Abstract
IAPT (Improving Access to Psychological Therapies) is a national programme aimed at increasing availability of evidence based psychological therapies in the NHS. IAPT is primarily for people who have mild to moderate, common mental health difficulties such as depression, anxiety, phobias and post traumatic stress disorder (PTSD). The programme seeks to use the least intrusive method of care possible to treat people at the time when it will be of most help to them. Individuals are able to self-refer into most IAPT services or alternatively can request to be referred by their GP or other services in the community.
Richmond Wellbeing Service (RWS) is one such IAPT Service and this research is based on our work to promote accessibility of the service to one of the harder to reach population groups - older adults. We know that IAPT services could have a positive impact on older adults as it is believed on average, 25% of over 65 year olds face common mental health problems. However, only a third of these people discuss this with their GP and so are less likely to be referred to an IAPT Service.
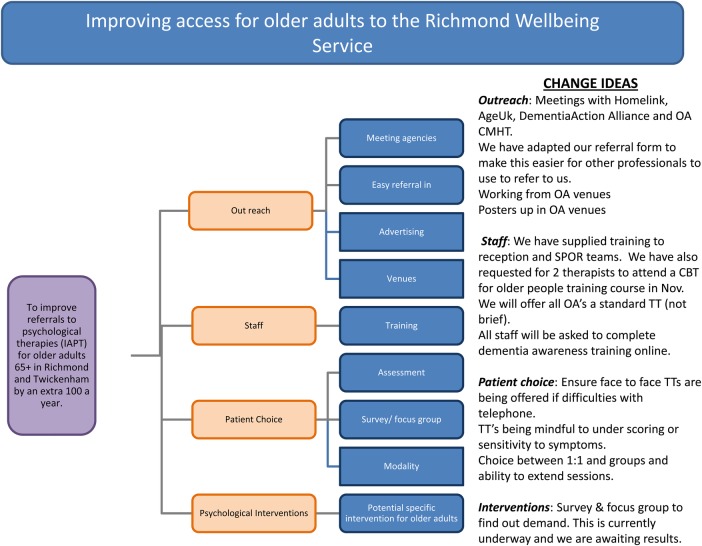
In relation to the above, this project was designed to look at increasing access for older adults into Richmond Wellbeing Service (RWS) specifically to improve access to the RWS by older adults by 100. The overall goal was to increase older adult (65+) referral rates by 20% over a year, in raw number this would translate to an increase of 100 over a year period, and in percentage terms an average of 8% of total referrals.
Results yielded an increase of 39 referrals between baseline and test period. The majority of this increase had occurred in the final five months of the projects duration(31). Interestingly the number of older adults in the older age band (85+) almost doubled within this period (from 12 to 21). In total, in percentage terms this translates to an an increase of OA referrals from 6% up to 6.7%, as above we are aiming for 8% or an additional increase of 61 patients. Thus during the duration of the project there were signals of an increase in the desired direction, as the number of OA referrals increased following the period of time the interventions were implemented. However referral rates did not fully reach the target set.
The authors concluded that sustainable and meaningful change in improving access for older adults into an IAPT service is possible but does take time. (Alongside the increase of referral a continous assessment of quality is required and where neccessary improve upon the appropriateness of the service offered to Older adults).
Problem
The IAPT programme is available to all adults in England. Despite this, older adults are being under represented and IAPT services have been criticised for not adequately addressing this issue.1 2
We know that IAPT services could have a positive impact on older adults.2 It is believed that one in four older people have a common mental health problem but that fewer than one in six discuss their symptoms with their GP.3 The risk of depression, for example increases with age and 40% of adults over 85 years are affected. There is good evidence for the effectiveness of psychological therapies for treatment of common mental health problems.3 4
We therefore feel through this project we could make positive changes if we could find and demonstrate successful ways to engage with older adults and this could also be helpful for other IAPT sites.
The joint commissioning implementation plan for adults and older people have identified that a key area to improve is the take up of IAPT services by older adults (65 years plus). A target has been set for the Richmond Wellbeing Service (RWS) to improve our current referral rate by 20% within the next year. This would be an extra 100 referrals a year.
In looking at increasing access it is also important to assess the quality and appropriateness of treatment we offer at the RWS for older adults.
Our aim therefore is to improve access to the RWS by older adults by 100 a year and to improve upon the appropriateness of the service offered to Older adults.
Background
Most research to date focuses on access to service, rather than suggestions for changes to treatment.
Research has found that older adults are under referred to psychological services for reasons outlined above. Research which has focused on the type of psychological support which should be offered to older adults has come to a general consensus that older adults should be offered the same type of interventions as other age groups but with some modifications based on individual circumstance.
This is linked to Mohlman and Gorman's (2005) research looking at the use of patients executive functioning (EF), which they hypothesised that the efficacy of CBT (Cognitive Behavioural Therapy) was partly dependant on.5 They described EF as a set of cognitive abilities including allocation of attention and generation of hypothesis which are essential in completing workbooks and homework tasks. For example if using thought restructuring exercises, patients challenge thoughts by finding evidence for and against and generating new thoughts all the while self-monitoring the key five areas and mood ratings. CBT was therefore described as teaching patients to increase and refine their use of EF. Mohlman and Gorman's (2005) paper found, as they predicted that older-adults are more likely to have reduced EF skills, and they feel this is the link to why older-adults are at increased risk for CBT nonresponse. This therefore highlights the importance of thinking of ways to adapt the CBT deliverance to meet the needs of older-adults who may be suffering with reduced EF, rather than just accepting it as a barrier to change. The findings highlight that older-adults may experience difficulties in retaining information and in formulating hypotheses to challenge; as this is a key part of the CBT interventions it supports the best practice recommendation to increase time supporting older-adults.
Other research as summarised in How to make IAPT more accessible to Older People1 and IAPT Older People Positive Practice Guide2 have suggested the following modifications to standard intervention dependent upon each individual older adults circumstance:
Flexibility: IAPT services are encouraged to take a flexible approach to working with older adults. The main suggestions to help us become more flexible are to offer appointments across a range of times and days with consideration given to the venues we can offer. It is also recommended there is a potential for the inclusion of carers to be present where appropriate and helpful.
Sessions: This report suggests we allow for longer sessions for older adults, with additional practitioner support.
Isolation and advertisement: There is a high amount of social isolation within the older adult community. It is therefore vital IAPT services make every effort to be accessible. This also raises the question about how and where to promote the service to help reach potential clients who are isolated. The report does not give any more specific advice other than IAPT services should advertise in meaningful ways.
Physical health: Service providers must be aware that older adults' needs are complex and often need both physical and mental health care. IAPT services must therefore be flexible in recognising and responding appropriately to these needs.
Choice: The best practice guide highlighted the importance for older adults to have the same choice of therapy as younger adults do.
Referral routes: IAPT services need to work to make referral routes into the service more effective. In doing this consideration is needed to be given into different services and ways they can refer to us. A suggestion given is to make referrals from social services easier as other professionals such as social workers and care home staff can play an important role in identifying need. We also need to identify current successful and unsuccessful referral pathways.
Service user involvement: In order to make changes to attempt to improve access, involving older adults within this is recommended.
Training: The report encouraged IAPT staff to have specific training on working with older adults.
Baseline measurement
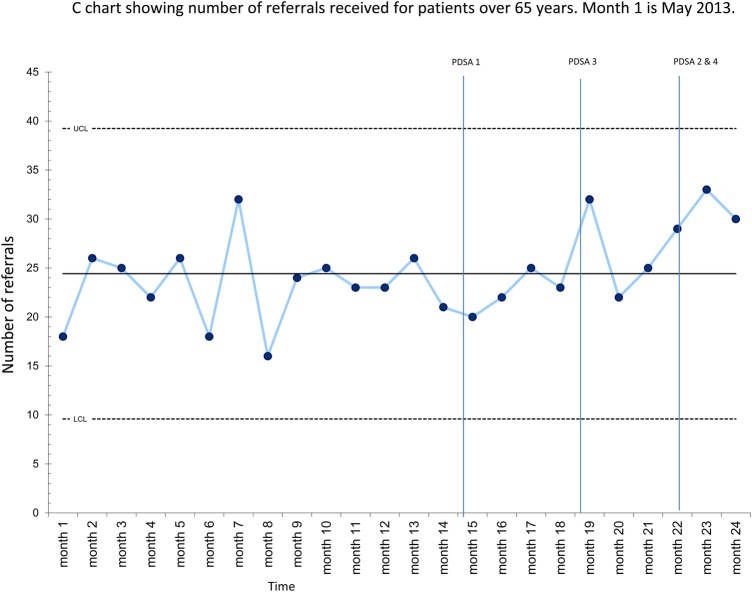
Our baseline data has been gathered and analysed from IAPTUS, the database used in the service. From this data we have established through analysis of descriptive data that our baseline, that is number of OA (older adult) referrals the previous year (ie May 2013 – April 2014).
For this project our main measure was the number of referral of older adults over a specified period (May 2014-April 2015 compared with May 2013-April 2014).
Directly linked to quality improvement secondary measures used as part of this project is quantitative and qualitative analysis of responses to our survey sent out to our current service users over 65 with the purpose of examining their views of our current service provision as well as ideas on how to make the referral process accessible for the OA age group. A large group of current and past OA were approached with a semi structured questionnaires enquiring about their experience of our service, the interventions offered as well as ease of finding us. (Appendix 1)
As part of this a qualitative analysis will be conducted on the open ended responses to the semi structured questionnaire.
The main measures used as part of this project are directly linked to the aims of the project, namely; to improve referral rates by 20% from older adults (over 65) over a year period (May 2014-April 2015). This would represent an increase from just under 6% of all referrals to 8% or an additional 100 referrals of people over 65 years of age (OA) across the period.
Our prediction is that we will see an increase in number of OA referrals at the end of the specified period.
Throughout our project we completed many PDSA cycles which have been described within the strategy section of this report.
Design
When considering the different reasons as to why fewer OA are referred into our service as compared to other age groups, we came up with five areas for further consideration. Firstly, that tertiary and third sector organisations working with OA may not know about our service and/or our referral criteria. Secondly, that IAPT advertising might not reach older adults. Thirdly, that the interventions that we offer to OA might not be relevant or interesting to them. Next, that there might be difficulties with geographical access. Finally, that staff at RWS might need further training in working with OA and potentially other services, especially those not focused on MH may benefit from training from us.
Based on the above considerations our main intervention as part of this project has been;
Survey to older adults who have used our service
Our first project was to look at what the experience, attitudes, and advice previous OA service users who have accessed our service hold. We therefore searched on our patient information system (IAPTus) for all previous service users who had contacted us or been referred who were over 65.
With support from the senior management team a questionnaire was devised asking clients to comment on six questions; Gender, Age, preference for groups between mixed ages, groups for over 65 year olds or would not attend groups, what issues were most relevant to them including low mood, anxiety, isolation, and several others with an option to add in any other, what their experience was like of finding out about us and accessing us, and what they thought we could go to encourage more OA's to access our service.
We sent out a stamped, addressed envelope to return the survey to us and an online Survey Monkey link for it to be completed online if wished.
This intervention took a large resource in terms of staff time and cost. The estimated cost of the postage was £196 and administration staff entered all the postal responses into Survey Monkey and two clinicians evaluated the outcomes.
Out-reach work
We felt an important area to tackle was looking at our links to other services in the borough. We identified three key services we wished to focus on; AgeUK, Older Adult CMHT, and homelink, a local service which offers nurse-led day respite care for adults.
Initially we made contact with the services to arrange a time to meet with them and discuss our service and whether they had links to clients that could benefit from our service. From these we were able to think more about how we can develop our proposed interventions. For example we were able to see how our referral pathways may not have been clear or could be made even more streamlined to help in making referrals easier and we have devised a screening tool to ease self-referral from these venues.
This intervention of building awareness of our service and relationships will need to be continued beyond this project. For example, we are working towards developing a poster for relevant older adult venues. It was further noted that the initial making of contact and meeting with organisations takes more resource then will be ultimately needed to maintain an ongoing outreach programme.
Staff training and dissemination to other services
Two members of staff (one from low intensity and one from high intensity) attended training specifically looking at CBT for older adults. Both clinicians then disseminated this down to the teams about best practice advice for working with older adults in the form of clinical skills sessions.
Through our second intervention, out-reach work, we also arranged a ‘no health without mental health’ talk to carers of clients using Homelink to help increase awareness of mental health in the public especially those likely to be older adults themselves or those caring for older adults.
Through this training we also agreed to pilot a 12-week depression group in the high intensity part of the service for OAs. This took a high intensity clinicians time as a resource (90 mins for 10 weeks) however the group is already established so we did not have to adjust or create a group package for these sessions.
Referral pathways clarification with other organisations
In meeting with services as part of our second intervention we were able to clarify our referral pathways. In doing so we realised a need for a simple referral from that a professional could make on an older adults behalf which we produced and sent. We also developed and discussed a screening questionnaire to also help other professionals identify older adults who may benefit from our input.
Strategy
The PDSA's are oulined in appendix 2 and thus refer to:
PDSA 1
Outreach – meetings with our services (amended referral form, promotion of our material establishing referral pathways)
PDSA 2
Responding to survey – offering specific interventions to older adults.
PDSA 3
Piloting a OA Depression Group (see supplementary file “PDSA(1–3)”)
bmjqir.u206099.w2510supp.pdf (219.8KB, pdf)
Results
Analysis of the data provided by survey responses in relation to question 1 pertaining to group inclusion confirmed that 51% of responders would prefer a mixed age group, 21% would prefer groups for over 65 age group only, and 28% said that they would not consider attending a group treatment. Data suggested that responders over the age of 75 years seemed most likely to prefer groups of mixed age attendees.
The second question on the survey asked responders to state which difficulties were most relevant to them. 71% of responders confirmed that anxiety and worry were of most relevance and 53% confirmed that low mood was more relevant.
We completed qualitative analysis of the open ended questions; 3) what was your experience of finding out about our service and accessing us; and 4) what could we do to encourage more people over 65 years of age to access our service?
The most frequently reported response to question 3 was that responders had been referred by their GP and that the process was easy, efficient, helpful, and good (17 responders). Another theme was that responders found the RWS team to be helpful and friendly (10 responders), which was interesting as the question had not specifically implied an interest in this.
We collated responders suggestions in respect of question 4 above and linked themes of service advertising, advertising through outreach work, and presentations and generally providing more accessible information about the service. In addition, responders referred to the importance of addressing stigma, including hope and normalising the process of seeking help for mental health difficulties. Others also suggested that we provide additional information specifically aimed at our provision for older adults. There was also mention of the lack of provision for individual therapy. RWS initially offering group interventions to patients on a stepped care basis. As previously mentioned, there was no clear majority for age specific interventions and indeed responders indicated that opinions were divided in this regard.
In summary, the data suggested that more older adults would opt for group interventions but, for some, a group intervention would not be considered as an acceptable treatment option.
ANALYSIS OF REFERRAL RATES:
The overall goal specified in our driver diagram was to increase older adult referral rates by 20% over a year, in raw number this would translate to an increase of 100 over a year period, and in percentage terms an average of 8% of total referrals.
Our results so far yields the following:
An increase of 39 referrals between the baseline and test period can be observed.
The majority of the increase has occurred over the last 5 months (31).
Number of older adults in the older age band (85+) has almost doubled within this period (from 12 to 21).
In percentage terms this translates to an an increase of OA referrals from 6% up to 6.7%, as above we are aiming for 8% or an additional increase of 61 patients.
As can be seen there are signals that the system is performing better. With time and continued attention and development of the older adult strategy which will continue beyond this project a sustained improvement of referral rates should be achievable.
Lessons and limitations
From our project we were pleased to see that OA referrals had increased following the period of time we implemented our intervention. Throughout the process of focusing on OA referrals and implementing change ideas we discovered road-blocks we had not predicted as well as new ideas of how to improve OA's access to primary care mental health services.
Below are our main areas of intervention and some reflections and learning from these:
Survey to older adults who have used our service
We had a good response rate to this survey, much higher than predicted. This therefore meant it was a bigger piece of work for administrators to input findings as well as the two clinicians working on this project to analyse the results and pull meaningful outcomes from it.
One of the most prominent findings from the survey which supports this type of improvement project is the majority of OAs who had used our service reported positively of the support offered and responded well to CBT focussed treatments. This finding from a large majority of our survey helped when thinking about out-reach work and promoting this type of treatment for common mental health problems in later life.
Out-reach work
We realised through this project that connecting with other services takes time, not only to make those links but to build relationships and confidence in the service.
We also discovered from talking to other services that many wanted to refer clients with mental health problems but also had a diagnosis of dementia. This highlighted a problem for us at commissioning level as a potential gap in services. Although this was not something we were able to resolve with services at this point it was a helpful conversation and one we were able to pass up to the senior management team to consider at a commissioning level.
Understandably however this was frustrating for other services who felt like their clients with dementia would benefit from the treatments offered through the service.
Although we had set a target of 100 extra referrals a year, we did not hit this. This was helpful to see that change takes time especially when looking at building relationships with other services. Over this project we gained a greater appreciation of how long this type of change idea can take to embed itself and so we gained a more realistic idea of what an appropriate target should be for this type of time period. However if this theory is to be true, if as a service we continue promoting our service and nurturing relationships with other services, we should see our referrals steadily increase and be maintained at a higher level.
Overall however from our out-reach work we saw that OA access is taken seriously across the borough and therefore we received support from other agencies and services in our aim to increase access. We also found by making links new ideas were generated such as running some of our treatment groups from an OA services' venue which would help us access carers of those with dementia, often themselves over 65 years of age.
Staff training and dissemination to other services
We found training into CBT for older adults was widely offered and gave helpful insights into working with older adults. One of the key messages was that the standard CBT treatments work well with OAs, and although some adaptations may be needed including longer assessments to gain a full formulation, that the same treatments work well. This was also supported by our findings from our survey.
From our out-reach work we also identified a need to support other professionals and carers in recognising common mental health problems in those they are working with or supporting. At the start of our project this was not a change idea we had identified however through seeing the importance of not only building relationships but building knowledge of the clients we were hoping to reach we offered a session to a local respite care service. Following from this session which was delivered to carers we had a lot of interest verbally expressed in the service and we anticipated to receive referrals from these clients.
We hope further outreach work in the format of training will grow an interest in mental health problems and help professionals identify these earlier and refer to our service. We also hope our screening questionnaire designed will aid this also.
Referral pathways clarification with other organisations
Again through our liaison work we were able to see the areas we could improve on for our referral pathways. We found it was helpful to liaise with services who would be using these referral routes to get their feedback.
Conclusion
Our project aimed to increase access of OAs to our primary care talking therapies service. We focused on four key areas; 1) Survey to older adults who have used our service, 2) Out-reach work, 3) Staff training and dissemination to other services, and 4) Referral pathways clarification with other organisations.
Although we did not hit our aim which was to increase referrals by 100 a year, we have increased referrals by 36 with the majority coming from over 85 year olds and through reflecting on the aim during the period of the interventions we feel this is a success and acknowledge that it will take longer and continual focus to help increase this further and maintain that change.
The main things we learnt and we feel are important to remember are that OAs with common mental health problems can benefit from the treatment offered in our service and so focusing on improving access is therefore an important area for our service, and services like ours to work on.
The IAPT best practice guide for OA's did stress the importance of referral pathways and with this we focused on our links with other services to increase awareness of us, improve our image and so to find ways to improve our referral pathways. We learnt that this is a very important area for improving access and became the main focus of our project and one change that we will be able to sustain going forward. We did find however how building relationships takes time and effort. Therefore for this initial success to be continued and maintained the service will need to prioritise this commitment and allow the time for an OA champion to maintain these relationships.
We also learnt that just knowing about a service is not enough. We found from meeting with potential clients they required re-assurance and encouragement to make referrals. A common concern from the clients we spoke to was that they would be taking the space away from someone who needed it more than them or that their difficulty did not warrant free NHS treatment. This highlights a bigger issue of general mental health awareness and potentially could be looked at in our services' advertising going forward.
In terms of what we offer as a service for OA's there were mixed findings between an age specific group, mixed aged groups and no groups. On trialing an older adult group with five members focusing on low mood the results of the group were positive with 4/5 recovered on the PHQ-9 and GAD-7 however whether this result was influenced by the specificity of the group remains unclear.
In fact the responses of the OAs in the group with regards to preference of OA specific or mixed group echoes that of the larger scale of the survey with approximately half preferring OA group and half mixed. Again, being adaptable and able to individualise care for older adults will be something that we are able to sustain going forward.
Of note is that all participants in this group were over the age of 80, and some had hearing difficulties. As suggested by available guidelines (Dep of Health, IAPT) adaptation to group was made in that the facilitator allowed more sessions to allow for a slower pace, repetitions and discussions. This worked well in this group and allowed for a more effective delivery of material than if it would have been a mixed group.
It is therefore reasonable to hypothesise that while opinions regarding preference of age specific group may be divided from a service delivery point of view this may be beneficial and more cost effective. If we are serious in offering choice and an OA group would be appropriate this would also potentially address the issue of isolation which is a strong contributing factor to depressions in this age group.
We also considered throughout this project whether the term OA should be considered from 75 not 65. We found from our survey that people who are 65 do not always identifying as older adults. Interestingly with our project focusing on OAs we actually mainly increased access for over 75s even though we were directing it in theory for over 65s.
We also reflected that finding out why people we predict have MH problems are not accessing our service is a difficult thing to do. We found a lot of our change ideas were generated from staff working within the field of mental health and we will continue to ensure that we have clinicians networking within these areas going forward. Even involving OAs who had used our service to see how we can reach more OAs can be difficult. We appreciate this issue can affect many services like ours for many different populations of groups of people so overall we feel the progress we have started to make is a success but we acknowledge continual focus and work to maintain this will be needed.
Going forward, we will continue to build on our learning from our outreach work, developing new and better ways to promote access to RWS by ensuring that other sector specialist workforce understand and are able to integrate psychological therapies into their thinking when considering the needs of the older population. We will continue to network and work from their premises when able and listen to and incorporate their feedback as appropriate.
Acknowledgments
We wanted to acknowledge the support that we received from Homelink Day Respite Centre in Whitton and we specifically thank Sue Hodder, the Chief Operations Officer. Sue provided her extensive experience of working with older adults and acted as liaison between Richmond Wellbeing Service and service users on many occasions and continues to do so. In addition, we have been welcomed to work from the Homelink premises.
Footnotes
Declaration of interests: Nothing to declare.
Ethical approval: This quality improvement project did not require ethical approval because it did not deviate from normal clinical practice. There was no additional burden imposed on patients. This project was not a research study, it entailed operational improvements to the service that would ensure a consistent approach towards all patients and collected some extra information as part of business as usual. There was no additional risk posed to patients.
References
- 1.Department of Health. How to make IAPT more accessible to older people: A compendium. Department of Health; London: 2013. [Google Scholar]
- 2.Department of Health Guide. IAPT Older People Positive Practice Guide. Department of Health; London: 2009 [Google Scholar]
- 3.Forum for mental health in primary care. Management of Depression in Older People: Why this is important in primary care. The forum for mental health In Primary Care; London: June, 2014. [Google Scholar]
- 4.Department of Health. Talking Therapies: Four Year Plan of Action. Department of Health; London: 2011. [Google Scholar]
- 5.Mohlman J, Gorman JM. The role of executive functioning in CBT: A pilot study with anxious older adults. Behaviour Research and Therapy. 2005. 43, 447–465. [DOI] [PubMed] [Google Scholar]
Bibliography:
- Laidlaw K, Thompson LW, Dick-Siskin L, Gallagher-Thompson D. Cognitive Behaviour Therapy with Older People. 2003. Chichester: Wiley. [Google Scholar]
- Nancy A. Pachana, Laidlaw K. Oxford Handbook of Clinical Geropsychology. 2014. (available online) [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjqir.u206099.w2510supp.pdf (219.8KB, pdf)