Abstract
Background
Preoperative B-type natriuretic peptide (BNP) is known to predict adverse outcomes after cardiac surgery. The value of postoperative BNP for predicting adverse outcomes is less well delineated. The authors hypothesized that peak postoperative plasma BNP (measured postoperative days 1–5) predicts hospital length of stay (HLOS) and mortality in patients undergoing primary coronary artery bypass grafting, even after adjusting for preoperative BNP and perioperative clinical risk factors.
Methods
This study is a prospective longitudinal study of 1,183 patients undergoing primary coronary artery bypass grafting surgery. Mortality was defined as all-cause death within 5 yr after surgery. Cox proportional hazards analyses were conducted to separately evaluate the associations between peak postoperative BNP and HLOS and mortality. Multivariable adjustments were made for patient demographics, preoperative BNP concentration, and clinical risk factors. BNP measurements were log10 transformed before analysis.
Results
One hundred fifteen deaths (9.7%) occurred in the cohort (mean follow-up = 4.3 yr, range = 2.38–5.0 yr). After multivariable adjustment for preoperative BNP and clinical covariates, peak postoperative BNP predicted HLOS (hazard ratio [HR] = 1.28, 95% CI = 1.002–1.64, P = 0.049) but not mortality (HR = 1.62, CI = 0.71–3.68, P = 0.25), whereas preoperative BNP independently predicted HLOS (HR = 1.09, CI = 1.01–1.18, P = 0.03) and approached being an independent predictor of mortality (HR = 1.36, CI = 0.96–1.94, P = 0.08). When preoperative and peak postoperative BNP were separately adjusted for within the clinical multivariable models, each independently predicted HLOS (preoperative BNP HR = 1.13, CI = 1.05–1.21, P = 0.0007; peak postoperative BNP HR = 1.44, CI = 1.15–1.81, P = 0.001) and mortality (preoperative BNP HR = 1.50, CI = 1.09–2.07, P = 0.01; peak postoperative BNP HR = 2.29, CI = 1.11–4.73, P = 0.02).
Conclusions
Preoperative BNP may be better than peak postoperative BNP for predicting HLOS and longer term mortality after primary coronary artery bypass grafting surgery.
PLASMA B-type natriuretic peptide (BNP) is secreted primarily by cardiac ventricular myocytes in response to increased ventricular wall stress related to volume expansion, pressure overload, or ischemia.1,2 In addition to having compensatory diuretic, natriuretic, and vasodilatory properties, plasma BNP is an established diagnostic and prognostic biomarker in both ambulatory heart failure and acute coronary syndrome patients.2–11 Similarly, elevations in preoperative BNP have been shown to predict increased morbidity or mortality after cardiac surgery,12–17 even after adjusting for clinical risk factors.13–15 Postoperative BNP has the potential to reflect both the preoperative condition of the heart and myocardial insults induced by intraoperative and early postoperative cardiac stress. However, the utility of postoperative plasma BNP for perioperative risk stratification has not been as clearly delineated, possibly because previous studies have used small cohorts or have enrolled subjects undergoing diverse surgeries.12,16–22 Furthermore, previous studies have not directly compared the predictive value of preoperative versus postoperative plasma BNP. Therefore, using a prospectively enrolled cohort of 1,183 subjects undergoing primary coronary artery bypass grafting (CABG) with cardiopulmonary bypass (CPB), we hypothesized that peak postoperative plasma BNP independently predicts increased hospital length of stay (HLOS) and up to 5 yr all-cause mortality, even after adjusting for preoperative BNP concentration and clinical risk factors.
Materials and Methods
Study Population
Between August 2001 and September 2006, 1,519 men and women aged 20 to 89 yr scheduled for isolated primary CABG surgery with CPB at Brigham Women’s Hospital, Boston, Massachusetts, and Texas Heart Institute, St. Luke’s Episcopal Hospital, Houston, Texas, were prospectively enrolled in an ongoing parent study known as the CABG Genomics Study.††23,24 Respective institutional review board approval and written informed consent of the subjects was obtained. CABG Genomics Study exclusion criteria included a preoperative hematocrit less than 25% or transfusion of leukocyte-rich blood products within 30 days before surgery. Enrolled subjects were, in addition, prospectively excluded from the analysis of this study if they had undergone previous cardiac surgery, if they underwent emergency surgery or concurrent valve surgery, if they received a preoperative inotrope, intraaortic balloon pump, or ventricular assist device support, or if they were missing preoperative or peak postoperative plasma BNP measurements. Patients with severe renal dysfunction (requiring preoperative hemodialysis or having preoperative serum creatinine > 3 mg/dl) were also excluded from analysis because severe renal dysfunction and perioperative dialysis can variably affect perioperative plasma BNP concentrations.25,26
Data and Blood Collection
Data were collected for each enrolled subject during primary hospitalization using a detailed prospectively designed study case report form that included (1) preoperative demographic characteristics, comorbidities, and medications; (2) surgical characteristics; and (3) postoperative in-hospital events. Data were subjected to automated range and logic checking and an additional manual audit of a proportion of records. Postoperative patient survival was assessed annually by mail or telephone interviews, and by examination of the Social Security Death Index. Death events were assessed through February 1, 2009.
Plasma samples obtained preoperatively and on postoperative days (PODs) 1–5 were stored in vapor-phase liquid nitrogen until analysis. BNP and cardiac troponin I were measured for all time points at a single core laboratory using sandwich immunoassays on a Triage® platform (Biosite, San Diego, CA).
Definitions
Study predictor covariates were prospectively defined as follows. Peak postoperative plasma BNP was assessed if a subject had at least three POD 1–5 measures and was defined as the highest of the measured POD 1–5 values. Creatinine clearance was estimated for all subjects using the four variable estimated glomerular filtration rate equation from the Modification of Diet in Renal Disease Study Group.27,28 Postoperative creatinine clearance was estimated using each subject’s peak postoperative creatinine from routine measurements made during primary hospitalization. Postoperative ventricular dysfunction was defined as a new requirement for two or more inotropes or as a new placement of an intraaortic balloon pump or ventricular assist device either during the intraoperative period after the patient separated from CPB or postoperatively in the intensive care unit. Inotrope support was defined as continuous infusion of amrinone, milrinone, dobutamine, dopamine (>5 μg · kg−1 · min−1), epinephrine, isoproterenol, norepinephrine, or vasopressin. New onset postoperative atrial fibrillation was defined as the occurrence of atrial fibrillation in patients who did not present for surgery in atrial fibrillation but who developed atrial fibrillation postoperatively as identified from nursing, physician, or electrocardiogram reports during primary hospitalization.
Mortality was defined as all-cause death within 5 yr after primary CABG surgery. HLOS was assessed as a continuous outcome for all analyses except receiver operating characteristic (ROC) curve analysis. For ROC analysis, extended HLOS was defined as primary hospitalization longer than 12 days after surgery (90th percentile for the study cohort).
Statistical Analysis
Statistical analyses were conducted using SAS (version 9.1; SAS Institute, Cary, NC) and R (R Foundation for Statistical Computing, Vienna, Austria). The R statistical package powerSur-vEpi (Channing Laboratory, Boston, MA) was used for Cox proportional hazards model-based power calculations.29 After excluding subjects from analysis according to prospectively defined exclusion criteria, assuming 80% power and a type I error rate = 0.05, we estimated a minimum detectable unadjusted hazard ratio (HR) of 2.28 for the association between a 1 unit change in log10 peak postoperative BNP and risk of mortality during 5 yr postoperative follow-up.
The Wilcoxon signed-rank test was used to compare differences in BNP concentrations between the different study time points. The Wilcoxon rank sum test was used to conduct between group comparisons of BNP levels measured at each time point after stratifying subjects by occurrence of extended HLOS or by mortality during up to 5 yr follow-up. Because preoperative and peak postoperative BNP data were right skewed, continuous plasma BNP was log10 transformed to normalize distribution before regression analyses. Linear regression was used to determine the square of Pearson correlations (r2), reflecting association between log10 preoperative and log10 postoperative BNP (peak postoperative and POD 1) measurements. Categorical and continuous patient and clinical characteristics (table 1) were assessed for univariate association with HLOS or mortality using Cox proportional hazards regression analyses.
Table 1.
Patient Demographics, Medications, and Perioperative Clinical Risk Factors for Increased Hospital Length of Stay and Mortality after Primary Coronary Artery Bypass Grafting
| Preoperative Demographics and Risk Factors (n = 1,183) | Mean or Proportion | Univariate Association with HLOS (Hazard Ratio, P Value) | Univariate Association with All-cause Mortality (Hazard Ratio, P Value) 115 Death Events |
|---|---|---|---|
| Age (yr) | 63.8 ± 10.1 | 1.01, < 0.0001 | 1.08, < 0.0001 |
| Female gender | 213 (18.0) | 1.10, 0.20 | 0.93, 0.76 |
| Institution | |||
| Brigham and Women’s Hospital | 879 (74.3) | 1.31, < 0.0001 | 0.75, 0.21 |
| Texas Heart Institute | 304 (25.7) | ||
| Ethnicity (minority) | 190 (16.1) | 1.13, 0.12 | 0.51, 0.04 |
| Diabetes mellitus (n = 1,182) | 344 (29.1) | 1.14, 0.04 | 1.32, 0.16 |
| Hypertension (n = 1,180) | 882 (74.7) | 1.21, 0.004 | 1.00, 0.99 |
| Hypercholesterolemia (n = 1,178) | 886 (75.2) | 0.85, 0.02 | 0.49, 0.0002 |
| Obesity (BMI > 30 kg/m2) | 471 (39.8) | 1.18, 0.006 | 1.23, 0.28 |
| Smoking, > 30-pack-year history (n = 1,135) | 305 (26.9) | 1.16, 0.03 | 2.36, < 0.0001 |
| Preoperative creatinine clearance (ml · min−1 · 1.73 m−2) (n = 1,182) | 74.7 ± 20.7 | 0.995, < 0.0001 | 0.99, 0.02 |
| Myocardial infarction ≤ 2 wk preoperatively (n = 1,181) | 206 (17.4) | 1.28, 0.002 | 1.38, 0.15 |
| Left ventricular ejection fraction (%)(n = 1,130) | 52.7 ± 12.4 | 0.99, < 0.0001 | 0.97, < 0.0001 |
| Coronary artery regions with > 50% stenosis | Overall P value 0.01 | Overall P value 0.03 | |
| 0–1 Region | 87 (7.3) | 1 | 1 |
| 2 Regions | 390 (33.0) | 0.74 | 0.43 |
| 3 Regions | 706 (59.7) | 0.85 | 0.47 |
| Mitral insufficiency (moderate or severe) (n = 1,142) | 25 (2.2) | 1.30, 0.20 | 3.34, 0.002 |
| Past arrhythmia | 118 (10.0) | 1.57, < 0.0001 | 2.23, 0.0009 |
| Anemia (n = 1,180) | 391 (33.1) | 1.27, 0.0001 | 1.94, 0.0004 |
| Median preoperative BNP (pg/ml) (10th and 90th percentile), mean preoperative BNP (pg/ml) ± SD | 16.4, [1.5, 122.8], 47.6 ± 92.8 | 1.22 for log10 increase, < 0.0001 | 1.99 for log10 increase, < 0.0001 |
| Preoperative cTnI > 0.1μg/l | 173 (14.6) | 1.11, 0.21 | 0.91, 0.72 |
| Preoperative medications | |||
| ACE inhibitor (n = 1,182) | 549 (46.4) | 1.10, 0.09 | 0.84, 0.34 |
| Diuretic (n = 1,182) | 249 (21.1) | 1.42, < 0.0001 | 1.33, 0.18 |
| Statin | 915 (77.3) | 0.87, 0.04 | 0.55, 0.002 |
| Digoxin | 32 (2.7) | 1.81, 0.002 | 3.94, < 0.0001 |
| β blocker | 913 (77.2) | 0.87, 0.05 | 0.67, 0.04 |
| Aspirin | 899 (76.0) | 0.89, 0.10 | 0.73, 0.12 |
| Nonaspirin platelet inhibitor (n = 1,182) | 257 (21.7) | 1.29, 0.0003 | 0.83, 0.45 |
| Nitroglycerin intravenous (n = 1,178) | 120 (10.2) | 1.04, 0.67 | 0.87, 0.67 |
| Heparin intravenous | 267 (22.6) | 1.10, 0.16 | 1.13, 0.58 |
| Surgical risk factors | |||
| Urgent surgery (n = 1,181) | 647 (54.8) | 1.02, 0.71 | 1.20, 0.33 |
| Cardiopulmonary bypass time > 120 min | 257 (21.7) | 1.20, 0.01 | 0.58, 0.04 |
| No. coronary grafts (n = 1,182) | Overall P value 0.65 | Overall P value 0.003 | |
| 1–2 Grafts | 176 (14.9) | 1 | 1 |
| 3 Grafts | 533 (45.1) | 0.97 | 1.05 |
| ≥ 4 Grafts | 473 (40.0) | 1.03 | 0.51 |
| In-hospital postoperative outcomes | |||
| Ventricular dysfunction | 138 (11.7) | 2.33, < 0.0001 | 2.75, < 0.0001 |
| New onset atrial fibrillation | 340 (28.7) | 1.81, < 0.0001 | 2.14, < 0.0001 |
| Postoperative creatinine clearance (ml · min−1 · 1.73 m−2) (n = 1,182) | 68.3 ± 21.5 | 0.99, < 0.0001 | 0.98, < 0.0001 |
| Peak postoperative cTnI (μg/l) | 1.25 [0.37, 7.49] | 1.32 for log10 increase, < 0.0001 | 0.90 for log10 increase, 0.56 |
Data are shown as n (%) for dichotomous variables and mean ± SD or median (10th and 90th percentiles) for continuous variables. ACE = angiotensin converting enzyme; BMI = body mass index; BNP = B-type natriuretic peptide; HLOS = hospital length of stay.
Using covariates listed in table 1, multivariable prediction models for HLOS and up to 5 yr mortality were separately developed using Cox proportional hazards regression with a semiparsimonious stepwise selection approach (two-tailed nominal P value thresholds for model entry and exit were 0.15 and 0.05, respectively). Age, gender, institution, and ethnicity were locked into the multivariable HLOS and mortality models before stepwise selection. Despite dropping out of the models during stepwise selection, the left ventricular ejection fraction covariate was subsequently forced back into both the HLOS and the mortality models because of perceived potential for this covariate to confound associations between BNP and the study outcomes. To avoid excessive influence of subjects who were outliers for HLOS, subjects who had HLOS greater than 30 days were censored at 30 days. For seven subjects who died during primary hospitalization within 30 days of surgery, HLOS was censored on the day of death. To assess whether peak postoperative BNP independently predicted HLOS or mortality after adjusting for preoperative BNP and perioperative clinical risk factors, peak postoperative BNP was added into both the HLOS and the mortality multivariable Cox proportional hazards models. To secondarily assess whether peak postoperative BNP predicted HLOS and mortality after adjusting for perioperative clinical risk factors but not adjusting for preoperative BNP, peak postoperative BNP was added into both the HLOS and the mortality models without preoperative BNP being included in the models. Because several previous studies have only assessed the predictive value of postoperative BNP measured approximately 24 h after cardiac surgery,12,17,18,20,21 we in addition used the same approach that we used for assessing peak postoperative BNP to assess the independent value of BNP measured on POD 1 for predicting HLOS and mortality.
Akaike information criteria (AIC) were used to compare goodness of fit for the multivariable HLOS and mortality models including (1) clinical covariates without any BNP covariates, (2) clinical covariates with preoperative BNP added, (3) clinical covariates with peak postoperative BNP added, and (4) clinical covariates with preoperative and peak postoperative BNP added simultaneously. The AIC is a statistical criterion used to compare how well different multivariable regression models that contain data from the same exact patients predict an outcome. A multivariable model is considered better for predicting a study outcome if it has a lower AIC. ROC curves were used to assess the relationship between peak postoperative BNP concentrations and both extended HLOS and mortality through 2.38 yr of follow-up (the minimum duration of study follow-up that all study subjects had reached). Both the HLOS and the mortality outcomes were dichotomized before ROC assessment because ROC analyses should not be conducted for time-censored outcome data. Areas under the ROC curves with 95% CIs and related specificities and sensitivities for the 75th percentile of peak postoperative BNP were calculated.
Results
Of the 1,519 subjects enrolled into the source cohort during the study period, 336 were prospectively excluded from the analysis for one or more of the following exclusion criteria: no CABG surgery performed (n = 16), previous cardiac surgery (n = 6), concurrent valve surgery performed (n = 61), emergency surgery (n = 4), CPB not used (n = 52), aortic cross-clamp not used (n = 76), preoperative intraaortic balloon pump (n = 39), preoperative inotropes (n = 8), preoperative hemodialysis (n = 2), preoperative serum creatinine more than 3 mg/dl (n = 4), no preoperative BNP (n = 98), or no peak postoperative BNP measurement (n = 166). Three of the subjects excluded for missing peak postoperative BNP died during the first five PODs (two died on POD 1 and one died on POD 4).
Patient Characteristics
Perioperative demographic, medical, and surgical characteristics of the 1,183 subjects included in the study analysis are listed in table 1 along with their univariate associations with HLOS and mortality during up to 5 yr of follow-up. Log10 preoperative plasma BNP concentration was univariately associated with both HLOS (HR = 1.22, 95% CI = 1.15–1.28, P < 0.0001) and mortality (HR = 1.99, 95% CI = 1.53–2.60, P < 0.0001).
Changes in Perioperative Plasma BNP Concentrations through POD 5
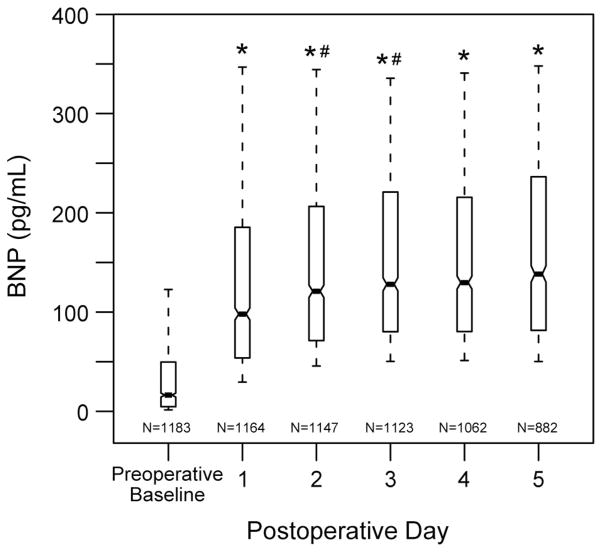
POD 1–5 plasma BNP concentrations were all significantly increased compared with preoperative plasma BNP concentration (P < 0.0001; fig. 1). Preoperative plasma BNP measurements significantly associated with peak postoperative plasma BNP (r2 = 0.30, P < 0.0001). Median peak postoperative BNP concentration = 177.6 pg/ml, with a 10th to 90th percentile range of 77.7–475.6 pg/ml. Mean peak postoperative BNP is 246.5 ± 229.5 pg/ml. Plasma BNP levels rose consecutively and significantly during PODs 1–3 (P < 0.0005), whereas POD 3–5 BNP measurements plateaued and did not increase significantly (P > 0.05) (fig. 1). Patients with extended HLOS had significantly higher BNP concentrations at all perioperative time points (P < 0.0001). Patients who died during the 5-yr follow-up period had significantly higher BNP concentrations at all perioperative time points (P < 0.0001).
Fig. 1.
Perioperative plasma B-type natriuretic peptide (BNP) concentrations for 1,183 subjects undergoing primary coronary artery bypass graft surgery with 10th, 25th, 50th, 75th, and 90th percentile values shown for each time point. * P < 0.0001 compared with preoperative baseline. # P < 0.0005 compared with previous postoperative day.
Relationship of Peak Postoperative BNP to Hospital Stay
Seven subjects died in hospital within 30 days of surgery, and 12 subjects had HLOS longer than 30 days. Only four subjects were discharged on POD 4. Median HLOS was 7 days (10th and 90th percentiles: 5 and 12 days, respectively). One hundred thirteen subjects had extended HLOS (i.e., greater than 12 days).
Peak postoperative plasma BNP concentrations are univariately associated with HLOS (HR = 2.04, 95% CI = 1.71–2.43, P < 0.0001). The value of peak postoperative BNP concentration for predicting HLOS was evaluated after adjusting for preoperative BNP concentration, demographic characteristics (age, sex, institution, and ethnicity), and other clinical predictors including: preoperative medications, history of preoperative arrhythmia treatment, extended CPB time, preoperative left ventricular ejection fraction, new onset postoperative atrial fibrillation, postoperative ventricular dysfunction, and decreased postoperative creatinine clearance (table 2). After multivariable adjustment for preoperative BNP and clinical covariates, peak postoperative BNP predicted HLOS (HR = 1.28, 95% CI = 1.002–1.64, P = 0.049). In this multivariable clinical model containing preoperative and peak postoperative BNP together, preoperative BNP also independently predicted HLOS (HR = 1.09, 95% CI = 1.01–1.18, P = 0.03). When preoperative BNP concentration was not included in the multivariable model, peak postoperative BNP continued to be an independent predictor of HLOS (HR =1.44, 95% CI =1.15–1.81, P = 0.001).
Table 2.
Proportional Hazards Model of Hospital Stay after Primary Coronary Artery Bypass Graft Surgery with Preoperative and Postoperative B-type Natriuretic Peptide Measures Alone and Together in the Model (n = 1,131*)
| AIC = 4,641.79 for Clinical Model without BNP Covariates | Model Including Log10 Preoperative BNP AIC = 4,632.84 |
Model Including Log10 Peak Postoperative BNP AIC = 4,633.60 |
Model Including Both Log10 Preoperative BNP and Log10 Peak Postoperative BNP AIC = 4,630.94 |
|||
|---|---|---|---|---|---|---|
| Hazard Ratio (95% CI) | P Value | Hazard Ratio (95% CI) | P Value | Hazard Ratio (95% CI) | P Value | |
| Predictor | ||||||
| Log10 preoperative BNP | 1.13 (1.05–1.21) | 0.0007 | — | — | 1.09 (1.01–1.18) | 0.03 |
| Log10 peak postoperative BNP | — | — | 1.44 (1.15–1.81) | 0.001 | 1.28 (1.002–1.64) | 0.049 |
| Age (10-yr increment) | 1.07 (1.003–1.14) | 0.04 | 1.07 (1.003–1.14) | 0.04 | 1.06 (0.994–1.13) | 0.08 |
| Gender (female) | 1.08 (0.92–1.27) | 0.32 | 1.05 (0.89–1.24) | 0.55 | 1.05 (0.89–1.23) | 0.59 |
| Institution | 1.63 (1.40–1.90) | < 0.0001 | 1.70 (1.45–1.98) | < 0.0001 | 1.69 (1.45–1.98) | < 0.0001 |
| Ethnicity (minority) | 1.20 (1.01–1.43) | 0.04 | 1.20 (1.01–1.43) | 0.03 | 1.20 (1.01–1.43) | 0.03 |
| Preoperative nonaspirin platelet inhibitor | 1.22 (1.05–1.41) | 0.01 | 1.24 (1.07–1.44) | 0.004 | 1.23 (1.06–1.43) | 0.007 |
| Preoperative β blocker | 0.84 (0.72–0.97) | 0.02 | 0.84 (0.72–0.97) | 0.02 | 0.83 (0.72–0.96) | 0.01 |
| History of preoperative arrhythmia treatment | 1.24 (1.01–1.52) | 0.04 | 1.26 (1.02–1.55) | 0.03 | 1.24 (1.01–1.52) | 0.04 |
| Cardiopulmonary bypass time > 120 min | 1.21 (1.04–1.41) | 0.01 | 1.22 (1.05–1.42) | 0.009 | 1.21 (1.04–1.41) | 0.01 |
| Preoperative left ventricular ejection fraction (%) | 0.999 (0.994–1.004) | 0.72 | 0.998 (0.993–1.003) | 0.49 | 1.000 (0.994–1.005) | 0.88 |
| New onset postoperative atrial fibrillation | 1.81 (1.57–2.08) | < 0.0001 | 1.78 (1.54–2.04) | < 0.0001 | 1.79 (1.55–2.05) | < 0.0001 |
| Postoperative ventricular dysfunction | 2.16 (1.76–2.65) | < 0.0001 | 2.08 (1.69–2.55) | < 0.0001 | 2.09 (1.70–2.56) | < 0.0001 |
| Postoperative creatinine clearance (ml · min−1 · 1.73 m−2) | 0.988 (0.985–0.991) | < 0.0001 | 0.988 (0.985–0.991) | < 0.0001 | 0.989 (0.986–0.992) | < 0.0001 |
Fifty-two subjects missing one or more of the model’s predictor variables and are not included in this analysis; 18 subjects censored for hospital length of stay more than 30 days or for in-hospital death within 30 days of surgery.
AIC = Akaike information criterion; BNP = B-type natriuretic peptide; CI = confidence interval.
To assess the goodness of fit of multivariable models for predicting HLOS, AIC were compared for each of the four multivariable models that contained clinical covariates alone or in combination with preoperative or peak postoperative BNP (table 2). The AICs from highest to lowest (worst to best fit) were as follows: 4,641.79 (clinical covariates without BNP covariates), 4,633.60 (clinical covariates with peak postoperative BNP), 4,632.84 (clinical covariates with preoperative BNP), and 4,630.94 (clinical covariates with both preoperative and peak postoperative BNP). Therefore, preoperative BNP alone improved model fit more than peak postoperative BNP alone, but adding peak postoperative BNP to the model together with preoperative BNP additionally improved the model fit for HLOS.
Area under the ROC curve describing the relationship between peak postoperative BNP and occurrence of extended HLOS was 0.69 (95% CI: 0.63–0.74; P < 0.0001). Associated specificity and sensitivity for the peak postoperative BNP cutoff of 303.7 pg/ml (75th percentile) were 77 and 46%, respectively.
Relationship of Peak Postoperative BNP to Postoperative Mortality
During the 5-yr postoperative follow-up period, 115 subjects died (9.7%), with the mean time between surgery and death being 2.5 ± 1.6 yr (range 6 days–5 yr). Because only seven subjects died within 30 days of surgery, we did not assess the predictors of short-term postoperative mortality. Mean follow-up for the 1,068 living patients was 4.3 ± 0.9 yr (range 2.38–5.0 yr).
Peak postoperative plasma BNP concentrations univariately associated with mortality during up to 5 yr postoperative follow-up (HR = 5.89, 95% CI = 3.38–10.28, P < 0.0001). The value of peak postoperative BNP concentration for predicting mortality was evaluated after adjusting for preoperative BNP concentration, demographic characteristics (age, sex, institution, and ethnicity) and other likely clinical predictors including: preoperative medications, preoperative left ventricular ejection fraction, greater than 30 pack year history of smoking, and decreased postoperative creatinine clearance (table 3). After these multivariable adjustments neither peak postoperative BNP concentration (HR = 1.62, 95% CI = 0.71–3.68, P = 0.25) nor preoperative BNP concentration (HR = 1.36, 95% CI = 0.96–1.94, P = 0.08) independently predicted mortality. When preoperative BNP concentration was not included in the multivariable model, peak postoperative BNP was an independent predictor of mortality (HR = 2.29, 95% CI = 1.11–4.73, P = 0.02).
Table 3.
Proportional Hazards Model of up to 5-yr All-cause Mortality after Primary Coronary Artery Bypass Graft Surgery with Preoperative and Postoperative BNP Measures Alone and Together in the Model (n = 1,089*)
| AIC = 1,267.26 for Clinical Model without BNP Covariates | Model Including Log10 Preoperative BNP AIC = 1,262.21 |
Model Including Log10 Peak Postoperative BNP AIC = 1,264.21 |
Model Including Both Log10 Preoperative BNP and Log10 Peak Postoperative BNP AIC = 1,262.89 |
|||
|---|---|---|---|---|---|---|
| Hazard Ratio (95% CI) | P Value | Hazard Ratio (95% CI) | P Value | Hazard Ratio (95% CI) | P Value | |
| Predictor | ||||||
| Log10 preoperative BNP | 1.50 (1.09–2.07) | 0.01 | — | — | 1.36 (0.96–1.94) | 0.08 |
| Log10 peak postoperative BNP | — | — | 2.29 (1.11–4.73) | 0.02 | 1.62 (0.71–3.68) | 0.25 |
| Age (10-yr increment) | 1.65 (1.32–2.06) | < 0.0001 | 1.67 (1.34–2.09) | < 0.0001 | 1.63 (1.31–2.04) | < 0.0001 |
| Gender (female) | 0.81 (0.48–1.36) | 0.42 | 0.77 (0.45–1.31) | 0.33 | 0.76 (0.45–1.30) | 0.31 |
| Institution | 1.42 (0.80–2.51) | 0.23 | 1.49 (0.83–2.67) | 0.18 | 1.51 (0.84–2.70) | 0.17 |
| Ethnicity (minority) | 0.68 (0.33–1.43) | 0.31 | 0.70 (0.34–1.47) | 0.35 | 0.69 (0.33–1.45) | 0.33 |
| Preoperative digoxin | 2.67 (1.32–5.38) | 0.006 | 2.79 (1.39–5.62) | 0.004 | 2.69 (1.34–5.43) | 0.006 |
| Preoperative beta blocker | 0.63 (0.41–0.96) | 0.03 | 0.66 (0.43–1.02) | 0.06 | 0.63 (0.41–0.98) | 0.04 |
| > 30-pack-year history of smoking | 1.73 (1.15–2.61) | 0.009 | 1.68 (1.11–2.54) | 0.01 | 1.70 (1.12–2.56) | 0.01 |
| Preoperative left ventricular ejection fraction (%) | 0.99 (0.97–1.01) | 0.19 | 0.99 (0.97–1.001) | 0.07 | 0.99 (0.97–1.01) | 0.24 |
| Postoperative creatinine clearance (ml · min−1 · 1.73 m−2) | 0.987 (0.977–0.998) | 0.02 | 0.987 (0.977–0.998) | 0.02 | 0.988 (0.977–0.999) | 0.03 |
Ninety-four subjects missing one or more of the model’s predictor variables and are not included in this analysis; 100 death events included in the analysis.
AIC = Akaike information criterion; BNP = B-type natriuretic peptide; CI = confidence interval.
To assess which model had the most goodness of fit for predicting mortality, AIC were compared with the four multivariable models that contained clinical covariates alone or in combination with preoperative or peak postoperative BNP (table 3). The AICs from highest to lowest (worst to best fit) were as follows: 1,267.26 (clinical covariates without BNP covariates), 1,264.21 (clinical covariates with peak postoperative BNP), 1,262.89 (clinical covariates with both preoperative and peak postoperative BNP), and 1,262.21 (clinical covariates with preoperative BNP). Therefore, preoperative BNP alone improved model fit for predicting mortality more than peak postoperative BNP alone or peak postoperative BNP considered in combination with preoperative BNP.
Fifty-seven death events occurred during the first 2.38 yr of follow-up (the minimal duration that all subjects in the cohort had been followed). Area under the ROC curve describing the relationship between peak postoperative BNP and mortality up to 2.38 yr of postoperative follow-up = 0.64 (95% CI: 0.57–0.72; P = 0.0002). Associated specificity and sensitivity for the peak postoperative BNP cutoff of 303.7 pg/ml (75th percentile) were 76 and 46%, respectively.
Relationship of POD 1 BNP to Postoperative Hospital Stay and Survival
Although post-CABG BNP measurements typically peak later than POD 1 (fig. 1), because several previous studies have assessed the utility of POD 1 BNP for perioperative risk stratification, we in addition assessed the predictive value of POD 1 BNP in our study cohort.12,17,18,20,21 Preoperative plasma BNP measurements are significantly associated with POD 1 plasma BNP (r2 = 0.23, P < 0.0001). Median POD 1 BNP concentration = 98.2 pg/ml, with a 10th to 90th percentile range of 29.5–347.9 pg/ml. POD 1 BNP concentrations were univariately associated with HLOS (HR = 1.29, 95% CI =1.16–1.43, P <0.0001) and with mortality during up to 5 yr postoperative follow-up (HR = 2.94, 95% CI = 1.87–4.61, P < 0.0001). However, POD 1 BNP was not significantly associated with either outcome after multivariable adjustments were made for the clinical covariates in tables 2 and 3, respectively (HRHLOS = 1.08, 95% CI = 0.94–1.24, P = 0.27; HRmortality = 1.58, 95% CI = 0.91–2.74, P = 0.10). This remained true when preoperative BNP was, in addition, included in the multivariable adjustments (HRHLOS = 0.99; 95% CI = 0.85–1.16, P = 0.92; HRmortality = 1.19, 95% CI = 0.66–2.17, P = 0.56).
Discussion
Elevations in BNP are known to predict morbidity and mortality in both ambulatory cohorts and noncardiac surgical populations.1–11,30–33 Preoperative BNP is also known to predict adverse outcomes after cardiac surgery, even after adjusting for known clinical risk factors such as preoperative left ventricular ejection fraction.13–15 However, the utility of postoperative plasma BNP for perioperative risk stratification has yet to be clearly delineated,12,16–22 particularly with regard to understanding the additional value it may provide over assessing preoperative BNP alone.
In the current study, after multivariable adjustment for preoperative BNP and clinical covariates, elevated peak postoperative BNP was a weak but significant predictor of HLOS and was not associated with mortality. In these same multivariable models, preoperative BNP independently predicted HLOS and approached being an independent predictor of mortality. The ability of the study’s multivariable clinical model to predict mortality was improved (as assessed by AIC) when preoperative BNP was added to the clinical model alone compared with when it was added to the clinical model together with peak postoperative BNP.
Although we hypothesized that peak postoperative BNP would add significantly to the utility of preoperative BNP and clinical risk factors for predicting HLOS and mortality after CABG surgery, our study results suggest that there is little added benefit to assessing peak postoperative BNP either instead of or in addition to preoperative BNP. Our HLOS results suggest a small additional predictive value that was derived from assessing peak postoperative BNP and preoperative BNP together compared with assessing preoperative BNP alone. However, we do not believe that this finding is sufficiently strong to warrant measuring both preoperative and peak postoperative BNP together for the purposes of risk stratifying primary CABG patients.
Another finding of our study is that when preoperative and peak postoperative BNP were separately entered into the multivariable clinical prediction models for HLOS and mortality, both the preoperative and the peak postoperative BNP measurements independently predict each study outcome. This indicates that peak postoperative BNP could be useful for postoperative risk stratification, particularly if a preoperative BNP measurement is not available. This also supports the findings of a recent smaller study of mixed cardiac surgical patients that did not adjust for preoperative BNP but did find that peak postoperative BNP significantly predicted occurrence of major adverse cardiovascular events during the first postoperative year, even after adjusting for subjects’ Euroscores.22 That study assessed postoperative BNP values immediately after surgery and on PODs 1 and 5, and, consistent with our findings, postoperative BNP was significantly more elevated at later postoperative time points.22 Approximately 20% of our primary CABG subjects were discharged on POD 5, and so assessing the peak of at least three POD 1–5 BNP measurements allowed us a high likelihood of capturing an approximate peak postdischarge measurement without limiting us to biases induced by assessing only the latest postoperative time points (i.e., assessing POD 5 BNP instead of peak postoperative BNP would have biased the analysis by eliminating those patients who did well enough to be discharged on POD 5 or earlier).
Although POD 1 BNP is clinically convenient to measure for immediate postoperative risk stratification, we found that it does not significantly predict HLOS and mortality after adjusting for clinical risk factors. This supports the findings of Provenchere et al.20 who reported that POD 1 BNP did not independently predict 1-yr mortality in a smaller cohort of CABG and valve surgery patients after adjusting for clinical risk factors. This suggests that future investigations of the predictive value of BNP measured after cardiac surgery should focus on peak postoperative BNP measurements. In our primary CABG cohort, peak postoperative BNP tends to occur later in the postoperative course (POD 3–5) after the initial postoperative rise in BNP release begins to plateau.
BNP cut-points for predicting adverse outcomes in various cardiac or general population cohorts are often substantially lower than BNP levels observed in patients with acute heart failure, suggesting that even mild elevations in BNP may reflect subclinical myocardial pathology that puts patients at risk beyond what can be predicted using clinical signs and symptoms alone.1,11,30 In our study, the CIs surrounding the HRs for peak postoperative BNP’s associations with HLOS and with mortality are wider than those surrounding the HRs for preoperative BNP. This reflects greater variation in the range of postoperative versus preoperative BNP measurements (fig. 1) and may explain why we found preoperative BNP to be a more significant predictor of both HLOS and mortality despite preoperative BNP having smaller associated HRs than those observed for peak postoperative BNP. Although our study’s findings suggest that preoperative BNP may be better than peak postoperative BNP for predicting HLOS and mortality, future studies of peak postoperative BNP that focus on prediction of longer term cardiac-specific outcomes such as heart failure may have narrower CIs surrounding HRs related to postoperative BNP, because the cardiac outcome is more strongly associated with peak postoperative BNP. Furthermore, although the areas under the ROC curves that we derived for the relationship between peak postoperative BNP and both extended HLOS and mortality (2.38 yr follow-up) indicate only moderate discriminatory ability of the peak postoperative BNP measurement, these areas are similar to the area under the curve reported by Fellahi et al.22 for the ROC curve relating peak postoperative BNP to occurrence of 1 yr postoperative major adverse cardiovascular events. Future studies of peak postoperative BNP in relation to development of longer term heart failure-specific outcomes may reveal improved areas under associated ROC curves. Results to date suggest that although peak postoperative BNP adds to what can be predicted by clinical risk factors alone, it should not be used as a “stand-alone” predictor of adverse outcome after CABG surgery but should be considered in conjunction with important clinical predictors.
Fellahi et al.22 recently reported significant improvement in 1 yr major adverse cardiovascular events prediction in 224 subjects undergoing elective CABG or valve surgeries when subjects’ Euroscores and peak postoperative BNP, cardiac troponin I, and C-reactive protein measurements were assessed together versus separately. One drawback to this multimarker approach is that the three measured biomarkers peak at different postoperative time points, necessitating the need for multiple postoperative measurements of three different postoperative biomarkers. The authors state that they did not analyze the value of simultaneous preoperative measurements of the three biomarkers because most of the preoperative biomarker assessments in their cohort were within the normal range and would, thus, warrant a larger sample size for assessment. The goal of our current study was to assess whether peak postoperative BNP added to what could be practically assessed by a single preoperative BNP measurement and routinely assessed clinical risk factors. However, given that we found preoperative BNP to be a more significant predictor of HLOS and mortality than peak postoperative BNP, a future study hypothesis could focus on the predictive value of simultaneous assessment of preoperative BNP, cardiac troponin I, and CRP measurements.
Several limitations of our study deserve consideration. First, this study included patients undergoing nonemergency primary CABG-only surgery with CPB. Therefore, caution should be taken in extrapolating these results to other surgical populations. However, the fact that perioperative BNP associates with HLOS and mortality in our study, even after excluding higher risk CABG patients, suggests that perioperative BNP can help to identify CABG patients who are at increased risk of adverse outcomes but who may not be clearly at risk based on clinical risk factors alone. Second, although we may not be able to completely account for institutional variations in perioperative management, we did statistically adjust for potential confounding related to institutional practice by including institution as a covariate in the study’s multivariable HLOS and mortality models. Third, there are multiple commercially available BNP and N-terminal proBNP assays. Although both BNP and N-terminal proBNP measurements generally correlate well with each other and both have been used successfully for perioperative risk stratification, the absolute values of BNP and N-terminal proBNP are not interchangeable.31,32 Furthermore, there is a variability in absolute values of measurements made with various commercially available BNP assays.33 Thus, although results of this study, particularly with regard to cut-points in peak postoperative BNP, should be considered specific to the BNP assay used in this study, future studies should focus on risk stratification cutoffs for different BNP and N-terminal proBNP assays in both primary CABG and other cardiac surgical cohorts. Fourth, although this is the largest study to date of the value of in-hospital postoperative BNP for risk stratification of cardiac surgical patients, it is possible that a much larger study with greater power might find that both preoperative BNP and peak postoperative BNP are independent predictors of up to 5-yr mortality. Finally, the outcomes of this study are limited to HLOS and all-cause mortality. Future studies may be warranted to assess the association between peak postoperative BNP and other longer term cardiac specific adverse outcomes such as development of postoperative heart failure, particularly because our HLOS results suggest that peak postoperative BNP may be able to detect additional intraoperative and postoperative cardiac insults that cannot be assessed using preoperative BNP.
Conclusions
Early identification of cardiac surgical patients at risk for developing shorter and longer term adverse postoperative outcomes is important for initiating and developing preventive therapies and interventions that improve patient outcomes. In this study of primary CABG surgery patients, preoperative BNP concentration seems to be better than peak postoperative BNP for predicting hospital stay or all-cause mortality after primary CABG surgery.
What We Already Know about This Topic
Preoperative B-type natriuretic peptide (BNP) predicts adverse outcomes after cardiac surgery
Postoperative BNP may reflect worsening cardiac function, but whether it provides additional prognostic value beyond assessment of preoperative BNP is uncertain
What This Article Tells Us That Is New
In more than 1,100 patients undergoing coronary artery bypass graft surgery, peak postoperative BNP adds little to the value of preoperative BNP measurement alone for predicting hospital stay and mortality
Acknowledgments
Supported by Biosite Inc., San Diego, California; Society of Cardiovascular Anesthesiologists Research Starter Grant, Richmond, Virginia (to Dr. Fox, Principal Investigator); Foundation for Anesthesia Education and Research Research Starter Grant, Rochester, Minnesota (to Dr. Fox, Principal Investigator); Dennis W. Jahnigen Career Development Scholars Award, American Geriatrics Society, New York, New York (to Dr. Fox, Principal Investigator); K23-HL068774 from the National Institute of Health grant, Bethesda, Maryland (to Dr. Body, Principal Investigator); the Department of Anesthesiology, Perioperative and Pain Medicine, Brigham and Women’s Hospital, and Division of Cardiovascular Anesthesia, Baylor College of Medicine, Texas Heart Institute, Saint Luke’s Episcopal Hospital, Houston, Texas.
The authors thank the outstanding contributory efforts of the CABG Genomics Research staff: Kutjim Bodinaku, M.D. (Research Assistant, Department of Anesthesiology, Perioperative and Pain Medicine, Brigham and Women’s Hospital, Boston, Massachusetts); Svetlana Gorbatov, M.P.H. (Research Assistant, Department of Anesthesiology, Perioperative and Pain Medicine, Brigham and Women’s Hospital); James Gosnell, R.N. (Research Nurse, Department of Anesthesiology, Perioperative and Pain Medicine, Brigham and Women’s Hospital); Sejfudin Kavazovic, B.A. (Research Assistant, Cardiovascular Research Division, Division of Cardiovascular Anesthesiology, Texas Heart Institute, Saint Luke’s Episcopal Hospital, Houston, Texas); Jai Madan, M.D., M.P.H. (Research Assistant, Department of Anesthesiology, Perioperative and Pain Medicine, Brigham and Women’s Hospital); and Charles Wellington, R.N., B.S.N., C.C.R.N.-C.S.C., C.V.R.N. II (Research Nurse, Cardiovascular Research Division, Division of Cardiovascular Anesthesiology, Texas Heart Institute, Saint Luke’s Episcopal Hospital). They also thank all the subjects who have participated in the CABG Genomics Program.
Footnotes
Presented at the American Society of Anesthesiologists 2009 Annual Meeting, New Orleans, Louisiana, Oral Discussion, October 20, 2009.
http://clinicaltrials.gov/show/NCT00281164. Accessed July 10, 2009.
References
- 1.Daniels LB, Maisel AS. Natriuretic peptides. J Am Coll Cardiol. 2007;50:2357–68. doi: 10.1016/j.jacc.2007.09.021. [DOI] [PubMed] [Google Scholar]
- 2.Maeda K, Tsutamoto T, Wada A, Mabuchi N, Hayashi M, Tsutsui T, Ohnishi M, Sawaki M, Fujii M, Matsumoto T, Kinoshita M. High levels of plasma brain natriuretic peptide and interleukin-6 after optimized treatment for heart failure are independent risk factors for morbidity and mortality in patients with congestive heart failure. J Am Coll Cardiol. 2000;36:1587–93. doi: 10.1016/s0735-1097(00)00912-8. [DOI] [PubMed] [Google Scholar]
- 3.de Lemos JA, Morrow DA, Bentley JH, Omland T, Sabatine MS, McCabe CH, Hall C, Cannon CP, Braunwald E. The prognostic value of B-type natriuretic peptide in patients with acute coronary syndromes. N Engl J Med. 2001;345:1014–21. doi: 10.1056/NEJMoa011053. [DOI] [PubMed] [Google Scholar]
- 4.Grabowski M, Filipiak KJ, Karpinski G, Wretowski D, Rdzanek A, Huczek Z, Horszczaruk GJ, Kochman J, Rudowski R, Opolski G. Serum B-type natriuretic peptide levels on admission predict not only short-term death but also angiographic success of procedure in patients with acute ST-elevation myocardial infarction treated with primary angioplasty. Am Heart J. 2004;148:655–62. doi: 10.1016/j.ahj.2004.04.023. [DOI] [PubMed] [Google Scholar]
- 5.Fonarow GC, Peacock WF, Horwich TB, Phillips CO, Givertz MM, Lopatin M, Wynne J. Usefulness of B-type natriuretic peptide and cardiac troponin levels to predict inhospital mortality from ADHERE. Am J Cardiol. 2008;101:231–7. doi: 10.1016/j.amjcard.2007.07.066. [DOI] [PubMed] [Google Scholar]
- 6.Bassan R, Tura BR, Maisel AS. B-type natriuretic peptide: A strong predictor of early and late mortality in patients with acute chest pain without ST-segment elevation in the emergency department. Coron Artery Dis. 2009;20:143–9. doi: 10.1097/MCA.0b013e3283292ac6. [DOI] [PubMed] [Google Scholar]
- 7.Harrison A, Morrison LK, Krishnaswamy P, Kazanegra R, Clopton P, Dao Q, Hlavin P, Maisel AS. B-type natriuretic peptide predicts future cardiac events in patients presenting to the emergency department with dyspnea. Ann Emerg Med. 2002;39:131–8. doi: 10.1067/mem.2002.121483. [DOI] [PubMed] [Google Scholar]
- 8.Maisel A, Hollander JE, Guss D, McCullough P, Nowak R, Green G, Saltzberg M, Ellison SR, Bhalla MA, Bhalla V, Clopton P, Jesse R. Primary results of the Rapid Emergency Department Heart Failure Outpatient Trial (REDHOT). A multicenter study of B-type natriuretic peptide levels, emergency department decision making, and outcomes in patients presenting with shortness of breath. J Am Coll Cardiol. 2004;44:1328–33. doi: 10.1016/j.jacc.2004.06.015. [DOI] [PubMed] [Google Scholar]
- 9.Doust JA, Pietrzak E, Dobson A, Glasziou P. How well does B-type natriuretic peptide predict death and cardiac events in patients with heart failure: Systematic review. BMJ. 2005;330:625–33. doi: 10.1136/bmj.330.7492.625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mega JL, Morrow DA, De Lemos JA, Sabatine MS, Murphy SA, Rifai N, Gibson CM, Antman EM, Braunwald E. B-type natriuretic peptide at presentation and prognosis in patients with ST-segment elevation myocardial infarction: An ENTIRE-TIMI-23 substudy. J Am Coll Cardiol. 2004;44:335–9. doi: 10.1016/j.jacc.2004.04.033. [DOI] [PubMed] [Google Scholar]
- 11.Schnabel R, Lubos E, Rupprecht HJ, Espinola-Klein C, Bickel C, Lackner KJ, Cambien F, Tiret L, Munzel T, Blankenberg S. B-type natriuretic peptide and the risk of cardiovascular events and death in patients with stable angina: Results from the AtheroGene study. J Am Coll Cardiol. 2006;47:552–8. doi: 10.1016/j.jacc.2005.09.039. [DOI] [PubMed] [Google Scholar]
- 12.Berendes E, Schmidt C, Van Aken H, Hartlage MG, Rothenburger M, Wirtz S, Scheld HH, Brodner G, Walter M. A-type and B-type natriuretic peptides in cardiac surgical procedures. Anesth Analg. 2004;98:11–9. doi: 10.1213/01.ANE.0000093249.35075.F1. [DOI] [PubMed] [Google Scholar]
- 13.Wazni OM, Martin DO, Marrouche NF, Latif AA, Ziada K, Shaaraoui M, Almahameed S, Schweikert RA, Saliba WI, Gillinov AM, Tang WH, Mills RM, Francis GS, Young JB, Natale A. Plasma B-type natriuretic peptide levels predict postoperative atrial fibrillation in patients undergoing cardiac surgery. Circulation. 2004;110:124–7. doi: 10.1161/01.CIR.0000134481.24511.BC. [DOI] [PubMed] [Google Scholar]
- 14.Gibson PH, Croal BL, Cuthbertson BH, Rae D, McNeilly JD, Gibson G, Jeffrey RR, Buchan KG, El-Shafei H, Hillis GS. Use of preoperative natriuretic peptides and echocardiographic parameters in predicting new-onset atrial fibrillation after coronary artery bypass grafting: A prospective comparative study. Am Heart J. 2009;158:244–51. doi: 10.1016/j.ahj.2009.04.026. [DOI] [PubMed] [Google Scholar]
- 15.Fox AA, Shernan SK, Collard CD, Liu KY, Aranki SF, DeSantis SM, Jarolim P, Body SC. Preoperative B-type natriuretic peptide is as independent predictor of ventricular dysfunction and mortality after primary coronary artery bypass grafting. J Thorac Cardiovasc Surg. 2008;136:452–61. doi: 10.1016/j.jtcvs.2007.12.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hutfless R, Kazanegra R, Madani M, Bhalla MA, Tulua-Tata A, Chen A, Clopton P, James C, Chiu A, Maisel AS. Utility of B-type natriuretic peptide in predicting postoperative complications and outcomes in patients undergoing heart surgery. J Am Coll Cardiol. 2004;43:1873–9. doi: 10.1016/j.jacc.2003.12.048. [DOI] [PubMed] [Google Scholar]
- 17.Cuthbertson BH, Amiri AR, Croal BL, Rajagopalan S, Brittenden J, Hillis GS. Utility of B-type natriuretic peptide in predicting medium-term mortality in patients undergoing major non-cardiac surgery. Am J Cardiol. 2007;100:1310–3. doi: 10.1016/j.amjcard.2007.05.058. [DOI] [PubMed] [Google Scholar]
- 18.Bail DH, Kofler M, Ziemer G. Brain natriuretic peptide (BNP) in patients undergoing coronary artery bypass grafting. Thorac Cardiovasc Surg. 2004;52:135–40. doi: 10.1055/s-2004-817875. [DOI] [PubMed] [Google Scholar]
- 19.Song M-H, Kobayashi Y, Michi H. Clinical implication of atrial and brain natriuretic peptide in coronary artery bypass grafting. Asian Cardiovasc Thorac Ann. 2004;12:41–6. doi: 10.1177/021849230401200111. [DOI] [PubMed] [Google Scholar]
- 20.Provenchere S, Berroeta C, Reynaud C, Baron G, Poirier I, Desmonts JM, Iung B, Dehoux M, Philip I, Benessiano J. Plasma brain natriuretic peptide and cardiac troponin I concentrations after adult cardiac surgery: Association with postoperative cardiac dysfunction and 1-year mortality. Crit Care Med. 2006;34:995–1000. doi: 10.1097/01.CCM.0000206110.94385.C4. [DOI] [PubMed] [Google Scholar]
- 21.Nozohoor S, Nilsson J, Luhrs C, Roijer A, Algotsson L, Sjogren J. B-type natriuretic peptide as a predictor of postoperative heart failure after aortic valve replacement. J Cardiothorac Vasc Anesth. 2009;23:161–5. doi: 10.1053/j.jvca.2008.11.006. [DOI] [PubMed] [Google Scholar]
- 22.Fellahi JL, Hanouz JL, Manach YL, Gue X, Monier E, Guillou L, Riou B. Simultaneous measurement of cardiac troponin I, B-type natriuretic peptide, and C-reactive protein for the prediction of long-term cardiac outcome after cardiac surgery. Anesthesiology. 2009;111:250–7. doi: 10.1097/ALN.0b013e3181a1f720. [DOI] [PubMed] [Google Scholar]
- 23.Collard CD, Shernan SK, Fox AA, Bernig T, Chanock SJ, Vaughn WK, Takahashi K, Ezekowitz AB, Jarolim P, Body SC. The MBL2 ‘LYQA secretor’ haplotype is an independent predictor of postoperative myocardial infarction in whites undergoing coronary artery bypass graft surgery. Circulation. 2007;116:I106–12. doi: 10.1161/CIRCULATIONAHA.106.679530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fox AA, Collard CD, Shernan SK, Seidman CE, Seidman JG, Liu KY, Muehlschlegel JD, Perry TE, Aranki SF, Lange C, Herman DS, Meitinger T, Lichtner P, Body SC. Natriuretic peptide system gene variants are associated with ventricular dysfunction after coronary artery bypass grafting. Anesthesiology. 2009;110:738–47. doi: 10.1097/aln.0b013e31819c7496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wahl HG, Graf S, Renz H, Fassbinder W. Elimination of the cardiac natriuretic peptides B-type natriuretic peptide (BNP) and N-terminal proBNP by hemodialysis. Clin Chem. 2004;50:1071–4. doi: 10.1373/clinchem.2003.030692. [DOI] [PubMed] [Google Scholar]
- 26.Das SR, Abdullah SM, Leonard D, Drazner MH, Khera A, McGuire DK, de Lemos JA. Association between renal function and circulating levels of natriuretic peptides (from the Dallas Heart Study) Am J Cardiol. 2008;102:1394–8. doi: 10.1016/j.amjcard.2008.07.018. [DOI] [PubMed] [Google Scholar]
- 27.Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: A new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med. 1999;130:461–70. doi: 10.7326/0003-4819-130-6-199903160-00002. [DOI] [PubMed] [Google Scholar]
- 28.K/DOQI clinical practice guidelines for chronic kidney disease: Evaluation, classification, and stratification. Am J Kidney Dis. 2002;39:S1–266. [PubMed] [Google Scholar]
- 29.Hsieh FY, Lavori PW. Sample-size calculations for the Cox proportional hazards regression model with nonbinary covariates. Control Clin Trials. 2000;21:552–60. doi: 10.1016/s0197-2456(00)00104-5. [DOI] [PubMed] [Google Scholar]
- 30.Wang TJ, Larson MG, Levy D, Benjamin EJ, Leip EP, Omland T, Wolf PA, Vasan RS. Plasma natriuretic peptide levels and the risk of cardiovascular events and death. N Engl J Med. 2004;350:655–63. doi: 10.1056/NEJMoa031994. [DOI] [PubMed] [Google Scholar]
- 31.Alibay Y, Beauchet A, El Mahmoud R, Schmitt C, Brun-Ney D, Benoit MO, Dubourg O, Boileau C, Jondeau G, Puy H. Plasma N-terminal pro-brain natriuretic peptide and brain natriuretic peptide in assessment of acute dyspnea. Biomed Pharmacother. 2005;59:20–4. doi: 10.1016/j.biopha.2004.06.002. [DOI] [PubMed] [Google Scholar]
- 32.Sanz MP, Borque L, Rus A, Vicente B, Ramirez Y, Lasa L. Comparison of BNP and NT-proBNP assays in the approach to the emergency diagnosis of acute dyspnea. J Clin Lab Anal. 2006;20:227–32. doi: 10.1002/jcla.20146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Apple FS, Wu AH, Jaffe AS, Panteghini M, Christenson RH. National Academy of Clinical Biochemistry and IFCC Committee for Standardization of Markers of Cardiac Damage Laboratory Medicine Practice Guidelines: Analytical issues for biomarkers of heart failure. Clin Biochem. 2008;41:222–6. doi: 10.1016/j.clinbiochem.2007.07.001. [DOI] [PubMed] [Google Scholar]