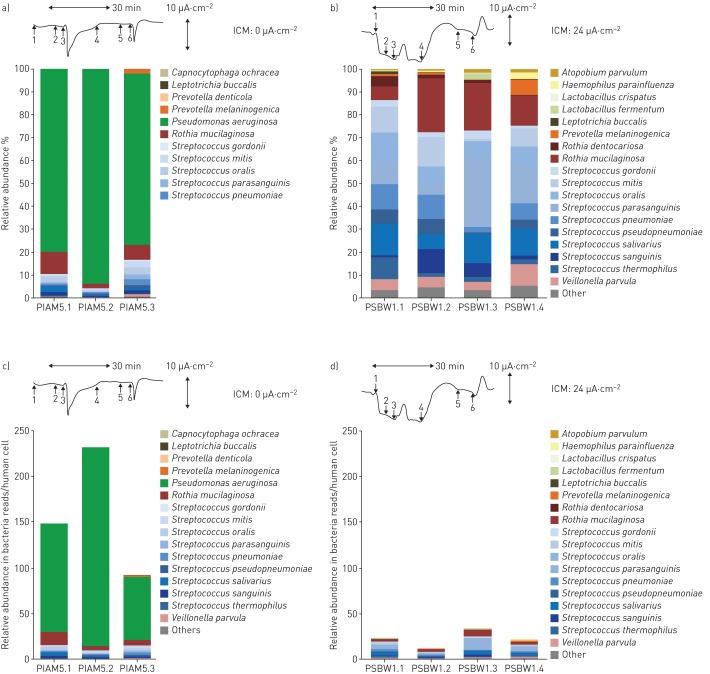
FIGURE 6.
Bacterial sputum microbiomes of a, c) an exocrine pancreas insufficient (PI) cystic fibrosis (CF) patient who is homozygous for the most common cystic fibrosis transmembrane conductance regulator (CFTR) mutation p.Phe508del and b, d) an exocrine pancreas sufficient (PS) CF patient who is homozygous for the rare splice mutation in the CFTR gene c.1766+3 A-G. Data are presented as a, b) stacked bar charts of relative abundance as fractions of total bacterial reads or c, d) number of bacterial reads per human cell. Whereas the normalised bacterial microbiomes (a, b) suggest unrelated compositions of the bacterial communities in the respiratory tracts of the two patients, the normalisation per human cell (c, d) unravels similar colonisation modes with anaerobes in the two patients, which are overshadowed by the dominant Pseudomonas aeruginosa community in the PI patient. Tracings show original recordings of short circuit currents in rectal suction biopsies [22] to characterise the basic defect and CFTR function in the two individuals with CF. The horizontal arrow corresponds to a recording time of 30 min and the vertical arrow to a current of 10 µA·cm−2. Intestinal current measurements (ICM) were performed per protocol [22] by the addition of amiloride (1), indomethacin (2), carbachol (3), cAMP/forskolin (4), 4,4'-diisothiocyanostilbene-2,2'-disulfonic acid (DIDS) (5) and histamine (6). Carbachol, cAMP/forkolin and histamine induce chloride secretory responses seen in the ICM by signals in the upward direction. The tracings show either no (a, c) or intermediate (b, d) CFTR activity, indicated by the cumulative chloride currents (0 or 24 µA·cm−2) which implies that no functional CFTR is operating in the PI CF patient whereas substantial residual CFTR activity is present in the PS CF patient.