of the older adults gets worse and the size of social networks or amount of social support changes as well. One longitudinal study found that available support for caregivers significantly decreased over five years (Clay, Roth, Wadley, & Haley, 2008). Given the importance of resources that was underlined in this study, decreases in resources may greatly affect caregiver health in negative ways. In addition, it may be necessary to use different health outcome variables such as mental health outcomes to expand our understanding of role of resources in caregiving. Although our model explained 60 percent of the variance in burden, it only explained 11 percent of the variance in perceived caregiver health, which may indicate the necessity of examining other types of health outcome variables.
This study also provides implications for social work practice. In the structural model, only the resources latent variable had a meaningful relationship with perceived health of caregivers, suggesting a critical role of resources in protecting health of caregivers. Social work practitioners can play a vital role in maintaining health of informal caregivers in the community by improving resources available to them and helping them navigate access to such resources. In particular, given the highest loading of mastery on resources, social workers need to actively implement skill-based interventions for caregivers to improve caregiver self-efficacy. Skill-based interventions can include education and information about caring for older adults and for locating necessary community services. Recent intervention research identified effective skills that can enhance caregiver self-efficacy such as caregiving-related decision-making skills and information on dealing with the symptoms of cognitive impairments (Judge, Yarry, Looman, & Bass, 2013).
This study found that financial resources might be a crucial factor in supporting perceived caregiver health. Caregiving often leads to additional costs such as medical expenses, lost wages, and employment benefits. Sun, Hilgeman, Durkin, Allen, and Burgio (2009) found that perceived financial strain had a stronger relationship with depressive symptoms and anxiety than actual income had with these outcomes among caregivers. Actual financial assistance can also help relieve the financial burden associated with caregiving costs. There are financial aid programs for caregivers such as the National Family Caregiver Support Program, the Dependent Care Tax Credit, and other tax incentive programs at the state level. However, funding for these programs is insufficient to cover the needs of family caregivers (Colello, 2009). Social work practitioners need to be actively involved in assessing financial needs of caregivers, locating and mobilizing necessary financial resources for them, and advocating for additional financial supports for caregivers.
References
- Anderson S., Elmståhl S. (2008). The relationship between caregiver burden, caregivers’ perceived health and their sense of coherence in caring for elders with dementia . Journal of Clinical Nursing , 6, 790–799. doi:10.1111/j.1365-2702.2007.02066.x [DOI] [PubMed] [Google Scholar]
- Casado B., Sacco P. (2012). Correlates of caregiver burden among family caregivers of older Korean Americans . Journal of Gerontology, Series B: Psychological Sciences and Social Sciences , 67B, 331–336. doi:10.1093/geronb/gbr115 [DOI] [PubMed] [Google Scholar]
- Cheng S., Lam L., Kwok T., Ng N., Fung A. (2013). Self-efficacy is associated with less burden and more gains from behavioral problems of Alzheimer’s disease in Hong Kong Chinese caregivers . Gerontologist , 53, 71–80. doi:10.1093/geront/gns062 [DOI] [PubMed] [Google Scholar]
- Clair J. M., Fitzpatrick K. M., La Gory M. E. (1995). The impact of psychosocial resources on caregiver burden and depression: Sociological variations on a gerontological theme . Sociological Perspectives , 38, 195–215. Retrieved from http://ucpressjournals.com/journal.php?j=sop [Google Scholar]
- Clay O. J., Roth D. L., Wadley V. G., Haley W. E. (2008). Changes in social support and their impact on psychosocial outcome over a 5-year period for African American and white dementia caregivers . International Journal of Geriatric Psychiatry , 23, 857–862. doi:10.1002/gps.1996 [DOI] [PubMed] [Google Scholar]
- Colello K. J. (2009). Family caregiving to the older population: Background, federal programs, and issues for Congress (CRS Report RL 34123). Retrieved from Congressional Research Service Web site: http://crs.wikileaks-press.org/RL34123.pdf [Google Scholar]
- DeSalvo K., Bloser N., Reynolds K., He J., Muntner P. (2006). Mortality prediction with a single general self-rated health question: A meta-analysis . Journal of General Internal Medicine , 21, 267–275. doi:10.1111/j.1525-1497.2005.00291.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ducharme F., Lévesque L., Lachance L., Gangbè M., Zarit S. H., Vézina J., Caron C. D. (2007). Older husbands as caregivers: Factors associated with health and the intention to end home caregiving . Research on Aging , 29, 3–31. doi:10.1177/0164027506291749 [Google Scholar]
- Hobfoll S. E. (1989). Conservation of resources: A new attempt at conceptualizing stress . American Psychologist , 44, 513–524. doi:10.1037/0003-066X.44.3.513 [DOI] [PubMed] [Google Scholar]
- Hobfoll S. E. (2001). The influence of culture, community, and the nested-self in the stress process: Advancing conservation of resource theory . Applied Psychology: An International Review , 50, 337–421. doi:10.1111/1464-0597.00062 [Google Scholar]
- Hong S.-L. (2009). Understanding patterns of service utilization among informal caregivers of community older adults . Gerontologist , 50, 87–99. doi:10.1093/geront/gnp105 [DOI] [PubMed] [Google Scholar]
- Judge K. S., Yarry S., Looman W., Bass D. (2013). Improved strain and psychosocial outcomes for caregivers of individuals with dementia: Findings from project ANSWERS . Gerontologist , 53, 280–292. doi:10.1093/geront/gns076 [DOI] [PubMed] [Google Scholar]
- Keith P., Wacker R., Collin S. (2009). Family influence on caregiver resistance, efficacy, and use of services in family elder care . Journal of Gerontological Social Work , 52, 377–400. doi:10.1080/01634370902304 [DOI] [PubMed] [Google Scholar]
- Kim H., Chang M., Rose K., Kim S. (2012). Predictors of caregiver burden in caregivers of individuals with dementia . Journal of Advanced Nursing , 68, 846–855. doi:10.1111/j.1365-2648.2011.05787.x [DOI] [PubMed] [Google Scholar]
- Kline R. B. (2005). Principles of structural equation modeling (2nd ed.). New York: Guilford Press; . [Google Scholar]
- Lawton M. P., Moss M., Hoffman C., Perkinson M. (2000). Two transitions in daughters’ caregiving careers . Gerontologist , 40, 437–448. doi:10.1093/geront/40.4.437 [DOI] [PubMed] [Google Scholar]
- Li A., Shaffer J., Bagger J. (2015). The psychological well-being of disability caregivers: Examining the roles of family strain, family-to-work conflict, and perceived supervisor support . Journal of Occupational Health Psychology , 20, 40–49. doi:10.1037/a0037878 [DOI] [PubMed] [Google Scholar]
- Manton K. G. (2010). National Long-Term Care Survey: 1982, 1984, 1989, 1994, 1999, and 2004 (ICPSR096810-v5). Ann Arbor, MI: Inter-university Consortium for Political and Social Research [Distributor] . doi:10.3886/ICPSR09681.v5 [Google Scholar]
- Meng Q., Xie Z., Zhang T. (2014). A single-item self-rated health measure correlates with objective health status in the elderly: A survey in suburban Beijing . Frontiers in Public Health , Article 27 doi:10.3389/fpubh.2014.00027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michie S., Prestwich A. (2010). Are interventions theory-based? Development of a theory coding scheme . Health Psychology , 29, 1–8. doi:10.1037/a0016939 [DOI] [PubMed] [Google Scholar]
- Muthén L., Muthén B. (2010). Mplus (Version 6.0) [Computer software] . Los Angeles: Authors; . [Google Scholar]
- Nakagawa Y., Nasu S. (2011). Association between components of family caregivers’ sense of burden and types of paid care services provided in Japan . Aging & Mental Health , 15, 687–701. doi:10.1080/13607863.2011.562181 [DOI] [PubMed] [Google Scholar]
- National Alliance for Caregiving & AARP. (2009). Caregiving in the U.S 2009: A focused look at those caring for the 50+. Retrieved from http://assets.aarp.org/rgcenter/il/caregiving_09.pdf [Google Scholar]
- Pfeiffer E. (1975). A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients . Journal of the American Geriatrics Society , 23, 433–441. Retrieved from http://onlinelibrary.wiley.com/journal/10.1111/(ISSN)1532-5415 [DOI] [PubMed] [Google Scholar]
- Pinquart M., Sörensen S. (2003). Differences between caregivers and noncaregivers in psychological health and physical health: A meta-analysis . Psychology and Aging , 18, 250–267. Retrieved from http://www.apa.org/pubs/journals/pag/index.aspx [DOI] [PubMed] [Google Scholar]
- Pinquart M., Sörensen S. (2011). Spouse, adult children and children-in-law as caregivers of older adults: A meta-analytic comparison . Psychology and Aging , 26, 1–14. doi:10.1037/a0021863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rapp S. R., Shumaker S., Schmidt S., Naughton M., Anderson R. (1998). Social resourcefulness: Its relationship to social support and wellbeing among caregivers of dementia victims . Aging & Mental Health , 2, 40–48. doi:10.1080/13607869856920 [Google Scholar]
- Roche V. (2009). The hidden patient: Addressing the caregiver . American Journal of the Medical Sciences , 337, 199–204. doi:10.1097/MAJ.0b013e31818b114d [DOI] [PubMed] [Google Scholar]
- Schafer J., Graham J. W. (2002). Missing data: Our view of the state of the art . Psychological Methods , 7, 147–177. doi:10.1037/1082-989X.7.2.147 [PubMed] [Google Scholar]
- Shadbolt B. (1997). Some correlates of self-rated health for Australian women . American Journal of Public Health , 87, 951–956. doi:10.2105/AJPH.87.6.951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun F., Hilgeman M. M., Durkin D. W., Allen R. S., Burgio L. (2009). Perceived income inadequacy as a predictor of psychological distress in Alzheimer’s caregivers . Psychological Aging , 24, 177–183. doi:10.1037/a0014760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tilden V., Tolle S., Drach L., Perrin N. (2004). Out-of-hospital death: Advance care planning, decedent symptoms, and caregiver burden . Journal of the American Geriatrics Society , 52, 532–539. doi:10.111/j.1532-5415.2004.52158.x [DOI] [PubMed] [Google Scholar]
- Vitaliano P., Zhang J., Scanlan J. (2003). Is caregiving hazardous to one’s physical health? A meta-analysis . Psychological Bulletin , 129, 946–972. doi:10.1037/0033-2909.129.6.946 [DOI] [PubMed] [Google Scholar]
- Wilk S. E., Croom B. (2008). Perceived stress and resilience in Alzheimer’s disease caregivers: Testing moderation and mediation models of social support . Aging & Mental Health , 12, 357–365. doi:10.1080/13607860801933323 [DOI] [PubMed] [Google Scholar]
- Zarit S., Todd P., Zarit J. (1986). Subjective burden of husbands and wives as caregivers: A longitudinal study . Gerontologist , 26, 260–266. doi:10.1093/geront/26.3.260 [DOI] [PubMed] [Google Scholar]