Abstract
The aim of this study was to investigate the efficiency of domestic physician-staffed helicopter emergency medical service (HEMS) for the transport of patients with severe trauma to a hospital. The study included patients with blunt trauma who were transported to our hospital by physician-staffed HEMS (Group P; n = 100) or nonphysician-staffed HEMS (Group NP; n = 80). Basic patient characteristics, transport time, treatment procedures, and medical treatment outcomes assessed using the Trauma and Injury Severity Score (TRISS) were compared between groups. We also assessed patients who were transported to the hospital within 3 h of injury in Groups P (Group P3; n = 50) and NP (Group NP3; n = 74). The severity of injury was higher, transport time was longer, and time from hospital arrival to operation room transfer was shorter for Group P than for Group NP (P < 0.001). Although Group P patients exhibited better medical treatment outcomes compared with Group NP, the difference was not statistically significant (P = 0.134 vs. 0.730). However, the difference in outcomes was statistically significant between Groups P3 and NP3 (P = 0.035 vs. 0.546). Under the current domestic trauma patient transport system in South Korea, physician-staffed HEMS are expected to increase the survival of patients with severe trauma. In particular, better treatment outcomes are expected if dedicated trauma resuscitation teams actively intervene in the medical treatment process from the transport stage and if patients are transported to a hospital to receive definitive care within 3 hours of injury.
Keywords: Injuries, Emergencies, Aircraft, Resuscitation, Treatment Outcome, Prehospital Emergency Care, Trauma Centers
Graphical Abstract
INTRODUCTION
Trauma is the leading cause of death of individuals aged < 45 years and the third leading cause of death in the entire population in South Korea, accounting for the maximum economic and life losses (1). Studies in advanced countries have reported that deaths from trauma can be prevented and decreased to one-fourth of the total number of deaths, with a further decrease to < 10% with the establishment of appropriate emergency medical systems (2,3,4,5). The Korean government has also established a goal to decrease the rate of preventable trauma-related deaths to 20% by 2020 and has been making consistent efforts to achieve this goal and establish an effective trauma management system tailored to domestic conditions through various measures since 2012, such as the establishment of 17 regional trauma centers throughout the country.
Timely transport of patients with severe trauma to an appropriate hospital where definitive care can be provided is the most important component of prehospital emergency medical care with regard to patient survival. Several studies have reported that helicopter-aided transportation decreases the mortality rate for trauma. Helicopter-aided transportation of emergency patients is actively implemented in advanced countries where emergency medical delivery systems are well established (6). Thomas et al. (7) performed a multicenter study and reported a decrease in the mortality rate to 24% when patients with trauma were transported by a helicopter. Taylor et al. (8,9) reported that physician-staffed helicopter emergency medical services (HEMS), despite their high initial cost, is beneficial with regard to cost effectiveness, considering the improvement in the mortality rate when calculated in monetary terms. However, not many studies have evaluated HEMS in South Korea. Although a few cases of helicopter-aided transportation after mountain accidents have been reported (10), HEMS, particularly physician-staffed HEMS, remain poorly studied. From these perspectives, we conducted the present study to investigate the necessity of physician-staffed HEMS for severe trauma patients by comparing the treatment outcomes of patients transported by physician-staffed and nonphysician-staffed HEMS.
MATERIALS AND METHODS
Patient data and transport settings
This study was conducted from April 2011 to June 2015 and included patients with blunt trauma who were transported by helicopter to our hospital for medical care. The authors work for the tertiary university hospital, which is running a trauma center equivalent to a level I trauma center in the United States. The hospital has been actively providing HEMS-aided patient transport since 2011 in collaboration with Fire and Disaster Headquarters / Aviation Team (local and national 119) and military and law enforcement professionals. The trauma center receives 2,300+ inpatients each year, with approximately 23% exhibiting severe trauma with an Injury Severity Score (ISS) of 15+.
This study targeted only those patients who were transported by a helicopter belonging to the Fire and Disaster Headquarters / Aviation Team and excluded the relatively fewer patients transported by helicopters belonging to military or police services, which are operated only under special circumstances. Furthermore, only patients with blunt trauma aged > 15 years were included. Patients with penetrating wounds; choked, burned, or drowned patients; patients who were declared dead on arrival (DOA), and patients who died in the emergency department despite resuscitation efforts (DIED) were excluded. Data were collected from medical records, videos filmed during the helicopter's landing and take-off, and films recorded with goggle cameras (Liquid Image Co® model 384, Santa Rosa, CA, USA) worn by the medical team at the time of boarding the helicopter. When the medical team was dispatched to the accident scene, they carried first-aid equipment and medicines. A trauma team comprising five trauma surgeons, one emergency physician and a nurse practitioner or emergency technician from the trauma center was generally on board.
If paramedics from the Firefighter Department or doctors from other facilities request the trauma team to the Fire and Disaster Headquarters for dispatching to the accident scene, the physician-staffed HEMS was activated based on the decision of the trauma team leader on duty. The trauma team leader activated the physician-staffed HEMS for cases that required fast transportation to a higher level facility according to the Field Triage Decision Schemes (11). As HEMS was activated, the helicopter from the Fire and Disaster Headquarters / Aviation Team transported the physician-staffed HEMS team at our hospital to the accident scene or other facilities. However, the pilots and paramedics from the Firefighter Department dispatched directly to the scene for minor injuries (i.e., ankle sprain from hiking) without a dispatch request at locations where the ground ambulance could not approach (i.e., mountains, sea, or islands). When this happened, one or two emergency medical technicians in the helicopter provided some basic life support procedures that were possible under the current domestic regulations with phone instructions from the medical team at the hospital.
We divided the patients into two groups. Group P patients were transported by physician-staffed HEMS and Group NP patients were transported by nonphysician-staffed HEMS. Basic patient characteristics, transport time, treatment procedures, and medical treatment outcomes, among other factors, were analyzed and compared between groups. Treatment on the helicopter was administered in accordance with the Advanced Trauma Life Support (ATLS)® guidelines (11).
Trauma and Injury Severity Score (TRISS)
TRISS is a tool used for predicting the prognosis of patients with trauma (12,13), and it is universally accepted for determination of the impact of HEMS on trauma-related mortality (14,15,16,17,18,19). The TRISS is a combined scoring system that was developed in 1987 (20), and it is based on the ISS as an anatomic component, RTS (21) as a physiological component, and patient age as a comorbid component, resulting in a combined index for injury that complements each component. The Major Trauma Outcome Study (MTOS) is a study wherein TRISS, age, and the mechanism of injury were used to calculate survival norms using regression analysis for 80,000 patients with trauma from 139 North American hospitals (22). The MTOS cohort has been widely used as a benchmark for comparing outcomes of trauma patients using the TRISS methodology. These data can be used to identify unexpected outcomes in both populations and individual patients.
Initial vital signs and Glasgow Coma Scale (GCS) scores were recorded for all patients on arrival at the trauma center and used to calculate RTS. Furthermore, Abbreviated Injury Scale (AIS) coding was performed by two trauma coordinators, and the results were reviewed by the dedicated trauma faculties (5 trauma surgeons, 1 emergency physician, 1 neurosurgeon, 1 orthopedic surgeon, and 1 radiologist) to yield ISS. These values were then inserted into the TRISS equation (12) to calculate the probability of survival. The obtained data were compared using statistical methods. MTOS-derived coefficients revised in 1995 (13) were used.
Statistical analysis
We used SPSS version 19 (IBM corporation) for all statistical analyses. Continuous data are summarized as medians and interquartile ranges (IQRs) unless otherwise specified. We compared patient demographics, TRISS, and transport time using the Mann–Whitney U test or χ2 analysis, as appropriate. Comparisons between predicted and observed patient mortality were made using Z and W statistics (12). The Flora Z statistic estimates the deviation of mortality in the study group relative to the MTOS benchmark (12). The W statistic calculates the number of survivors more or less than the MTOS norm per 100 patients analyzed (23) and provides a clinical perspective for a statistically significant Z score (22).
Ethics statement
This study was approved by the institutional review board of Ajou University Hospital (IRB No. AJIRB-MED-MDB-16-005). Informed consent was waived by the board due to the observational nature of the study.
RESULTS
During the study period, a total of 244 patients with trauma were transported to the trauma center by Fire & Disaster Headquarters Helicopter. From these, 180 adult patients with blunt trauma were included in the present study. The mechanisms of injury in the patients are shown in Table 1. Motor vehicle accidents were the most common, accounting for > 50% patients, followed by falls. Of the total, 100 patients were included in Group P and 80 in Group NP. There were no differences in age between the two groups, whereas statistically significant differences were observed with regard to the severity of injury, transport time, and time from hospital arrival to operation room transfer. RTS was lower for Group P than for Group NP, whereas ISS was higher for Group P than for Group NP. Thus, the injury severity was greater for Group P than for Group NP. The transport time for Group P was twice that for Group NP (170 vs. 78 minutes; P < 0.001). However, the time from hospital arrival to operation room transfer was significantly shorter for Group P than for Group NP (105 vs. 185 minutes, P < 0.001). There were 79 (79%) and 39 (48.75%) patients with an ISS of 15+ in Groups P and NP, respectively (Table 2), with corresponding overtriage rates of 21% and 51% what means.
Table 1. Mechanisms of injury in the 180 patients enrolled in the study.
| Mechanism | All patients | Group P | Group NP |
|---|---|---|---|
| No. | 180 | 100 | 80 |
| Motor vehicle accident | 93 (51.7) | 59 (59.0) | 34 (42.5) |
| Fall | 49 (27.2) | 27 (27.0) | 22 (27.5) |
| Slip or rolling down | 14 (7.8) | 4 (4.0) | 10 (12.5) |
| Machinery | 6 (3.3) | 0 (0.0) | 6 (7.5) |
| Unspecified/NEC | 18 (10.0) | 10 (10.0) | 8 (10.0) |
The number of patients (proportions, %) are presented.
Group P, patients transported by physician-staffed helicopter emergency medical services; Group NP, patients transported by nonphysician-staffed helicopter emergency medical services; NEC, not elsewhere classifiable.
Table 2. Baseline characteristics of the study population.
| Parameters | All patients | Group P | Group NP | P value* |
|---|---|---|---|---|
| No. | 180 | 100 | 80 | |
| Men | 147 (81.7) | 84 (84.0) | 63 (78.8) | 0.367 |
| Age, yr | 51 (37–58) | 50.5 (37–58) | 52 (40–59) | 0.683 |
| RTS, points | 7.8408 (5.9672–7.8408) | 7.5500 (5.0304–7.8408) | 7.8408 (7.2186–7.8408) | < 0.001 |
| ISS, points | 20 (10–29) | 24.5 (16–35) | 14 (7–26) | < 0.001 |
| ISS > 15 | 118 (65.7) | 79 (79.0) | 39 (48.8) | < 0.001 |
| Transport time, min | 109 (60–213) | 170 (84–308) | 78 (60–120) | < 0.001 |
| ER to OR time, min | 136 (75–230) (n = 95) | 105 (60–183) (n = 59) | 185 (126–350) (n = 36) | < 0.001 |
The number of patients (proportions, %) or median values (interquartile range) are presented.
Group P, patients transported by physician-staffed helicopter emergency medical services; Group NP, patients transported by nonphysician-staffed helicopter emergency medical services; ER, emergency room; OR, operation room; IQR, interquartile range; RTS, revised trauma score; ISS, injury severity score.
*Mann-Whitney U test or χ2 analysis, as appropriate.
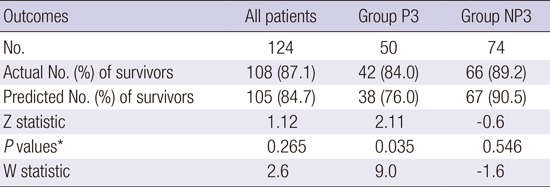
With regard to treatment outcomes assessed using TRISS, Group P patients tended to exhibit better outcomes compared with Group NP patients, although the difference was not statistically significant (W statistic, 4.6 vs. −0.9; P = 0.134 vs. 0.730). When analyzed using the W statistic, patients transported and treated through physician-staffed HEMS showed a survival potential of 5.5 more patients per 100 patients compared with those transported and treated through nonphysician-staffed HEMS, although statistically significant values were not achieved (Table 3). In Group P, the medical team implemented treatments within their reach in accordance with the ATLS® guidelines (Table 4). Although these efforts are expected to contribute to an increase in the survival rate, we did not have enough data to achieve statistically significant outcomes. During our analysis process, the authors noted that the transport time for Group P was very long compared with that for Group NP. An investigation into the transport distance was conducted to correct the problem; however, sufficient data could not be obtained because of missing detailed records of the accident scene or the unit region for recording being present in a large administrative district such as a city or province in most cases. Therefore, the transport time was determined to be modified for better comparison between the two groups. Accordingly, we implemented a subgroup analysis using data reclassified according to the transport time. We confirmed that 93% patients in Group NP (n = 74) were transported within 3 h of injury (Group NP3); therefore, only those patients that were transported within 3 h of injury in Group P (Group P3; n = 50) were selected. Groups P3 and NP3 were subjected to survival rate comparisons using TRISS. The results revealed significantly higher scores for Group P3 than for Group NP3 (Z statistic, 2.11 vs. −0.6; P = 0.035 vs. 0.546; W statistic, 9.0 vs. −1.6). In other words, if these results were literally considered, we could conclude that nine more patients could be saved per 100 patients when transportation occurred through physician-staffed HEMS within 3 hours of injury (Table 5).
Table 3. Comparison of medical treatment outcomes between Group P and Group NP on the basis of TRISS.
| Outcomes | All patients | Group P | Group NP |
|---|---|---|---|
| No. | 180 | 100 | 80 |
| Actual No. of survivors (%) | 151 (83.9) | 79 (79.0) | 72 (90.0) |
| Predicted No. of survivors (%) | 147 (81.7) | 75 (75.0) | 73 (91.3) |
| Z statistic | 1.03 | 1.50 | −0.35 |
| P value* | 0.302 | 0.134 | 0.730 |
| W statistic | 2.1 | 4.6 | -0.9 |
Group P, patients transported by physician-staffed helicopter emergency medical services; Group NP, patients transported by nonphysician-staffed helicopter emergency medical services; TRISS, trauma and injury severity score.
*Significance level for Z statistic values.
Table 4. Activities during transport by physician-staffed HEMS.
| ATLS principles | Procedures | N = 100 |
|---|---|---|
| Airway maintenance with cervical spine protection | Endotracheal intubation | 3 |
| Cervical spine immobilization | 56 | |
| Breathing and ventilation | Ambu bag | 8 |
| Mechanical ventilation | 15 | |
| Oxygen supply via nasal tube or mask | 77 | |
| Circulation with hemorrhage control | Large-caliber IV catheters and fluid resuscitation | 100 |
| CVC insertion | 12 | |
| Transfusion | 25 | |
| External hemorrhage control | 55 |
HEMS, helicopter emergency medical services; ATLS, advanced trauma life support; IV, intravenous; CVC, central venous catheter.
Table 5. Comparison of medical treatment outcomes between Group P3 and Group NP3 on the basis of TRISS.
| Outcomes | All patients | Group P3 | Group NP3 |
|---|---|---|---|
| No. | 124 | 50 | 74 |
| Actual No. (%) of survivors | 108 (87.1) | 42 (84.0) | 66 (89.2) |
| Predicted No. (%) of survivors | 105 (84.7) | 38 (76.0) | 67 (90.5) |
| Z statistic | 1.12 | 2.11 | −0.6 |
| P values* | 0.265 | 0.035 | 0.546 |
| W statistic | 2.6 | 9.0 | −1.6 |
TRISS, trauma and injury severity score; Group P3, patients transported by physician-staffed helicopter emergency medical services within 3 hours of injury; Group NP3, patients transported by nonphysician-staffed helicopter emergency medical services within 3 hours of injury.
*Significance level for Z statistic values.
DISCUSSION
The latest reported domestic preventable trauma-related mortality rate in South Korea was 35.2% (24). The authors of that study, which was published in 2012, stated that this high rate in South Korea was due to problems in rescue and medical treatment services at the prehospital stage. They further stated that the introduction of an effective transport system was essential to decrease this rate, because inappropriate care at the prehospital stage affects the mortality rate in emergency rooms at the hospital stage as well as the eventual mortality rate. To resolve these issues, the so-called Doctor Heli project was initiated under the leadership of the government in South Korea in 2011, and, as of 2015, it was ongoing at four hospitals in total (25). Under this project, patients with trauma or disease are preferentially transported from medically disadvantaged areas that are difficult to access geographically, such as remote islands. With regard to the rate of transportation of patients with severe trauma under this project (25), the numbers were 53 of 287 in 2012 (16.6%), 134 of 485 in 2013 (27.6%), and 247 of 950 in 2014 (26.0%), thus showing the trend of an annual increase. However, these services cannot be operated at night or in severe weather conditions, and there are access limitations in that helicopters cannot approach the accident scene as closely as required. Furthermore, the medical treatment outcomes for this system have not been reported (26).
The helicopter transport system used in this study was not related to the Doctor Heli project but to an EMS Helicopter project operated by an existing domestic Fire & Disaster Headquarter Helicopter. The helicopter provided under this project can operate at night and is relatively less vulnerable in severe weather conditions. Furthermore, it has easier access to the accident scene with the help of firefighting professionals. However, despite all these advantages, there have been few domestic studies on helicopter transport with dominant intervention by a medical team using firefighting helicopters. In particular, there are no studies on physician-staffed HEMS.
For more than 20 years now, advanced countries have been conducting several studies on the importance of physician intervention at the prehospital stage, particularly during helicopter transport, and the associated positive effects. Osterwalder (27) reported that intervention by an emergency physician at the prehospital stage can decrease the mortality rate for patients with blunt polytrauma exhibiting an ISS of ≥ 8. Schmidt et al. (17) compared two groups of patients with the same ISS who were transported by helicopter transport with a medical doctor or a paramedic on board. They reported that very difficult procedures such as intravenous fluid therapy, endotracheal intubation, and chest tube insertion were implemented more frequently in the group with a medical doctor on board, and this decreased the initial mortality rate and increased the overall survival rate. According to Garner et al. (28), during the helicopter transports of patients with blunt trauma and an ISS of ≥ 10, the mortality rate was significantly lower when a team of physicians was on board than when a team of paramedics was on board. The positive effects of physician-staffed HEMS were also confirmed in the present study. Because of the relatively initial stages of the project in South Korea, the number of patients in the present study was relatively small compared to that in foreign studies. However, analysis using TRISS revealed that nine more patients could survive per 100 patients when transportation occurred through physician-staffed HEMS within 3 hours of injury (W statistic, 9.0; P = 0.035). Although the transport time was noticeably longer for patients transported by physician-staffed HEMS than for those transported by nonphysician-staffed HEMS, this was compensated by the fact that the time from hospital arrival to operation room transfer was significantly shorter for the former group.
Physician-staffed HEMS can be operated differently in accordance with the emergency medical system in a region or nation (29). It can be largely divided into the Anglo-American system and the Franco-German system (30). In the Anglo-American system, which is based on the “scoop and run” concept and is led by the United States, well-trained paramedics take charge of treatment during helicopter transport, whereas in the Franco-German system, which is based on the “stay and play” concept, typical physician-staffed HEMS dispatch physicians directly to the accident scene. The better system of the two remains controversial; however, it is evident that the system has to be established in harmony with the existing emergency medical system in the region or nation. However, under the current domestic circumstances, where emergency medical technicians are not well organized or trained and where there are many legal limitations in the prehospital treatment process. For example, under the current domestic law related to the emergency medical technicians, they are not able to do any interventions to severe trauma patients except for simple oxygen supply and oropharyngeal airway insertion unless physicians order them. Therefore, a system involving direct intervention of physicians such as the ATLS procedures during the transport by physician-staffed HEMS in the study is preferable in Korea. The results of the present study, despite its retrospective nature, small sample size, and single-institution design, allow us to expect an increased survival rate if physician-staffed HEMS are immediately implemented for patients with severe trauma under the current domestic trauma patient transport system.
This study has a few limitations. First, no distinction was made between the patients transported directly from the accident scene and the cases via other facilities before arrival at the trauma center in Group P. This is one of the greatest limitations of the study, yet it represents the current circumstances of the domestic emergency medical system, wherein timely transport of patients with severe trauma to an appropriate hospital where definite care can be provided is not in place. Second, the time limit of 3 hours after injury used for subgroup analysis was an arbitrary value taken by the authors. This was not a calculated value obtained through statistical analysis; it was simply drawn from the fact that most patients in Group NP (93%) were transported within 3 hours of injury. In other words, the 3-hour cut-off was used because the number of patients transported within 2 hours was too small to obtain statistically significant values. As a result, a relatively lower number of patients were placed into group P3 (50.0%, 50 of 100) compared to Group NP (7.5%, 6 of 80). This was because the decision to transport most of the Group P patients to a higher level facility was delayed due to imaging work-up in the smaller local hospital. On the other hand, most patients of Group NP were transported to our hospital directly within 3 hours without visiting other facility by the decision of paramedics from the Firefighter Department. The third limitation is the use of vital signs and GCS scores initially measured by the trauma center medical team for TRISS calculations. In other similar studies (31), prehospital data were applied for TRISS calculations, whereas in the present study, vital signs and GCS scores initially measured by the trauma center medical team, not those measured at the prehospital stage or at the accident scene, were used for patients transported via intermediate facilities. This is because precise values for physiological parameters were difficult to obtain before arrival at the trauma center and were consequently inaccurate.
To our knowledge, our study, despite its single-center design and a few limitations, is the first to evaluate the outcomes of physician-staffed HEMS involving the direct intervention of medical doctors at the prehospital transport stage in South Korea. In particular, our results indicate that better treatment outcomes can be expected if dedicated trauma resuscitation teams actively intervene in the medical treatment process from the transport stage and if patients are transported to a hospital to receive definitive care within 3 hours of injury. The authors anticipate that this study will trigger interest in the helicopter transport systems of exclusive medical teams in trauma centers that are in the process of getting established throughout the country, and that forward-thinking multidisciplinary studies will be conducted on physician-staffed HEMS in Korea in the near future.
ACKNOWLEDGMENT
The authors would like to thank the pilots and emergency medical technicians of Gyeonggi Province Fire and Disaster Headquarters / Aviation Team for their dedication to saving trauma victims' lives.
Footnotes
DISCLOSURE: The authors have no potential conflicts of interest to disclose.
AUTHOR CONTRIBUTION: Conception and coordination of the study: Jung K, Huh Y. Physician-Staffed HEMS Members: Jung K, Huh Y, Lee JC, Kim Y, Moon J, Youn SH. Acquisition of data: Jung K, Huh Y, Kim J, Kim TY, Kim J, Kim H. Analysis and interpretation of data: Jung K, Huh Y, Moon J, Youn SH, Kim Y. Statistical analysis: Jung K, Huh Y, Kim J. Critical review and editing: Jung K, Huh Y, Lee JC. Manuscript preparation: Jung K, Huh Y. Manuscript approval: all authors.
References
- 1.National Emergency Center (KR) Emergency medical service annual report 2012 [Internet] [accessed on 2 September 2013]. Available at http://www.nemc.or.kr/egen/inf.emb13.do.
- 2.Trunkey DD, Lim RC. Analysis of 425 consecutive trauma fatalities: an autopsy study. J Am Coll Emerg Physician. 1974;3:368–371. [Google Scholar]
- 3.West JG, Trunkey DD, Lim RC. Systems of trauma care. A study of two counties. Arch Surg. 1979;114:455–460. doi: 10.1001/archsurg.1979.01370280109016. [DOI] [PubMed] [Google Scholar]
- 4.Cales RH. Trauma mortality in Orange County: the effect of implementation of a regional trauma system. Ann Emerg Med. 1984;13:1–10. doi: 10.1016/s0196-0644(84)80375-3. [DOI] [PubMed] [Google Scholar]
- 5.Cales RH, Trunkey DD. Preventable trauma deaths. A review of trauma care systems development. JAMA. 1985;254:1059–1063. doi: 10.1001/jama.254.8.1059. [DOI] [PubMed] [Google Scholar]
- 6.Giannakopoulos GF, Kolodzinskyi MN, Christiaans HM, Boer C, de Lange-de Klerk ES, Zuidema WP, Bloemers FW, Bakker FC. Helicopter emergency medical services save lives: outcome in a cohort of 1073 polytraumatized patients. Eur J Emerg Med. 2013;20:79–85. doi: 10.1097/MEJ.0b013e328352ac9b. [DOI] [PubMed] [Google Scholar]
- 7.Thomas SH, Harrison TH, Buras WR, Ahmed W, Cheema F, Wedel SK. Helicopter transport and blunt trauma mortality: a multicenter trial. J Trauma. 2002;52:136–145. doi: 10.1097/00005373-200201000-00023. [DOI] [PubMed] [Google Scholar]
- 8.Taylor C, Jan S, Curtis K, Tzannes A, Li Q, Palmer C, Dickson C, Myburgh J. The cost-effectiveness of physician staffed helicopter emergency medical service (HEMS) transport to a major trauma centre in NSW, Australia. Injury. 2012;43:1843–1849. doi: 10.1016/j.injury.2012.07.184. [DOI] [PubMed] [Google Scholar]
- 9.Taylor CB, Stevenson M, Jan S, Middleton PM, Fitzharris M, Myburgh JA. A systematic review of the costs and benefits of helicopter emergency medical services. Injury. 2010;41:10–20. doi: 10.1016/j.injury.2009.09.030. [DOI] [PubMed] [Google Scholar]
- 10.Yoon YH, Moon SW, Lee SW, Choi SH, Cho HJ, Kim JY. Helicopter emergency medical services: a report on the current status in a metropolitan area of South Korea. Eur J Emerg Med. 2011;18:176–178. doi: 10.1097/MEJ.0b013e32834007be. [DOI] [PubMed] [Google Scholar]
- 11.American College of Surgeons Committee on Trauma. Advanced Trauma Life Support®: Student Course Manual. 9th ed. Chicago, IL: American College of Surgeons; 2012. [Google Scholar]
- 12.Champion HR, Copes WS, Sacco WJ, Lawnick MM, Keast SL, Bain LW, Jr, Flanagan ME, Frey CF. The Major Trauma Outcome Study: establishing national norms for trauma care. J Trauma. 1990;30:1356–1365. [PubMed] [Google Scholar]
- 13.Champion HR, Sacco WJ, Copes WS. Injury severity scoring again. J Trauma. 1995;38:94–95. doi: 10.1097/00005373-199501000-00024. [DOI] [PubMed] [Google Scholar]
- 14.Baxt WG, Moody P. The impact of a physician as part of the aeromedical prehospital team in patients with blunt trauma. JAMA. 1987;257:3246–3250. [PubMed] [Google Scholar]
- 15.Hamman BL, Cué JI, Miller FB, O'Brien DA, House T, Polk HC, Jr, Richardson JD. Helicopter transport of trauma victims: does a physician make a difference? J Trauma. 1991;31:490–494. doi: 10.1097/00005373-199104000-00007. [DOI] [PubMed] [Google Scholar]
- 16.Burney RE, Passini L, Hubert D, Maio R. Comparison of aeromedical crew performance by patient severity and outcome. Ann Emerg Med. 1992;21:375–378. doi: 10.1016/s0196-0644(05)82653-8. [DOI] [PubMed] [Google Scholar]
- 17.Schmidt U, Frame SB, Nerlich ML, Rowe DW, Enderson BL, Maull KI, Tscherne H. On-scene helicopter transport of patients with multiple injuries--comparison of a German and an American system. J Trauma. 1992;33:548–553. doi: 10.1097/00005373-199210000-00010. [DOI] [PubMed] [Google Scholar]
- 18.Baxt WG, Moody P. The impact of a rotorcraft aeromedical emergency care service on trauma mortality. JAMA. 1983;249:3047–3051. [PubMed] [Google Scholar]
- 19.Bartolacci RA, Munford BJ, Lee A, McDougall PA. Air medical scene response to blunt trauma: effect on early survival. Med J Aust. 1998;169:612–616. doi: 10.5694/j.1326-5377.1998.tb123435.x. [DOI] [PubMed] [Google Scholar]
- 20.Boyd CR, Tolson MA, Copes WS. Evaluating trauma care: the TRISS method. Trauma score and the injury severity score. J Trauma. 1987;27:370–378. [PubMed] [Google Scholar]
- 21.Champion HR, Sacco WJ, Copes WS, Gann DS, Gennarelli TA, Flanagan ME. A revision of the trauma score. J Trauma. 1989;29:623–629. doi: 10.1097/00005373-198905000-00017. [DOI] [PubMed] [Google Scholar]
- 22.Champion HR, Copes WS, Sacco WJ, Lawnick MM, Keast SL, Bain LW, Jr, Flanagan ME, Frey CF. The major trauma outcome study: establishing national norms for trauma care. J Trauma. 1990;30:1356–1365. [PubMed] [Google Scholar]
- 23.Younge PA, Coats TJ, Gurney D, Kirk CJ. Interpretation of the Ws statistic: application to an integrated trauma system. J Trauma. 1997;43:511–515. doi: 10.1097/00005373-199709000-00021. [DOI] [PubMed] [Google Scholar]
- 24.Kim H, Jung KY, Kim SP, Kim SH, Noh H, Jang HY, Yoon HD, Heo YJ, Ryu HH, Jeong TO, et al. Changes in preventable death rates and traumatic care systems in Korea. J Korean Soc Emerg Med. 2012;23:189–197. [Google Scholar]
- 25.National Emergency Center (KR) Emergency medical service annual report 2014 [Internet] [accessed on 31 December 2015]. Available at http://www.nemc.or.kr/egen/inf.emb13.do.
- 26.National Emergency Center (KR) Report for result of helicopter emergency medical service support project [Internet] [accessed on 31 December 2015]. Available at http://www.1339.or.kr/egen/inf.fai52.do?flag=8&strid=72770&strnum=6.
- 27.Osterwalder JJ. Mortality of blunt polytrauma: a comparison between emergency physicians and emergency medical technicians—prospective cohort study at a level I hospital in eastern Switzerland. J Trauma. 2003;55:355–361. doi: 10.1097/01.TA.0000034231.94460.1F. [DOI] [PubMed] [Google Scholar]
- 28.Garner A, Rashford S, Lee A, Bartolacci R. Addition of physicians to paramedic helicopter services decreases blunt trauma mortality. Aust N Z J Surg. 1999;69:697–701. doi: 10.1046/j.1440-1622.1999.01688.x. [DOI] [PubMed] [Google Scholar]
- 29.Salomone JP, Salomone JA., 3rd . Prehospital care. In: Mattox KL, Moore EE, Feliciano DV, editors. Trauma. 7th ed. New York, NY: McGraw-Hill; 2013. pp. 100–122. [Google Scholar]
- 30.Dick WF, Franco-German Emergency Medical Services System Anglo-American vs. Franco-German emergency medical services system. Prehosp Disaster Med. 2003;18:29–35. doi: 10.1017/s1049023x00000650. [DOI] [PubMed] [Google Scholar]
- 31.Meizoso JP, Valle EJ, Allen CJ, Ray JJ, Jouria JM, Teisch LF, Shatz DV, Namias N, Schulman CI, Proctor KG. Decreased mortality after prehospital interventions in severely injured trauma patients. J Trauma Acute Care Surg. 2015;79:227–231. doi: 10.1097/TA.0000000000000748. [DOI] [PubMed] [Google Scholar]


