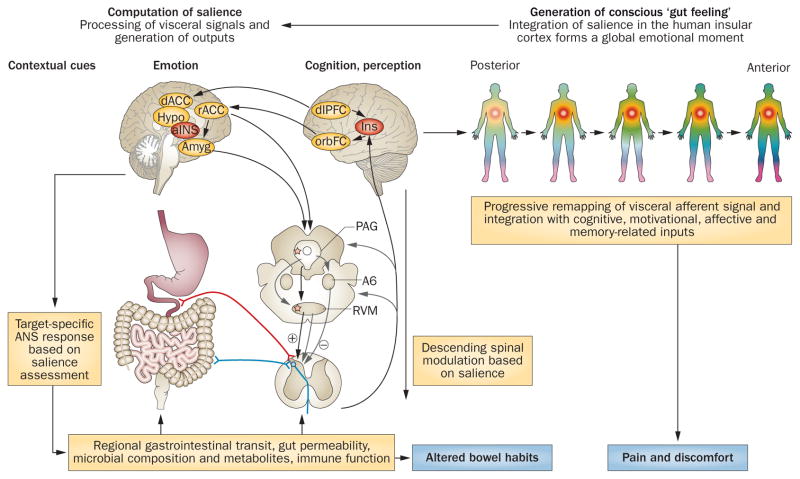
Figure 3.
Cross-sectional integrated brain–gut model of IBS pathophysiology. Proposed model for involvement of brain–gut axis in the generation of cardinal IBS symptoms (chronic abdominal pain associated with altered bowel habits). Under normal circumstances, visceral and external signals are evaluated by the salience network, which generates brain outputs in terms of targeted ANS responses (regulating gastrointestinal and immune function) and descending pain modulatory activity (regulating pain sensitivity at the dorsal horn level). Target organ alterations (either peripherally or ANS stimulated) are signalled back to the brain via neural, endocrine or immune-related channels. These signals are processed within subregions of the INS, and depending on their subjective salience, are consciously perceived (associated with activation of anterior INS) as normal gut sensations, discomfort or pain. IBS symptoms can arise from several primary peripheral or central mechanisms, but once brain–gut interactions are altered, causality is difficult to determine. Abbreviations: Amyg, amygdala; ANS, autonomic nervous system; dACC, dorsal anterior cingulate cortex; dlPFC, dorsolateral prefrontal cortex; Hypo, hypothalamus; INS, insula; orbFC, orbitofrontal cortex; PAG, periaqueductal grey; rACC, rostral anterior cingulate cortex; RVM, rostral ventromedial medulla.