Abstract
We report five serial cases of ciliated muconodular papillary tumor (CMPT) of the lung. CMPT is characterized as a low-grade malignant tumor with ciliated columnar epithelial cells combined with goblet cells, typically presenting as peripheral lung tumor and often causing diagnostic or therapeutic problems. In the cases described here, all patients presented with abnormal chest shadow but no definitive symptoms. Although all tumors were peripheral, computed tomography (CT) revealed various radiographic findings including small lung nodules, ground-grass opacity or irregular-shaped consolidation. All patients underwent complete surgical resection, and no recurrence has been noted over follow-up. In all cases, pathological findings included columnar ciliated cells with mucus lakes, consistent with the immunohistochemical staining. As there are few reports on this tumor entity, which has not yet received a WHO classification, we believe our case series may be of interest.
Introduction
Lung tumors with ciliated cells are usually benign, mostly occurring in the central airway. Ciliated muconodular papillary tumor (CMPT) is a relatively new clinical entity characterized by ciliated columnar cells and goblet cells, which often appear in the peripheral lung [1]. The radiological findings and clinical behavior are not yet well described. Here, we report five surgical cases of CMPT.
Case Report
Patient 1
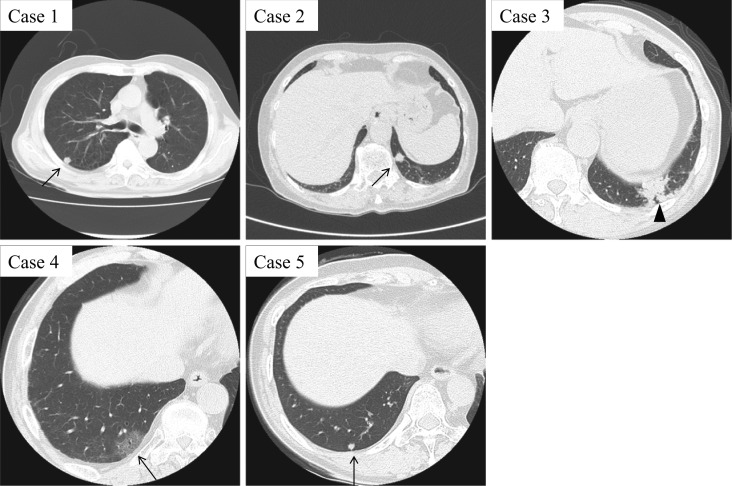
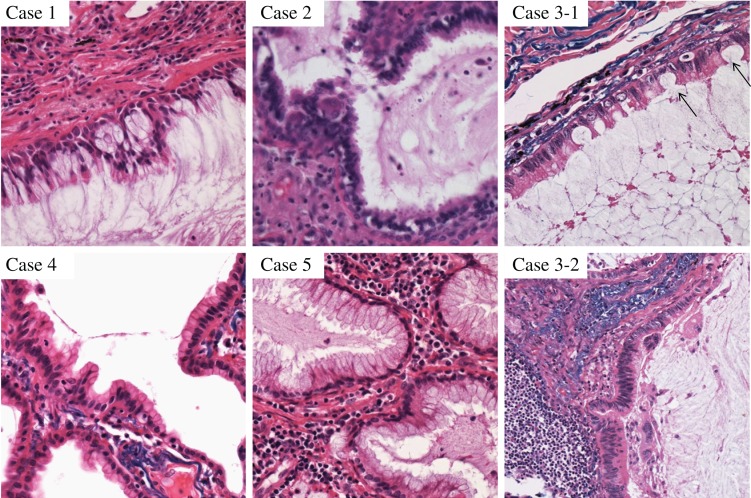
A 66-year-old man with a 45 pack/year smoking history was referred to our hospital with abnormal chest shadow. Chest computed tomography (CT) findings revealed a 10-mm peripheral right lung nodule (Fig. 1). Because frozen sections of the tumor presented borderline lesions with mucinous cystic neoplasm, right upper lobectomy was carried out. Histological findings showed low-grade malignant tumor with ciliated columnar cells and goblet cells (Fig. 2), resulting in a final diagnosis of CMPT. No recurrence has been noted during a 58-month follow-up.
Figure 1:
CT findings of five CMPT cases. While Cases 1, 2 and 5 present with small peripheral pulmonary nodules around 10 mm in diameter, Case 4 shows a ground-grass opacity pattern (arrow). Case 3 with mucinous colloid adenocarcinoma exhibits an irregular consolidation-like lesion, which is highly suggestive of lung cancer (arrowhead).
Figure 2:
Histopathological findings of five CMPT cases, showing ciliated columnar cells with mucous lakes. Case 3 presented with mucinous colloid adenocarcinoma (bottom), as well as CMPT with typical features of goblet cells (top/arrow).
Patient 2
An 82-year-old woman with no smoking history was admitted to our hospital due to abnormal chest shadow. Chest CT findings revealed a 10-mm peripheral nodule in the left S10 segment (Fig. 1). Because lung cancer was strongly suspected, mediastinoscopy followed by thoracoscopic partial resection of the tumor was performed. Frozen sections of the nodule revealed no evidence of malignancy, and CMPT was suspected, confirmed by histological diagnosis (Fig. 2). The patient remained free of recurrence after 55 months.
Patient 3
A 77-year-old man with a 57-pack-year smoking history had an abnormal shadow on routine medical check-up in the left lower lobe (Fig. 1). Lung cancer was strongly suspected, and thoracoscopic left lower lobectomy was performed. Adenocarcinoma was suspected at intraoperative histological consultation, with low-grade malignant tumor including CMPT a possibility. Postsurgical histological findings revealed a transitional or mixed tumor of mucinous colloid adenocarcinoma and CMPT 45 mm in size (Fig. 2). The patient was given oral tegafur-uracil as adjuvant chemotherapy, suspended because of drug toxicity after 6 months. Neither local recurrence nor distant metastasis has been noted at 48 months.
Patient 4
A 70-year-old man with a 92-pack-year smoking history as well as a history of asbestos exposure visited our hospital with a 30-mm peripheral ground-grass opacity (GGO) in the right lower lobe (Fig. 1). Thoracoscopic partial resection of the tumor was performed, and intraoperative frozen section investigation revealed CMPT, which was confirmed by postoperative histological analysis. The tumor showed proliferation of the mucinous epithelium at 15 mm in the subpleural area (Fig. 2). The patient remained relapse-free at 19 months.
Patient 5
A 67-year-old woman was referred with a growing peripheral small lung nodule. She had never smoked but had a medical history of bronchial asthma and eosinophilic pneumonia treated with oral corticosteroid. Chest CT revealed remaining lung nodules with pleural indentation in the S10 segment of the right lung (Fig. 1). Thoracoscopic partial resection was conducted, and pathological diagnosis was CMPT 5 mm in diameter (Fig. 2). The patient remained free of recurrence 28 months postoperatively.
Discussion
While pulmonary tumors with cilia are basically benign, CMPT possess some histological features associated with low-grade malignancy [1]. Irrespective of histological characteristics, the malignant potential of this neoplasm is still unclear.
To date, several cases with lung nodules have been pathologically confirmed as CMPT and reported in the literature [1–6]. Radiological findings mainly include irregular-shaped nodules, sometimes with adjoining GGO [2], ranging in size from 5 to 15 mm. Malignancy could not be ruled out on the basis of radiological findings alone. Characteristics of our five cases are summarized in Table 1.
Table 1.
Characteristics of five CMPT cases
| Case number | Age/sex | Smoking history | Maximum tumor size (mm) | Location | CT findings | Intraoperative pathological diagnosis | Operation mode |
|---|---|---|---|---|---|---|---|
| 1 | 66 M | Ex | 13 | RUL | Well-defined nodule | Mucinous cystic neoplasm, borderline lesion | Lobectomy |
| 2 | 82 F | Never | 10 | LLL | Well-defined nodule | No malignancy | Partial resection |
| 3 | 77 M | Current | 45 | LLL | Irregular-shaped mass | Mucinous colloid adenocarcinoma suspected | Lobectomy |
| 4 | 70 M | Ex | 35 | RLL | Ground-grass shadow | CMPT | Partial resection |
| 5 | 67 F | Never | 5 | RLL | Well-defined nodule | No malignancy | Partial resection |
RUL, right upper lobe; LLL, left lower lobe; RLL, right lower lobe.
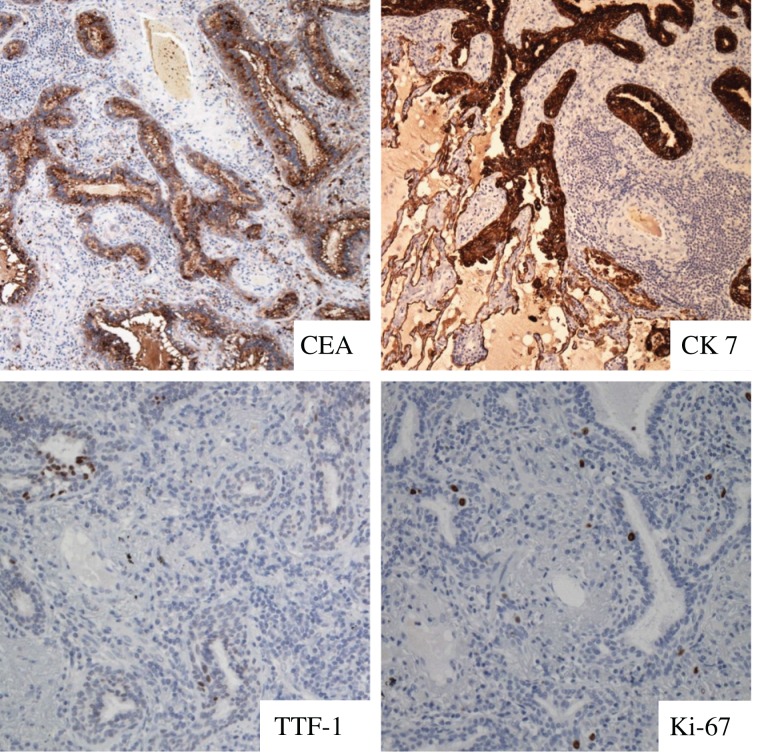
Histologically, CMPT shows few atypia and a low Ki-67 index, consistent with its more benign nature. Characteristic markers of CMPT are reported to be carcinoembryonic antigen, thyroid transcription factor-1 and cytokeratin (CK) 7, whereas CK20 is negative [2]. This is very similar to our cases (Fig. 3), with the exception of Patient 3 with malignant tumor. Immunohistochemical characteristics of our cases are presented in Table 2.
Figure 3:
Immunohistochemical findings of Case 2, showing positive staining pattern for CEA, CK7 and TTF-1 with low Ki-67 index. CEA, carcinoembryonic antigen; CK, cytokeratin; TTF-1, thyroid transcription factor-1.
Table 2.
Immunohistochemical staining patterns of five CMPT cases
| Case number | CEA | TTF-1 | CK7 | CK20 | Ki-67 | p53 |
|---|---|---|---|---|---|---|
| 1 | Positive | Negative | Positive | Negative | <5% | n/a |
| 2 | Positive | Positive | Positive | Negative | <3% | n/a |
| 3 | Positive | ± | Positive | Positive | 1–5% | Positive |
| 4 | Positive | Negative | Positive | Negative | 1–10% | Positive |
| 5 | Positive | Positive | Positive | Negative | Small | Positive |
n/a, not applicable; CEA, carcinoembryonic antigen; TTF-1, thyroid transcription factor-1; CK, cytokeratin.
CMPT is reported to affect mostly elderly patients [7]. This tumor could occur in either sex, without any correlation with smoking history. All patients were asymptomatic, with incidentally discovered abnormal pulmonary shadow, and diagnosed as CMPT after surgical intervention. With its rarity and peripheral nature, preoperative diagnosis with transbrochial or percutaneous biopsy will be difficult.
Although the optimal surgical approach for CMPT has not been established, wedge resection of the lung with wide free-margins might be sufficient. However, because coexistent malignant tumors can also be present, careful investigation of appropriate histological material is indispensable. When differentiation from malignant tumor is difficult, the standard surgical modality for lung cancer should be the treatment of choice.
The metastatic or invasive nature of this tumor has not been determined. It seems that all CMPT cases, including ours described here, remained free from recurrence after complete surgical resection [7]. Further observation is required to clarify metastatic potential.
In conclusion, CMPT is a rare pulmonary tumor with cilia and goblet cells often incidentally found as small irregular peripheral nodules on chest CT of elderly patients. Although basically regarded as benign, some histological characteristics suggest low-grade malignancy, with potential for malignant transformation or possibility of recurrence. Further accumulation of similar cases will be vital to determine the true clinical characteristics of this tumor entity.
Conflict of interest statement
None declared.
References
- 1.Ishikawa Y. Ciliated muconodular papillary tumor of the peripheral lung: benign or malignant. Pathol Clin Med (Byouri-to-Rinsho) 2002;20:964–5 (in Japanese). [Google Scholar]
- 2.Sato S, Koike T, Homma K, Yokoyama A. Ciliated muconodular papillary tumor of the lung: a newly defined low-grade malignant tumour. Interact Cardiovasc Thorac Surg 2010;11:685–7. [DOI] [PubMed] [Google Scholar]
- 3.Hata Y, Yuasa R, Sato F, Otsuka H, Goto H, Isobe K, et al. Ciliated muconodular papillary tumor of the lung: a newly defined low-grade malignant tumor with CT findings reminiscent of adenocarcinoma. Jpn J Clin Oncol 2013;43:205–7. [DOI] [PubMed] [Google Scholar]
- 4.Chuang HW, Liao JB, Chang HC, Wang JS, Lin SL, Hsieh PP. Ciliated muconodular papillary tumor of the lung: a newly defined peripheral pulmonary tumor with conspicuous mucin pool mimicking colloid adenocarcinoma: a case report and review of literature. Pathol Int 2014;64:352–7. [DOI] [PubMed] [Google Scholar]
- 5.Lau KW, Aubry MC, Tan GS, Lim CH and Takano AM. Ciliated muconodular papillary tumor: a solitary peripheral lung nodule in a teenage girl. Hum Pathol 2016;49:22–6. [DOI] [PubMed] [Google Scholar]
- 6.Harada T, Akiyama Y, Ogasawara H, Kishi F, Hattori A, Okamoto K, et al. Ciliated muconodular papillary tumor of the peripheral lung: a newly defined rare tumor. Respir Med CME 2008;1:176–8. [Google Scholar]
- 7.Kamata T, Yoshida A, Kosuge T, Watanabe S, Asamura H, Tsuta K. Ciliated muconodular papillary tumors of the lung: a clinicopathologic analysis of 10 cases. Am J Surg Pathol 2015;39:753–60. [DOI] [PubMed] [Google Scholar]