Abstract
Malaria is one of the most important parasitic diseases worldwide, which is characterized by high morbidity and mortality in tropical and subtropical regions. The aim of this study was to evaluate epidemiology of malaria in East Azerbaijan province, Iran, from 2001 to 2013. During 13 years, blood samples were taken from all suspected malaria cases using lancet and then peripheral blood smear was prepared using one blood drop. The smears were stained by Giemsa’s stain and were examined under a light microscope with 1000X of magnification. All demographic variables and epidemiological recorded data were obtained from Health Center and were analyzed by SPSS v. 16 software using descriptive statistical tests. Total of 133 cases were fined to be infected by malaria in 13 years that the highest rate (54.13 %) was observed in Kaleybar county. One hundred and fifteen (86.46 %) and 18 (13.54 %) out of 133 infected individuals were male and female, respectively. Mean age of the infected people was 31.57 years. The most affected age group was 30–40 years. One hundred twenty seven (95.48 %) and 6 (4.52 %) cases were infected by Plasmodium vivax and Plasmodium falciparum, respectively. Based on the findings of this study, the incidence of malaria has been declined continuously over the past decade in East Azerbaijan province, Iran.
Keywords: Malaria, Epidemiology, Plasmodium falciparum, Plasmodium vivax, Iran
Introduction
Malaria is one of the most important parasitic diseases all over the globe (Assmar et al. 2003). The disease is a public health problem caused by Plasmodium spp. and is transmitted by Anopheles mosquitoes that are commonly seen in tropical and subtropical areas. People can be infected by mosquito bites, tissue transplantation, blood transfusion and transplacental transmission (Aydin and Sahin 2013; Cox 2010).
P. falciparum and P. vivax cause most of the malaria infections globally. Approximately half of the world’s population live in regions, including 100 countries from Africa, Asia, the Middle East, Eastern Europe, Central and South America, Caribbean and Oceania, where malaria is transmitted (Cullen and Arguin 2002). According to available information, it is estimated 219 million clinical cases and 660,000 deaths globally in 2010, mostly among children aged <5 years living in sub-Saharan Africa (Cullen and Arguin). Based on the World Malaria Report (2011), it is estimated that 3.3 billion people were at risk of malaria in 2010. Of this number, 2.1 billion were at low risk while 1.2 billion people were at high risk (>1 case per 1,000 population) that were living mostly in the African (47 %) and Southeast Asian regions (37 %) (Goh et al. 2013; Newman 2011).
In the past, malaria was widespread disease in Iran. In 1924, it was estimated that 4–5 million out of 13 million individuals had contracted the disease (Khalili et al. 2009; Sadrizadeh 2001). As a result of the anti-malaria campaign started in 1951, malaria transmission was interrupted in many regions. Reports show that there has been a decreasing trend in the malaria incidence in recent years in Iran (Manouchehri et al. 1992). The prevalence rate of malaria was reported about 1 in 10,000 individuals at first midyear of 2002 and majority of the cases were reported in summer (Edrissian 2003).
Malaria is endemic in southeast of Iran with a prevalence of 25.5 per 1,000 individuals with the same proportions of P. vivax and P. falciparum (Assmar et al. 2003). The prevalence of malaria in south and southeast of Iran is hypoendemic. There has been a decrease in the incidence rate of malaria in recent years due to local drought (from 23,860 cases in 1999 to 19,700 in 2000).
Now, southeast of Iran including Sistan and Bluchistan, Hormozgan and South of Kerman provinces are still considered as endemic areas for malaria (Assmar et al. 2003). About 60 % of population of Iran was living in endemic areas with 30–40 % malaria morbidity before beginning of any malaria control program (Edrissian 2006; Hanafi-Bojd et al. 2010).
Reported studies in 2008 indicate that out of 11,460 malaria cases in Iran, 8 % was due to P. falciparum, whereas 90 % were infected by P. vivax (Ministry of Health 2008). In WHO malaria report 2009, Iran indicated evidence of a continuous decrease in the number of cases associated with wide measure implementation of malaria control activities. The country is classified as in the pre-elimination step (Aregawi et al. 2009).
By 1977, malaria transmission was interrupted in all northern parts of Iran (Zakeri et al. 2004), But in 1991, after the independence of the southern countries of the former Soviet Union and the outbreak of the Nagorno-Karabakh civil war, a new threat of malaria importation emerged lately from the Republic of Azerbaijan to the north-west of Iran, which was affected by serious epidemics of P. vivax (Vatandoost et al. 2003).
Various factors can affect malaria reappearance in this region such as; socio-economic conditions, especially movement of massive populations from war-stricken zones in the Republic of Azerbaijan. Cases have been reported in emigrant camps since 1993, while probably more cases have gone unreported outside the camps. Hence, in some parts of West Azerbaijan, East Azerbaijan, Ardabil and Guilan provinces of Iran, several malaria foci were seen (Vatandoost et al. 2003).
Better control and monitoring programs cannot be fulfilled without adequate information on the epidemiology of malaria in different parts of the country. Thus it is necessary to have updated information about the epidemiology of the disease in each region. The aim of this study was to evaluate and report malaria cases in East Azerbaijan province, Iran, from 2001 to 2013 in order to determine the incidence and prevalence of malaria in the studied region.
Materials and methods
The present cross-sectional retrospective study was carried out in order to determine epidemiological feature of malaria in East Azerbaijan province, Iran. Thus, all episodes from 2001 to 2013 documented in Health Center of province was carefully studied, analyzed and reported.
Based on the recorded documents, blood sampling has been done using sterile lancet from the patient’s middle finger. Then one drop of blood was placed on a clean microscopic slide and spread with another slide to prepare a peripheral blood smear. The methanol fixed slides were stained by Giemsa’s stain and dried in air. The whole blood smears were precisely examined under light microscope using 100X objective for any possible Plasmodium spp. by an expert technician.
Positive specimens and patient’s related information were recorded and sent to Health Center located in Tabriz city, capital of East Azerbaijan province (Google Maps location of East Azerbaijan province link: https://www.google.com/maps/@37.9505774,46.7470071,8z?hl=en). Epidemiological data including type of malaria (endemic or imported), transmission season and demographic variables such as sex, county of infection, age group and parasite species were investigated.
One hundred and fifteen (86.46 %) and 18 (13.54 %) out of 133 infected individuals were male and female, respectively. The mean age of patients was 31.57 years and the most affected age group was 31–40 years. The oldest and the youngest cases were 17 and 51 years old, respectively.
Data were analyzed by SPSS (version 16.2, SPSS Inc., Chicago, IL, USA) through descriptive tests.
Results
Total of 133 malaria cases were documented during 13 years (2001–2013) in East Azerbaijan province that the highest infection rate was related to Kaleybar county (54.13 %). The distribution of malaria cases in each region of the province during 13 years is available in Table 1. One hundred and fifteen (86.46 %) and 18 (13.54 %) out of 133 infected individuals were male and female, respectively. The mean age of patients was 31.57 years and the most affected age group was 31–40 years. The oldest and the youngest cases were 17 and 51 years old, respectively. The distribution of malaria cases by age group are presented in Table 2.
Table 1.
Distribution of malaria cases in East Azerbaijan province during studied years
| County | Year | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | Total | |
| Azarshahr | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Osku | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Ahar | 2 | – | – | – | 1 | – | – | – | – | – | – | – | – | 3 |
| Bostanabad | – | – | – | 1 | – | – | – | – | – | – | – | – | – | 1 |
| Bonab | – | – | – | – | 1 | – | – | – | – | – | – | – | – | 1 |
| Tabriz | – | 1 | 5 | – | 3 | – | – | 1 | 2 | – | 1 | – | – | 13 |
| Jolfa | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Charoymaq | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Sarab | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Shabestar | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Ajabshir | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Kaleybar | 19 | 12 | 29 | 12 | – | – | – | – | – | – | – | – | – | 72 |
| Maragheh | – | – | – | – | – | 1 | – | – | – | – | – | – | – | 1 |
| Marand | 2 | 1 | – | – | 1 | – | – | – | – | – | – | – | – | 4 |
| Malekan | 1 | 2 | 1 | 2 | – | 1 | – | – | – | – | 1 | – | – | 8 |
| Miyaneh | 15 | 9 | – | 1 | – | 1 | – | – | 2 | – | – | – | – | 28 |
| Varzaqan | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Heris | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Hashtrud | 1 | – | – | – | – | – | 1 | – | – | – | – | – | – | 2 |
| Total | 40 | 25 | 35 | 16 | 6 | 3 | 1 | 1 | 4 | 0 | 2 | 0 | 0 | 133 |
Table 2.
Distribution of malaria cases based on the age groups
| Age group | Frequency n (%) |
|---|---|
| <20 | 8 (6.1) |
| 20–30 | 46 (34.59) |
| 31–40 | 68 (51.13) |
| >40 | 11 (8.27) |
One hundred twenty seven cases (95.48 %) and 6 (4.52 %) cases were infected by P. vivax and P. falciparum, respectively. No other Plasmodium spp. has been recorded. Highest reported rate of infection observed in 2001 that 40 patients were infected by malaria parasite which all the cases were related to P. vivax. After that, the highest infection rate was observed in 2003 that 35 (26 %) cases out of 133 malaria cases were documented (Table 3).
Table 3.
Distribution of malaria cases in different genders and years
| Year | Sex | Total n (%) | |
|---|---|---|---|
| Male | Female | ||
| 2001 | 36 | 4 | 40 (30.07) |
| 2002 | 20 | 5 | 25 (18.79) |
| 2003 | 29 | 6 | 35 (26.31) |
| 2004 | 13 | 3 | 16 (12.03) |
| 2005 | 6 | 0 | 6 (4.51) |
| 2006 | 3 | 0 | 3 (2.25) |
| 2007 | 1 | 0 | 1 (0.75) |
| 2008 | 1 | 0 | 1 (0.75) |
| 2009 | 4 | 0 | 4 (3) |
| 2010 | 0 | 0 | – |
| 2011 | 2 | 0 | 0 (1.5) |
| 2012 | 0 | 0 | – |
| 2013 | 0 | 0 | – |
| Total n (%) | 115 (86.46) | 18 (13.54) | 133 |
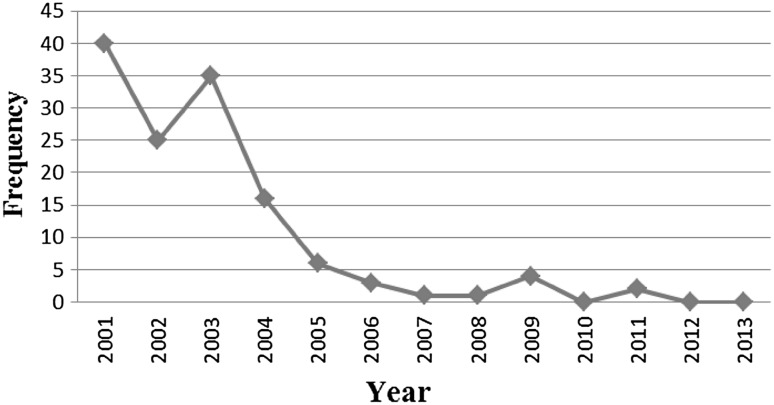
All the cases from 2001 to 2004 were endemic and were related to P. vivax, but from 2005 to 2013 all malaria cases were imported, which were related to P. falciparum and P. vivax. All these imported cases had traveled to Sistan and Baluchistan, Kerman provinces and Chabahar city (south and south east of Iran). The endemic transmission was occurred during June to the end of October of each year (Fig. 1).
Fig. 1.
Annual distribution of malaria cases in East Azerbaijan province
Discussion
In the past, malaria was widespread in Iran (Khalili et al. 2009; Manouchehri et al. 1992), but it has decreasing trend gradually. In East Azerbaijan province malaria infection was observed in 133 cases during 13 years (2001–2013). The highest infection rate was reported in 2001 that 40 patients (30 %) were infected, which all cases were P. vivax.
The results of this study illustrate the endemic pattern of transmission of malaria from 2001 to 2004 in the studied area. Since 2005, all reported malaria cases were imported due to traveling to southern endemic regions such as Chabahar city, Sistan and Bluchistan and Kerman provinces. It is clear that the endemic transmission of malaria has interrupted from 2005 in the studied region.
Based on the results of the present study, the decreasing trend of malaria in East Azerbaijan province is similar to the report of Khalili et al. (2009) in Yazd province (Khalili et al. 2009) that can be attributed to malaria control, prevention and fighting program. The transmission period of all endemic malaria cases in East Azerbaijan province was related to hot season (from June to end of October).
Khalili et al. (2009) reported 79.7 % of malaria cases in spring. The higher prevalence in spring might be due to the construction projects and migration from Afghanistan to Pakistan, but it could be due to activity of mosquitoes carrying the parasite in hot season in Yazd provinces (Khalili et al. 2009).
In the present study, proportion of P. vivax and P. falciparum infection were 95.48 and 4.52 %, respectively. P. vivax was the predominant species in the studied region. Also, all reported endemic malaria cases were P. vivax in the studied area. However, imported cases were both P. vivax and P. falciparum.
In a study in Africa, proportion of P. vivax and P. falciparum has been reported 79 % and 21 %, respectively (Mahon and Manuselis 1995; Reza and Taghi 2011). In a study conducted in Bandar Abbas city (Hanafi-Bojd et al. 2010), proportion of P. vivax and P. falciparum were reported 97.69 and 2.17 %, in Yazd province (Khalili et al. 2009) 85.2 and 13.7 %, in Sistan and Bluchistan province (Reza and Taghi 2011) 90 and 7.8 %, respectively. In the present study, similar to the mentioned studies above, P. vivax observed as a predominant species.
The mean age of patients in this study was 31.57 years, but in Yazd province (Khalili et al. 2009), south and southeast of Iran (Assmar et al. 2003) the mean age of patients has been reported 22.5, which are slightly lower than the mean age that we have fined. In the present study the most affected age group observed in 31–40 (51.13 %) years. In Turkey, the most infected age were reported in 15–44 age group (Aydin and Sahin 2013). This difference is probably related to the different geographical regions which the studies carried out.
We noted the lowest infection rate in patients with less than 20 years of age (6.1 %), but in the survey conducted in south and southeast of Iran (Assmar et al. 2003), this age group indicated high rate of infection. This difference could be due to being in endemic and non-endemic areas of malaria. Also, in our study, 86.46 % of infected people were males and 13.54 % were females. In Yazd province, 95 % of patients were males and 5 % females (Khalili et al. 2009). Both studies illustrate higher rate of infection in men. Also similar results about the gender of the patients have been reported in Iran and Turkey (Assmar et al. 2003; Aydin and Sahin 2013; Hanafi-Bojd et al. 2010; Reza and Taghi 2011) the high prevalence of malaria in men might be due to more exposure to the vector.
Based on the findings of the present study, it is clear that the endemic transmission of malaria has interrupted from 2005 in the studied region. This may be happened due to anti-malaria campaign started and/or drought that Iran faced during recent years (Assmar et al. 2003; Manouchehri et al. 1992). Also during the past decades hygienic and sanitary levels of Iran have been got better and other parasitic diseases such as intestinal infections also been decreased continuously (Jafari et al. 2014a; Jafari et al. 2014b). Malaria may have the same pattern of decline and relationship with the hygienic status of the people who live in Iran.
Conclusion
According to the results of the present study, in the past few years, there has been no endemic transmission of malaria in East Azerbaijan province, Iran. Also we faced a dramatic decline in the incidence of malaria during the past decade, which shows the effectiveness of malaria control and elimination program. Additionally, increasing awareness of people about transmission of malaria in endemic areas, control and monitoring of the infection before and after traveling may help to prevent occurrence of imported malaria in East Azerbaijan province.
Acknowledgments
The authors would like to thank Health Center staff of East Azerbaijan province and who had helped us in this study.
References
- Aregawi M, Cibulskis RE, Otten M, Williams R. World malaria report 2009. Geneva: World Health Organization; 2009. [Google Scholar]
- Assmar M, Terhovanessian A, Jahani MR, Nahrevanian H, Amirkhani A, Piazak N, Esmaeili AR, Farahmand M, Zare M (2003) Molecular epidemiology of malaria in endemic areas of Iran. Southeast Asian J Trop Med Public Health 34:15–19 [PubMed]
- Aydin MF, Sahin A. Malaria epidemiology in Mersin province, Turkey from 2002 to 2011. Iran J Parasitol. 2013;8:296. [PMC free article] [PubMed] [Google Scholar]
- Cox FE. History of the discovery of the malaria parasites and their vectors. Parasit Vectors. 2010;3:5. doi: 10.1186/1756-3305-3-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cullen KA, Arguin PM. Malaria Surveillance at United States, 2011. Morb Mortal Wkly Rep Surveill Summ. 2002;62:1–17. [PubMed] [Google Scholar]
- Edrissian GH. Malaria history and status in Iran. J School Public Health Inst Public Health Res. 2003;1:50–61. [Google Scholar]
- Edrissian G. Malaria in Iran: past and present situation. Iran J Parasitol. 2006;1:1–14. [Google Scholar]
- Goh Xiang, Lim Yvonne AL, Vythilingam Indra, Chew Ching, Lee Ping, Ngui Romano, Tan Tian, Yap Nan, Nissapatorn Veeranoot, Chua Kek. Increased detection of Plasmodium knowlesi in Sandakan division, Sabah as revealed by PlasmoNex™. Malaria Journal. 2013;12(1):264. doi: 10.1186/1475-2875-12-264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanafi-Bojd AA, Vatandoost H, Philip E, Stepanova E, Abdi A, Safari R. Malaria situation analysis and stratification in Bandar Abbas County, southern Iran, 2004–2008. Iran J Arthropod Borne Dis. 2010;4:31–41. [PMC free article] [PubMed] [Google Scholar]
- Jafari R, Fallah M, Yousofi Darani H, Yousefi HA, Mohaghegh MA, Latifi M, Sadaghian M, Maghsood AH. Prevalence of intestinal parasitic infections among rural inhabitants of Hamadan city, Iran, 2012 Avicenna. J Clin Microb Infec. 2014;1:e21445. [Google Scholar]
- Jafari Rasool, Sharifi Forough, Bagherpour Bahram, Safari Marzieh. Prevalence of intestinal parasites in Isfahan city, central Iran, 2014. Journal of Parasitic Diseases. 2014;40(3):679–682. doi: 10.1007/s12639-014-0557-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khalili MB, Anvari-Tafti MH, Sadeh M. Epidemiological pattern of malarial disease in the province of Yazd, Iran (Since 1986–2006) World. J Med Sci. 2009;4:41–45. [Google Scholar]
- Mahon C, Manuselis G. Textbook of diagnostic microbiology. Philadelphia: WB Saunders Company; 1995. [Google Scholar]
- Manouchehri AV, Zaim M, Emadi AM. A review of malaria in Iran 1975–90. J Am Mosq Control Assoc. 1992;8:381–385. [PubMed] [Google Scholar]
- Newman RD (2011) World malaria report
- Reza YM, Taghi RM. Prevalence of malaria infection in Sarbaz, Sistan and Bluchistan province. Asian Pac J Trop Biomed. 2011;1:491–492. doi: 10.1016/S2221-1691(11)60107-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadrizadeh B. Malaria in the world, in the eastern Mediterranean region and in Iran: review article WHO/EMRO. Report. 2001;1:13. [Google Scholar]
- Vatandoost H, Ashraf H, Lak SH, Mahdi RE, Abai MR, Nazari M. Factors involved in the re-emergence of malaria in borderline of Iran Armenia, Azerbaijan and Turkey. Southeast Asian J Trop Med Public Health. 2003;34:6–14. [PubMed] [Google Scholar]
- Zakeri S, Mamaghani S, Mehrizi AA, Shahsavari Z, Raeisi A, Arshi S, Dinparast-Djadid N. Molecular evidence of mixed P. vivax and P. falciparum infections in northern Islamic Republic of Iran. East Mediterr Health J. 2004;10:336–342. [PubMed] [Google Scholar]