Abstract
Purpose
Total hip replacement (THR) is one of the most successful and cost-effective surgical procedures and remains the treatment of choice for long-term pain relief and restoration of function for patients with diseased or damaged hips. Acetabular fractures managed either conservatively or operatively by fixation tend to present later with secondary joint changes that require THR. In this study we evaluated the functional outcome and quality of life achieved by such patients.
Methods
Our study was carried out as a retrospective trial by recruiting patients who underwent THR from June 2006 to May 2012. A total of 32 patients were included with a mean age of 46.08 years ranging from (25–65) years. We evaluated the quality of life in the patients using scoring techniques of Short Musculoskeletal Functional Assessment (SMFA) and the 12-Item Short Form Health Survey (SF-12). Functional outcome was assessed using Harris Hip Score (HHS).
Results
The mean HHS of the patients was 84.3 with a range from 56 to 100. The SMFA averaged 13.3. The SF-12 score averaged 49.1. The correlation of the HHS with SF-12 was positive (p = 0.001) while with SMFA there was a negative correlation (p = 0.001).
Conclusion
From this study it is inferred that the functional outcome of THR and quality of life in patients who had acetabular fractures and were initially managed by open reduction and internal fixation is good.
Keywords: Arthroplasty, replacement, hip; Acetabulum; Fractures, bone; Fracture fixation, internal
Introduction
Total hip replacement (THR) is one of the most successful and cost-effective surgical option and remains the treatment modality of choice for long-term pain relief and functional restoration for patients with diseased or damaged hips. THR is frequently advised and regularly performed for patients who suffered femoral neck fracture, femoral intertrochanteric fracture and acetabular fractures. Acetabular fractures managed either conservatively or operatively by fixation tend to present later with secondary joint changes that require THR. Seventy-two percent of patients with poor reduction and thirty percent with good reduction develop this complication.1 Such patients form a high number of cases undergoing THR in India as per records.2 The lack of traffic sense, poor condition of roads and not wearing seat belts3 could be the reason for acetabular fractures. The soft tissue condition, the previous implant used, the bone stock deterioration, the anticipated bleeding due to fibrosis, all owing to the primary surgery make subsequent THR difficult and may have a call on the final outcome. In the present study, we evaluated the functional outcome and quality of life achieved by such patients.
Materials and methods
The present retrospective trial was carried out by recruiting patients who underwent THR from June 2006 to May 2012, following acetabular fractures that were primarily managed by open reduction and internal fixation. A total of 32 patients were included with a mean age of 46.08 years ranging from (25–65) years. The males formed the majority of cases (n = 28). We evaluated the quality of life in the patients using scoring techniques of Short Musculoskeletal Functional Assessment (SMFA) and the 12-Item Short Form Health Survey (SF-12). The SMFA score of less than 20 means a good quality of life, between 20 and 40 is fair and more than 40 is poor.4 SF-12 scores greater than 50 represent above average health status.
Functional outcome was also assessed using Harris Hip Score (HHS). The functional outcome is considered poor if score is less than 70, fair when between 70 and 79, good when between 80 and 89 and excellent when above 90.5 We also established a correlation between the HHS and the SMFA and SF-12 scores. Normally distributed data were analysed with analysis of variance followed by Tukey's honestly significant difference Test. Non-normally distributed data were analyzed with Kruskal–Wallis test. A p value < 0.05 was considered statistically significant.
Results
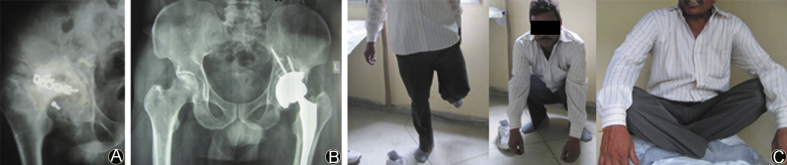
The mean HHS of the patients was 84.3 with a range from 56 to 100 and standard deviation of 13.79. Hence, the functional outcome in the patients in the present study on an average was good (Fig. 1, Fig. 2).
Fig. 1.
A 42-year-old male with a history of road side accident causing fracture in left acetabulum that was fixed 3 years back in 2006 (A). He presented with complains of pain and difficulty in walking. He had 2.5 cm of shortening with rotations at hip restricted. He received THR on August 7, 2009 (B). On follow up he presented with good functional status with optimum hip range of movements (C).
Fig. 2.
In January 2007, a 60-year-old male presented with secondary osteoarthritis in left hip, after acetabular fracture had been fixed surgically in 2005. He had complains of pain and restriction of movements. Cemented THR was done on January 1, 2007 (A). On follow up in August 2013, patient was pain free with HHS of 100 on the left side and he was in good spirit with excellent quality of life (B).
The SMFA averaged 13.02 with standard deviation of 13.27. The SF-12 score averaged 49.1 with a standard deviation of 11.36. We combined the physical and the mental component scores in the latter and then calculated the mean score. The Pearson's correlation of the HHS with SF-12 was positive (p = 0.001) while with SMFA there was a negative correlation (p = 0.001).
Discussion
Males form the majority of THR cases according to studies by Pachore et al2 and Dhaon et al.6 The present study too confirms their overwhelming majority (7:1). In India, males are much more victims of road traffic accidents than females. The conventional trend of males in families earning a livelihood and travelling for work, while females being home makers, make the former more susceptible to accidents. This probably explains the high sex ratio in the present study. The relatively younger age group of these patients requires them to lead a more active life and achieve a better functional status to lead a fruitful life. Whether or not such a degree of functional well-being and quality of life is achieved by THR in them, is the aim of the present study.
We used validated scoring techniques of SF-12 and SMFA score to assess the quality of life in our patients.
SF-12 score is inclusive of physical and mental component scales. It basically is composed of a 12 item self-administered personal interview. It has been validated as a useful tool previously by Ostendorf et al7 and Kontodimopoulos et al.8 It was used in assessing the functional outcome of THR in steroid induced avascular necrosis of hips by Rahman et al.9
SMFA score is basically a single point score of the physical status of the patient and quantifies the functional status of patients with broad range of musculoskeletal injuries and disorders. It has been validated by Wollmerstedt et al10 and Kirschner et al11 finding it to possess high reliability and recommended its use. Taylor et al12 in 2012 used it to assess outcome of hemiarthroplasties in femoral neck fracture in elderly patients. A higher score indicates a worse outcome.
To assess the functional outcome, we use the technique of HHS that has been used previously in various studies13, 14, 15, 16 evaluating outcomes of THR. It is a tool to measure the functional capacity of an individual that has been used to assess the condition of a patient with hip pathology before and after surgical or conservative management. It has been validated by Söderman et al17 and Hoeksma et al18.
The mean HHS of the patients in the present study is 84.3. As per grades by Marchetti et al,5 the functional outcome in our patients is good (80–90). The average SMFA score of 13.3 shows the quality of life achieved to be good.1 The SF-12 of the average population is around 50. The score achieved in this study after combining the mental and physical scores is 49.1, near to the average value. So, it can be said that THRs that were done in this study provided the patients with a good quality of life and functional outcome.
We statistically correlated the functional score and the quality of life scores and the results showed that patients with good functional outcome also have a good quality of mental and physical lives.
In our study, functional outcome of THR in patients who had previous, ipsilateral acetabular fractures and were initially managed by open reduction and internal fixation is good. The quality of life in such patients is good and is close to the average population. Patients with good functional outcome should also have a good quality of life as both are correlated.
A single, vastly experienced and technically sound, senior arthroplasty surgeon performed all the surgeries offsetting any technical factors affecting the result. Also, a single investigator who was not involved at any time during surgical procedure collected all the data. Also multiple scoring techniques were used strengthening the study.
Being a retrospective study, we do acknowledge the limitations of this study. The pre-operative scores were not evaluated and the difference in technique with use of cement or meshes in some cases, were not documented. Further this is a short term study. So, we warrant further studies with longer follow ups preferably in a prospective fashion for better evaluation of such patients.
Footnotes
Peer review under responsibility of Daping Hospital and the Research Institute of Surgery of the Third Military Medical University.
References
- 1.Tile M. Springer-Verlag; New York: 1996. Fractures of the Acetabulum. [Google Scholar]
- 2.Pachore J.A., Vaidya S.V., Thakkar C.J. ISHKS joint registry: a preliminary report. Indian J Orthop. 2013;47:505–509. doi: 10.4103/0019-5413.118208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dakin G.J., Eberhardt A.W., Alonso J.E. Acetabular fracture patterns : association with motor vehicle crash information. J Trauma. 1999;47:1063–1071. doi: 10.1097/00005373-199912000-00012. [DOI] [PubMed] [Google Scholar]
- 4.Badra M.I., Anand A., Straight J.J. Functional outcome in adult patients following Bernese periacetabular osteotomy. Orthopaedics. 2008;31:69. doi: 10.3928/01477447-20080101-03. [DOI] [PubMed] [Google Scholar]
- 5.Marchetti P., Binazzi R., Vaccari V. Long-term results with cementless Fitek (or Fitmore) cups. J Arthroplast. 2005;20:730–737. doi: 10.1016/j.arth.2004.11.019. [DOI] [PubMed] [Google Scholar]
- 6.Dhaon B.K., Jaiswal A., Nigam V. Noncemented total hip replacement in various disorders of the hip. Indian J Orthop. 2005;39:225–227. [Google Scholar]
- 7.Ostendorf M., van Stek H.F., Buskens E. Patient reported outcome in total hip replacement. A comparison of five instruments of health status. J Bone Jt Surg Br. 2004;86:801–808. doi: 10.1302/0301-620x.86b6.14950. [DOI] [PubMed] [Google Scholar]
- 8.Kontodimopoulos N., Pappa E., Niakas D. Validity of SF-12 summary scores in Greek general population. Health Qual Life Outcomes. 2007;5:55. doi: 10.1186/1477-7525-5-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rahman W.A., Garbuz D.S., Masri B.A. Total hip arthroplasty in steroid-induced osteonecrosis: early functional and radiological outcomes. Can J Surg. 2013;56:41–46. doi: 10.1503/cjs.032510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wollmerstedt N., Kirschner S., Wolz T. Evaluating the reliability, validity and responsiveness of the German short musculoskeletal function assessment questionnaire, SMFA-D, in inpatient rehabilitation of patients with conservative treatment of hip osteoarthritis. Rehabil (Stuttg) 2004;43:233–240. doi: 10.1055/s-2004-828294. [DOI] [PubMed] [Google Scholar]
- 11.Kirschner S., Walther M., Mehling E. Reliability, validity and responsiveness of the German short musculoskeletal function assessment questionnaire (SMFA-D) in patients with osteoarthritis of the hip undergoing total hip arthroplasty. Z Rheumatol. 2003;62:548–554. doi: 10.1007/s00393-003-0514-y. [DOI] [PubMed] [Google Scholar]
- 12.Taylor F., Wright M., Zhu M. Hemiarthroplasty of the hip with and without cement: a randomized clinical trial. J Bone Jt Surg Am. 2012;94:577–583. doi: 10.2106/JBJS.K.00006. [DOI] [PubMed] [Google Scholar]
- 13.Chiu H.C., Mau L.W., Hsu Y.C. Postoperative 6-month and 1-year evaluation of health related quality of life in total hip replacement patients. J Formos Med Assoc. 2001;100:461–465. [PubMed] [Google Scholar]
- 14.Nath R., Gupta A.K., Chakravarty U. Primary cemented total hip arthroplasty: 10 years follow-up. Indian J Orthop. 2010;44:283–288. doi: 10.4103/0019-5413.65152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.He A.S., Li F.B., Liao W.M. Outcomes of cementless total hip arthroplasty in treatment of osteoarthritis. Chin J Reparative Reconstr Surg. 2003;17:442–445. [PubMed] [Google Scholar]
- 16.Chong R.W., Chong C.S., Lai C.H. Total hip arthroplasty in patients with chronic autoimmune inflammatory arthroplasties. Int J Rheum Dis. 2010;13:235–239. doi: 10.1111/j.1756-185X.2010.01477.x. [DOI] [PubMed] [Google Scholar]
- 17.Söderman P., Malchau H. Is the Harris hip score system useful to study the outcome of total hip replacement? Clin Orthop Relat Res. 2001;384:189–197. doi: 10.1097/00003086-200103000-00022. [DOI] [PubMed] [Google Scholar]
- 18.Hoeksma H., Van den Ende C.H., Ronday H.K. Comparison of the responsiveness of the Harris Hip Score with generic measures for hip function in osteoarthritis of the hip. Ann Rheum Dis. 2003;62:935–938. doi: 10.1136/ard.62.10.935. [DOI] [PMC free article] [PubMed] [Google Scholar]