Figure 1.
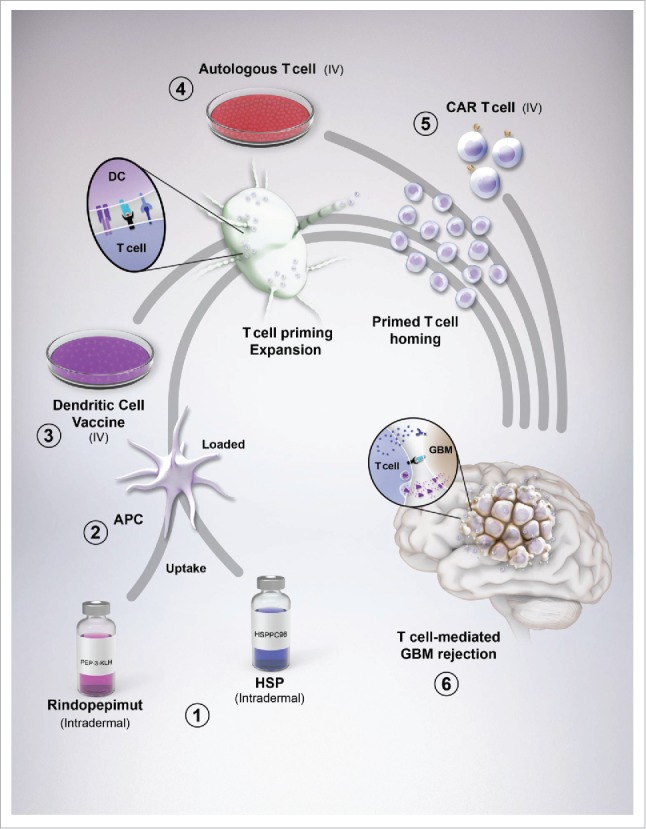
Glioblastoma (GBM) vaccines and their interaction with immunity. (1) Rindopepimut (RINTEGA), a synthetic peptide vaccine targeted at the EGFRvIII mutation, and HSPPC-96 (Prophage), an autologous-derived complex consisting of heat shock proteins complexed with GBM antigens, are intradermally injected for uptake by resident dendritic cells (DC). (2) The vaccines are co-administered with adjuvants, such as GM-CSF and keyhole limpet hemocyanin (with respect to RINTEGA) for stimulating DC uptake, antigen processing and upregulation of costimulatory molecules. (3) Peripheral blood mononuclear cells can be isolated from patient blood (not shown), expanded in culture, primed with autologous patient-derived GBM tumor lysate, followed by intravenous transfer back into the patient, bypassing the need for dermal injection of tumor antigens. Regardless of whether DCs are primed and loaded in culture, or a cutaneous route, DC drain to lymphoid tissue for subsequent T cell activation and expansion. (4) Similar to PBMC isolation for DC preparation, autologous T cells can also be isolated from this pool. These cells can be (re-)stimulated with plate-bound anti-human CD3ϵ, without anti-CD28, as to only (re-)engage the experience T cells that might respond to TAAs. This CD3ϵ-targeted stimulation can be further boosted by adding in cytokines that favor a proinflammatory/antitumor T cell subset such as IL-2, IL-12 and IL-15. (5) An alternative to simple autologous T cell isolation, (re-)priming and expansion, is by engineering the T cell to be highly specific to a GBM-expressed antigen, in the form of a chimeric antigen receptor-expressing T cell. This step provides a high level of stringency and targeting for all T cell adoptively transferred into the GBM patient. Ultimately, the goal of all vaccines is to eventually cause GBM-specific T cells to infiltrate the tumor and elicit immune-mediated rejection.
