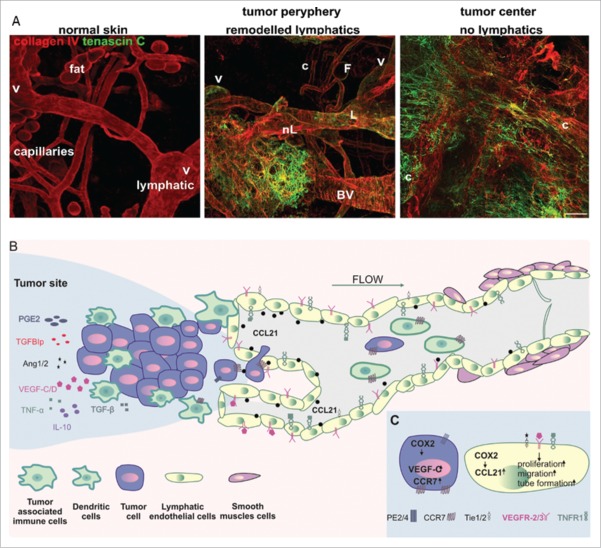
Figure 1.
(A) The lymphatic vessel in normal and mouse melanoma tumor tissue. Left. In normal skin, basement membrane-supported lymphatic vessels (L) can be morphologically distinguished after identification of intravascular valves (V) from blood capillaries (c) and adipocytes (F). Normal tissue is also free from tenascin C, extracellular matrix characteristic for tumor remodeled tissue. Middle. At the tumor margin, new extracellular matrix is deposited and pre-existing lymphatic (L) and blood vessels (BV) are remodeled. Also, new, poorly organized vessels are formed (nL). Right. In the center of the tumor, deposition of new matrix paralleled the loss of organized tissue architecture with large tortuous granulation tissue-like blood (c) vessels and a collapse of lymphatics. (B) The overview of LECs, tumor and tumor-associated immune cells' interactions during tumor lymphangiogenesis and lymphatic vessels enlargement. Secretion of a variety of cytokines and growth factors mobilize tumor cells as well as dendritic cells to get inside the initial lymphatic vessels. (C) COX-2 increases level of prostaglandin receptor (EP2) and enhances expression of VEGF-C, CCR7 as well as CCL21. Binding of VEGFR-3, Tie1/2 and TNFR1 ligands induces LECs proliferation and capability of tube formation.