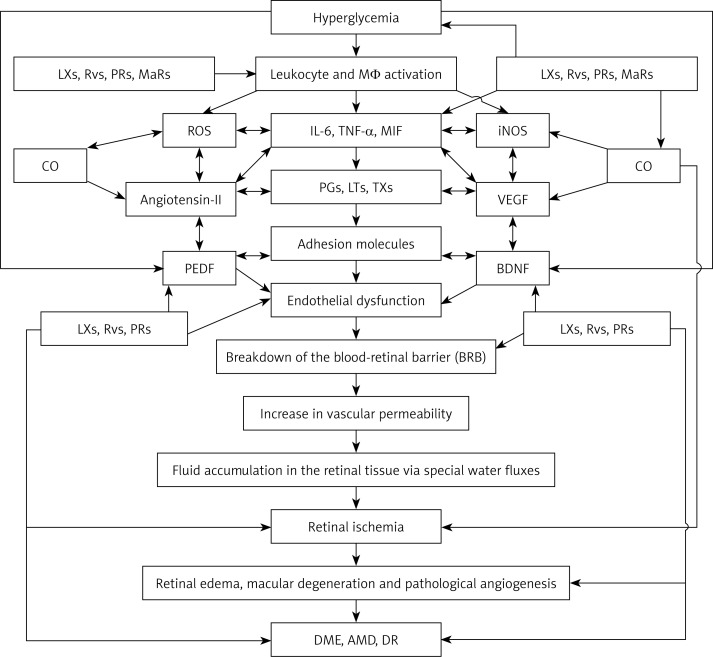
Figure 5.
Scheme showing possible sequence of events that lead to the development of DME, DR and AMD. Hyperglycemia causes activation of leukocytes, macrophages and lymphocytes, resulting in increased production of reactive oxygen species (ROS) and pro-inflammatory IL-6, TNF-α, macrophage migration inhibitory factor (MIF) and other cytokines. These cytokines also enhance ROS production and enhance the production and release of pro-inflammatory eicosanoids ((prostaglandins (PGs), leukotrienes (LTs) and thromboxanes (TXs)) by activating cell membrane bound phospholipase A2 (PLA2) that induces the release of polyunsaturated fatty acids: arachidonic acid (AA), eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), which are precursors of PGs, LTs and TXs. IL-6, TNF-α, MIF, PGs, LTs and TXs enhance the expression of adhesion molecules, which leads to adhesion of leukocytes to endothelial cells, resulting in endothelial dysfunction due to the action of ROS released by adherent leukocytes on endothelial cells. Eicosanoids, cytokines, ROS and endothelial dysfunction can cause breakdown of the blood-retinal barrier, resulting in increased vascular permeability and fluid accumulation in the retinal tissue via special water fluxes. This leads to retinal ischemia and increased production of VEGF and pathological angiogenesis, events that result in the initiation and progression of retinal edema, macular degeneration and DR. Increased production of IL-6, TNF-α, MIF, and eicosanoids also induces enhanced production of VEGF and iNOS, which have pro-inflammatory actions and so are capable of producing endothelial dysfunction, retinal ischemia and pathological angiogenesis. Leukocytes are activated, and when diabetes is associated with hypertension there could be enhanced production of angiotensin-II, which has pro-inflammatory actions. Angiotensin-II is capable of enhancing ROS generation by leukocytes and stimulates increased production of IL-6, TNF-α and MIF and pro-inflammatory eicosanoids. Under normal physiological conditions, AA, EPA and DHA can also give rise to the formation of anti-inflammatory lipoxins (LXs), resolvins (RVs), protectins (PRs) and maresins (MaRs), which suppress leukocyte activation, ROS generation, PGs, LTs and TXs, formation of angiotensin-II, VEGF production and activation of iNOS. These events would ultimately result in suppression of inflammation and preservation of the blood retinal barrier and prevention of retinal ischemia and thus amelioration of DME, DR and AMD. Lipoxins, resolvins and protectins enhance the production of CO, a vasodilator and anti-inflammatory gas that also has cytoprotective properties. CO can suppress the production of ROS. PEDF produced by retinal pigment epithelial cells has anti-inflammatory, cytoprotective and anti-oxidant properties and is capable of protecting retinal cells and thus preventing DME, AMD and DR. Hyperglycemia suppresses the production of PEDF and thus may initiate the onset of DME, DR and AMD. It is not yet known whether PEDF can enhance the formation of lipoxins, resolvins and protectins and vice versa, though this is a distinct possibility. PEDF suppresses the formation of ROS, IL-6, TNF-α and MIF and expression of adhesion molecules and preserves the blood retinal barrier. BDNF is another neurotrophic factor that preserves retinal cell integrity, enhances formation of lipoxins, resolvins, protectins and maresins and prevents DME, DR and AMD. For details see the text