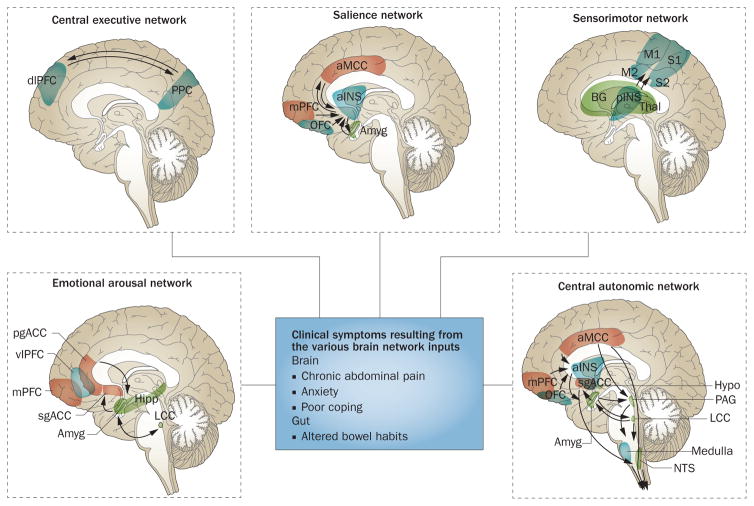
Figure 2.
Brain networks contributing to IBS symptoms. Depicted are task-related brain networks that have been described in the literature and for which structural and functional alterations have been reported in patients wiht IBS. The box in the centre describes the clinical symptoms related to the network inputs. Outputs most relevant for IBS pathophysiology occur in the form of descending pain modulation and autonomic nervous system activity. Abbreviations: Amyg, amygdala; aINS, anterior insula; aMCC, anterior midcingulate cortex; BG, basal ganglia; dlPFC, dorsolateral prefrontal cortex; Hipp, hippocampus; Hypo, hypothalamus; LCC, locus coeruleus complex; M1, primary motor cortex; M2, supplementary motor cortex; mPFC, medial prefrontal cortex; NTS, solitary nucleus; OFC, orbitofrontal cortex; PAG, periaqueductal grey; pgACC, pregenual anterior cingulate cortex; pINS, posteria insula; PPC, posterior parietal cortex; sgACC, subgenual anterior cingulate cortex; Thal, thalamus; vlPFC, ventrolateral prefrontal cortex.