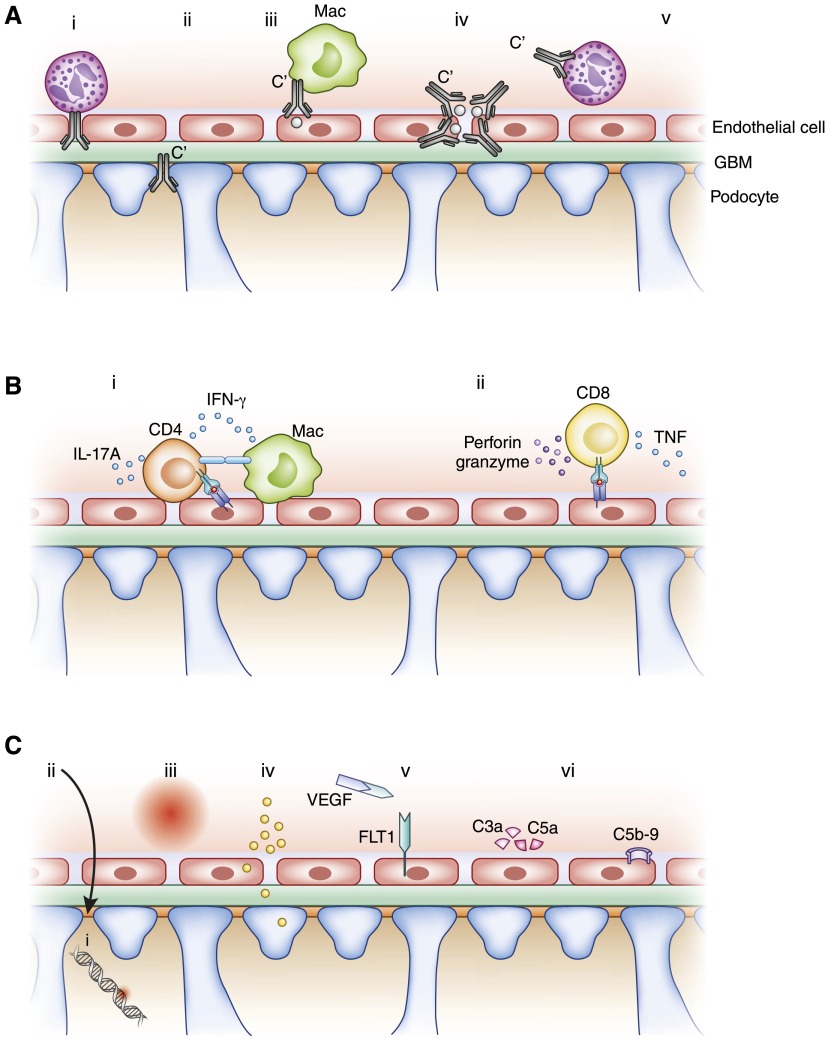
Figure 2.
Simplified diagrammatic representation of a selection of mechanisms of glomerular injury. (A) Antibody-mediated glomerular injury. From left to right, (i) neutrophils (shown) and macrophages induce injury after anti-α3(IV)NC1 autoantibodies bind to the GBM in anti-GBM GN; (ii) in membranous glomerulopathy autoantibodies against PLA2R1 (and other antigens) on podocytes are deposited subepithelially, with the involvement of complement; (iii) antibodies can bind to antigens lodged in the glomerulus (grey dots) with recruitment of macrophages (shown) and neutrophils, and the activation of complement; (iv) circulating immune complexes can be deposited in glomeruli, activate complement, and recruit leukocytes; (v) ANCA, (with complement) activates neutrophils and enables their recruitment to the glomerulus. Not shown, but important, is IgA deposition in mesangial areas. (B) Cell-mediated immune mechanisms. (i) Effector CD4+ cells (often Th1 or Th17 type) recognize antigens that can be intrinsic to or planted in the glomeruli. This occurs via their T cell receptor recognizing MHC class II peptide complexes (several cell types could possibly be involved in this process). Activated T cells produce cytokines (IL-17A and IFN-γ as examples) that have direct effects on intrinsic kidney cells and activate, together with costimulatory molecules (e.g., CD154/CD40), innate leukocytes such as macrophages. Not shown are interactions between intrinsic renal cells and T cells that include costimulation and cytokines. (ii) CD8+ cells can recognize antigenic peptides with MHC class I on intrinsic cells and secrete cytokines or induce cell death. (C) Metabolic, vascular, and other mechanisms of injury. Podocyte and foot process injury and dysfunction occurs due to (i) genetic abnormalities of slit diaphragm proteins and (ii) in minimal change disease and FSGS due to circulating permeability factors. Metabolic factors such as (iii) systemic and intraglomerular hypertension and (iv) hyperglycemia and its consequences are common, and affect both the cells and the structural components of the glomerulus. Both glomerular endothelial cell and podocyte injury are important consequences of preeclampsia, involved a number of mediators including soluble fms-like tyrosine kinase-1. C3 glomerulopathy, as well as some types of atypical hemolytic uremic syndrome (vi), can be induced by autoantibodies to, or genetic abnormalities in, complement regulatory proteins, resulting in complement activation. α3(IV)NC1, the non-collagenous domain of the α3 chain of type IV collagen; FLT1, fms-like tyrosine kinase-1; GBM, glomerular basement membrane; Mac, macrophage; M-type PLA2R1, phospholipase A2 receptor 1; Th, T helper; VEGF, vascular endothelial growth factor.