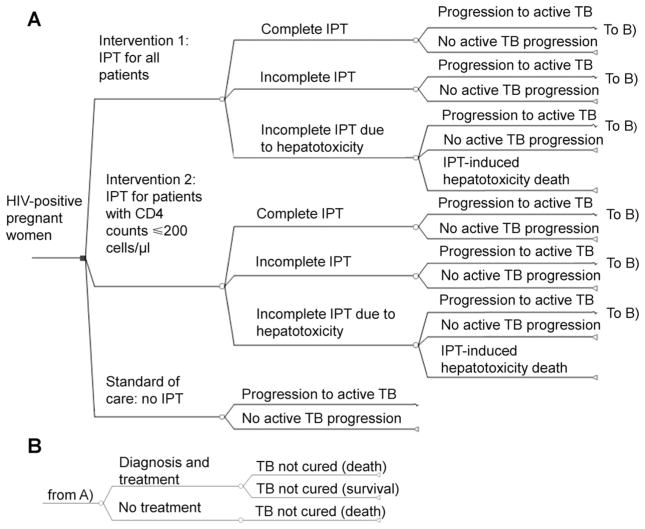
Figure 1.
Schematic diagram of decision analysis model: simplified schematic of decision tree model. The target population was HIV-infected pregnant women. We assumed provisions for ART and knowledge of CD4+T-cell count. In all model arms, the proportion of patients progressing to active TB was affected by baseline latent TB (TST) status, CD4 count, and usage of IPT. In the base-case intervention arms, women are given IPT irrespective of TST status, but we explored TST-driven strategies in secondary analysis. We included progression to active TB among patients with a negative baseline TST (lower proportion than for TST-positive) to account for imperfect test sensitivity and possibility of infection at time points after model entry. For the IPT interventions, we accounted for reduced efficacy with incomplete adherence, and incorporated costs and effects of IPT-induced hepatotoxicity. In all arms, we assumed that patients developing active TB could be diagnosed and treated based on current case-detection and treatment rates in India. HIV-infected pregnant women with undiagnosed and untreated active TB were assumed to die. HIV =human immunodeficiency virus; IPT =isoniazid preventive therapy; TB =tuberculosis; ART =antiretroviral therapy; TST = tuberculin skin test.