Abstract
Radiation dose monitoring in medical imaging examination areas is mandatory for the reduction of patient radiation exposure. Recently, dose monitoring techniques that use digital imaging and communications in medicine (DICOM) dose structured reports (SR) have been introduced. The present paper discusses the setup of a radiation dose monitoring system based on DICOM data from university hospitals in Korea. This system utilizes the radiation dose data-archiving method of standard DICOM dose SR combined with a DICOM modality performed procedure step (MPPS). The analysis of dose data based on a method utilizing DICOM tag information is proposed herein. This method supports the display of dose data from non-dosimeter-attached X-ray equipment. This system tracks data from 62 pieces of equipment to analyze digital radiographic, mammographic, mobile radiographic, CT, PET-CT, angiographic, and fluorographic modalities.
Keywords: Radiation exposure, DICOM dose SR, DICOM MPPS, Radiation dose monitoring, Hospital information system
Introduction
Patients are exposed to X-rays when undergoing medical examinations in diagnostic radiology. Medical examinations based on X-rays are acknowledged worldwide as essential tools for improving human health; however, they also represent, by far, the largest manmade source of radiation exposure [1].
Digital radiographic technology can reduce the potential risks of medical radiation exposure to patients and increase image utility. However, concerns regarding the unnecessary radiation exposure that may result from operator inexperience or lack of understanding of the digital radiographic process have been raised. The International Commission on Radiological Protection (ICRP) indicated in Publication 93 that the ease of obtaining and deleting images during digital angiography was accompanied by a tendency among clinical users to take a larger number of images [2].
Digital radiographic systems contribute to patient radiation exposure information archives, thus also supporting digital information and communications in medicine (DICOM) header information, modality performed procedure step (MPPS) technology, and DICOM dose structured reports (SRs) [3, 4]. A document on medical radiation dose monitoring to introduce the standards of medical radiation dose monitoring by DICOM and the fundamentals of a national dose registry has been published by the Integrated Healthcare Enterprise (IHE) [5].
The International Atomic Energy Agency (IAEA) initiated the Smart Card project in 2006 with the objective of developing a flexible template for tracking cumulative medical radiation exposure, including dose information for individual procedures whenever possible [6–8].
Since the Fukushima Daiichi Nuclear Power Plant accident, interest in medical radiation has increased among medical staff and patients. The MFDS (Ministry of Food and Drug Safety in Korea) conducted a survey to accurately determine medical radiation exposure. According to MFDS reports, the amount of medical exposure fluctuated by 10–30 times for the same radiological examination conducted at different institutions. Therefore, it is essential to efficiently manage and control the medical exposure so as to reduce unnecessary patient exposure and to alert medical staff to this exposure.
One of the first attempts to use digital technology in Europe for patient dose management was made in 1999, when the first digital generators and digital imaging systems were installed in several hospitals. It then became possible to transfer radiographic exposure conditions and geometric data to PCs and to calculate entrance surface air kerma from the X-ray output curves [9].
In 2012, the Ministry of Food and Drug Safety of Korea independently developed CT radiation dose estimation software. This software accurately estimates CT dose information but does not correctly estimate the dose information for other modalities. The purpose of the present study is to develop the first real-time radiation dose monitoring system for various modalities at a university hospital in Korea.
Materials and Methods
Radiation Dose Actuation of Digital X-ray Systems
This study examined 17 general digital X-ray systems, two digital mammography systems, and 14 portable X-ray systems found in these hospitals. Among the general X-ray devices used, roughly 20 % had dose area product (DAP) meters so that they could send the DAP dose and DICOM information to the development system, and all of the digital mammography systems were able to send both DAP information and organ dose information.
The rest of the systems did not send DAP information. In these systems, each exposure dose was estimated by obtaining the DICOM information, and this estimated dose information was saved in the database of the developed system by matching the examination name and dose information. The examination name, dose value, and patient demographic information were obtained for each exposure.
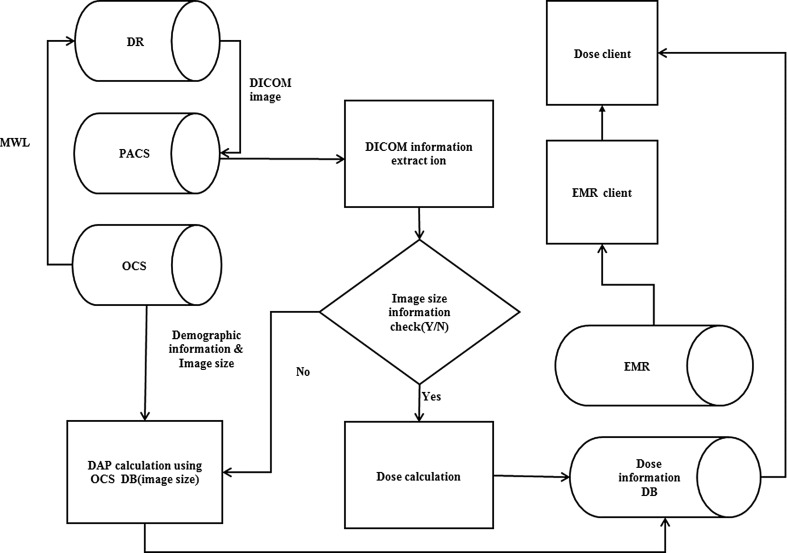
To estimate the doses in general X-ray systems, tube voltage, tube current, focal-spot area, filtration, and source-to-image distance (SID) information was obtained from the DICOM information and then used for the calculations. The model for dose information acquisition from a general X-ray system is shown in Fig. 1.
Fig. 1.
Dose monitoring mode using DICOM information for general X-ray equipment. DR digital radiology, PACS picture archiving and communication system, OCS order communication system, DAP dose area product, DICOM digital image and communications in medicine, EMR electronic medical record
In addition, to estimate the dose information, automatic calculations were performed by the system using the incident air kerma equation from Edmonds et al. [18]:
| 1 |
where T is the total filtration in mm of aluminum and the source to skin distance (SSD) is measured in cm. In the developed system, the exposure area was using in the Edmonds et al. incident air kerma equation, and then, the DAP correction factor was applied based on the particular features of the system. It was not problematic to extract the radiation field area with the device that included a DAP meter; however, it was difficult to calculate the DAP values without using a DAP meter. Therefore, the radiation field area was input during the OCS prescription stage such that if the examination were prescribed, the radiation field area would be automatically set. The effective dose was calculated using the estimated DAP for each examination via the equation:
| 2 |
where ED is the effective dose in mSv, DAP is the dose area product in Gy cm2, and k is the conversion factor. Using this methodology, ED can be estimated from the DAP, which is reported for the general X-ray, angiography, and fluorography systems. In this study, the dose information was recorded as follows: for DR and CT, the DAP was recorded; for CT, the dose length product (DLP) was recorded; and for mammography, the organ dose was recorded. Using the appropriate effective dose (ED) conversion factor from ICRP103, the ED was recorded. In case an examination was not justified in ICRP103, a DAP-to-ED conversion factor provided by NPRB was used, and the calculated ED value was recorded. The DAP-to-ED conversion factors are shown in Table 1.
Table 1.
Normalized effective dose per dose length product for adult (standard physique) and pediatric patients of various ages over various body regions. Conversion factor for adult and pediatric patients assumes the use of a 16-cm-diameter head CT dose phantom. All other conversion factors assume the use of a 32-cm-diameter CT body phantom [10, 11]
| Region of body | K (mSv mGy−1 cm−1) | ||||
|---|---|---|---|---|---|
| 0 year old | 1 year old | 5 years old | 10 years old | Adult | |
| Head/neck | 0.013 | 0.0085 | 0.0057 | 0.0042 | 0.0031 |
| Head | 0.011 | 0.0067 | 0.0040 | 0.0032 | 0.0021 |
| Neck | 0.017 | 0.012 | 0.011 | 0.079 | 0.0059 |
| Chest | 0.039 | 0.026 | 0.018 | 0.013 | 0.014 |
| Abdomen/pelvis | 0.049 | 0.030 | 0.020 | 0.015 | 0.015 |
| Trunk | 0.044 | 0.028 | 0.019 | 0.014 | 0.015 |
For DAP measurements, a DAP meter (DAP W2, PEHA MED, Germany) was used at the hospital.
The expanded relative uncertainty at k = 2 (k is the coverage factor; and k = 2 indicates a 95 % confidence interval) in the DAP measurements was estimated as ±8 % for DAP results. These estimates of uncertainty in the DAP measurements are still well below the maximum acceptable combined standard uncertainty (k = 2) of ±25 %, as stipulated in the international standard IEC 60580 for DAP meters.
Acquisition of CT Dose Information
In the developed system, the exposure dose data was acquired for seven CT systems. To acquire this data, first, the radiation dose information was obtained, both in the DICOM dose SR and DICOM MPPS. Then, the dose information was obtained from the CT DICOM image dose report. The dose data was then saved in the database [12, 13]. In this system, the radiation dose information was multiplied by a factor k to allow calculation of the effective dose via the equation [14]:
| 3 |
where ED is the effective dose in mSv, DLP is the dose length product in Gy cm, and k is the conversion factor. Using this methodology, ED can be estimated from the DLP, which is reported by most CT systems. The DLP-to-ED conversion factors are shown in Table 2.
Table 2.
Dose length product-to-effective dose conversion factors from NRPB report
| Category (examination) | Conversion factor (mSv/(Gy cm2)) |
|---|---|
| Conventional radiology | |
| Skull and facial bone | 0.028 |
| Head—soft tissue | 0.028 |
| Soft tissues of neck | 0.03 |
| Cervical spine | 0.13 |
| Thoracic spine | 0.19 |
| Lumbar spine | 0.21 |
| Shoulder girdle | 0.036 |
| Elbow | 0.01 |
| Forearm, wrist, and hand | 0.01 |
| Pelvis | 0.29 |
| Hip | 0.175 |
| Knee, lower leg, ankle, and foot | 0.01 |
| Chest | 0.12 |
| Mammography | 0.1 |
| Abdomen | 0.26 |
For five PET-CT systems, the CT radiation dose information was acquired. Two PET-CT systems used DICOM dose SRs, and the remainder acquired the DLP information using the MPPS and OCR from the CT image.
Acquisition of Angiography and Fluorography Equipment Information
This system acquired the exposure dose information for 11 angiography systems. For 10 of these systems, the radiation dose information was acquired from DICOM MPPS and was saved in the database. Initially, one angiography system that was unable to acquire any dose information was excluded; however, it was later replaced by new equipment and eventually provided the additional radiation dose in MPPS form. The DICOM MPPS messages included irradiation information. We developed the DICOM MPPS conversion using a commercial tool (Leadtools, LEAD Technologies, USA). Only three of the six fluorography systems were able to transfer dose information in the form of MPPS and DICOM tag information. In the three remaining fluorography systems, the mean dose values were calculated every 3 months by systems that could extract the dose information from the MPPS and DICOM tags. The calculated mean dose values were matched to the prescribed order at the OCS. To improve the accuracy of the dose information, every 3 months, the mean dose values were recalculated and archived.
To classify each modality, the examination room information from the PACS database and the dose information from each modality were matched to the independent field in the database. If a new device is added, it can be modified in the system’s administrator mode.
In Korea, most hospitals do not use radiological information systems (RISs). A number of institutions have introduced order communication systems (OCSs); however, these are only used in Korea, preventing the commonly established quality assurance (QA) and quality control (QC) systems from being utilized. Additionally, the existing radiation dose monitoring system calculates the entrance surface dose (ESD); however, in this study, the DAP values were used to eliminate error caused by the size of the patient, facilitating the control of dose information fluctuation in the output of the device. Moreover, to facilitate comprehension by medical staff, the dose value is displayed as the effective dose using the conversion factor from ICRP Pub. 103 [15, 16]. From January 1, 2013 to December 31, 2014, this system was used to collect examination data corresponding to each modality (Table 3).
Table 3.
Number of examinations by modality
| Modality | Exam number of 2013 | Exam number of 2014 | Total exam number |
|---|---|---|---|
| Digital radiography | 810,809 | 711,585 | 1,522,394 |
| Computed tomography | 150,371 | 154,084 | 304,455 |
| Angiography | 10,057 | 10,308 | 20,365 |
| Mammography | 16,685 | 15,894 | 32,579 |
| Fluorography | 16,116 | 8866 | 24,982 |
| Positron emission tomography-computed tomography | 14,784 | 15,489 | 30,273 |
This study complied with the Health Insurance and Portability and Accountability Act and was approved by our respective institutional review boards; the need for informed consent was waived.
Results
This study proposed an automatic, real-time patient medical radiation dose management system for all modalities that can be developed and applied in a clinical environment.
The radiation dose information collected from the CT, DR, XA, mammography, and RF modalities was sent to the dose monitoring system and saved. This system recorded the examination history of the patient and dose information from each exam. For the DR, XA, and RF modalities, DAP and ED were given by the system. Similarly, the organ dose was given for the mammography modality, and both the DLP and ED were given for the CT and PET-CT modalities. The workflow of the developed system is shown in Fig. 2.
Fig. 2.
Workflow of dose monitoring system. CR computed radiography, DR digital radiography, MG mammography, RF radio fluoroscopy, CT computed tomography, XA angiography, MPPS modality performed procedure step, OCS order communication system)
The radiation exposure information generated by modalities is included in and categorized by the dose report image, DICOM MPPS, and dose SR. The information in the dose report image is extracted using the OCR method and stored in the dose monitoring system. The data extracted using the OCR method is mapped using the order entry information from HIS to be identified. The dosage information that is included in the DICOM dose SR and MPPS is directly transferred to the dose monitoring system. The stored radiation exposure information can be called by the EMR system and can be displayed using a specially designed dose information screen to provide the individual patient’s exposure information.
In the system viewer, different displays were presented for each patient, equipment setup, examination room, and examination name, and a diagnostic reference level (DRL) display was organized to set the DRL. In the analysis display, the graphs for analyzing each patient, equipment setup, operator, and examination are presented.
The dose view was designed to enable communication at any time in the hospital and simultaneous display of the dose information graphs for each viewer. On the patient display, the dose information for all examinations of that patient are shown; the total DAP, DLP, cumulative dose, and the dose information from each modality may be represented, depending on the chosen term.
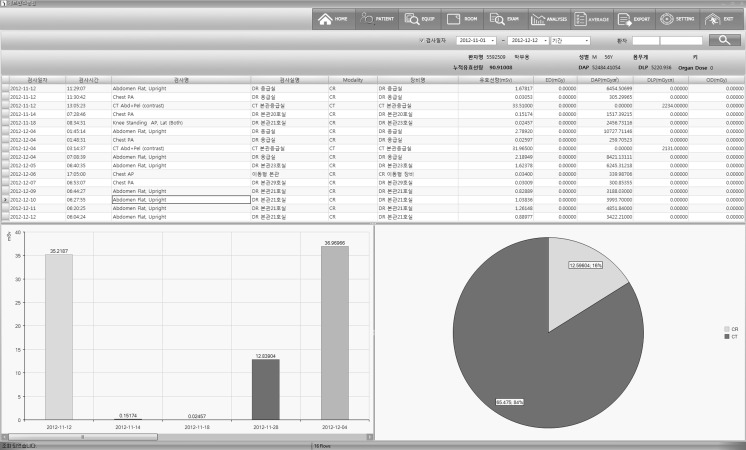
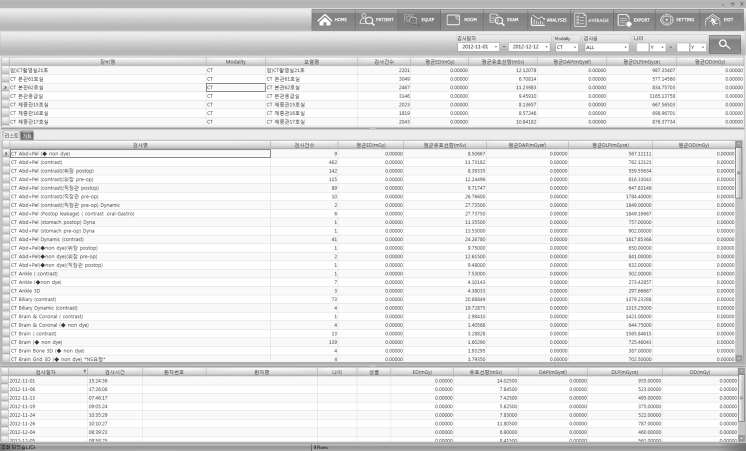
The dose information display is shown in Figs. 3 and 4. In the modality display, the mean dose information from each modality and the equipment utilized for the examination are shown; thus, one can confirm all dose information for each examination. The next step of each examination is determined by monitoring the information from every patient who had the examination.
Fig. 3.
Screenshot of patient radiation dose display (generated for each patient). (The first section displays the exam date and time, exam name, room number, modality, equipment name, effective dose, and DAP for X-ray and fluorography exams; DLP for CT; and mean organ dose for mammography. The left graph displays the effective dose for each date. The right graph displays the effective dose for each modality)
Fig. 4.
Screen shot of radiation dose display by equipment type. (The first section displays the equipment name, modality, room number, exam number, effective dose, and mean DAP for X-ray and fluorography exams; mean DLP for CT; and mean organ dose for mammography. The second section displays the exam name, exam number, mean effective dose, mean DLP, and mean organ dose for each exam. The third section displays the exam date; patient ID, name, age, and sex; effective dose; DAP; DLP; and organ dose for each patient.)
In the analysis display, the radiation dose statistics, sorted by patient age, are provided; patients who exceeded the DRL set previously are also shown. In addition, the dose information for each type of equipment is indicated by the graphical tool for equipment QC.
Discussion
Previous dose monitoring systems were only able to save and manage the dose information for modalities under the regulations of DICOM dose SRs; they only indicated DAP information using conventional methods such as the DICOM MPPS or DICOM header [17].
The radiation exposure monitoring profile from the IHE advised the tracking of patient radiation doses using DICOM dose SR [5]. However, most modality systems do not yet output radiation dose information in DICOM dose SR form. The standards of IEC60601-1-3 advise the installation of devices that show patient doses. However, the majority of diagnostic radiation equipment established before this standard was applied is not equipped with such dose displays.
The radiation exposure of non-DICOM modalities could be managed using the extra modules suggested in this study. The developed information system is designed to support analyzing the data in one system not only for an individual patient but also for different modalities, radiography rooms, and exams. This advantage can easily support physicians from the stage of order entry using the radiation exposure data. This information can be considered ancillary information to clinical decision support for radiation imaging exams.
Based on the findings of the Conference of Radiation Control Directors, all hospitals are advised to monitorpatient doses with the best possible tools, even though no monitoring system can perfectly manage these doses. Therefore, the proposed dose monitoring system is applicable to equipment without DAP meters. The system provides data that can be used by experts, such as medical physicists, to consolidate dose data from various imaging modalities, convert the data into effective doses, and provide the effective dose information to radiologists and clinicians. This system makes it possible to observe patient doses in real time by utilizing the hospital computing system, thus aiding clinical doctors in choosing the proper examinations for patients, acting as a clinical decision support system, and, in the end, reducing patient radiation exposure.
The limitation of this system is that acquiring dose information for PET-CT is confined to CT dose information. We will develop new features for internal radiation exposure estimation by examining radioactivity in PET-CT examinations.
Conclusion
Medical devices that use medical radiation are tested for quality control and optimization of radiation level. To maximize the optimization of radiation tests, continuous monitoring of radiation exposure and quality management must be performed. To achieve these goals, IHE and DICOM committees have defined standards for radiation exposure monitoring. However, for medical devices that were manufactured before the application of these standards, further efforts by individual hospitals (and this study) suggest the development of a model for controlling the radiation exposures for those legacy medical devices. This study could contribute to minimizing the radiation exposure of patients, via the decision support system for medical radiology examination.
References
- 1.Kim YH, Choi JH, Kim CK, Kim JM, Kim SS, Oh YW, Lee CY, Kang DH, Lee YB, Cho PK, Kim HC. Patient dose measurements in diagnostic radiology procedures in Korea. Radiat Prot Dosim. 2007;123(4):540–545. doi: 10.1093/rpd/ncl501. [DOI] [PubMed] [Google Scholar]
- 2.International Commission on Radiological Protection. Managing patient dose in digital radiology, ICRP Publication 93. Ann. ICRP 34, 1–74, 2004 [DOI] [PubMed]
- 3.Vano E, Fernandez JM, Ten JI, Gonzalez L, Guibelalde E, Prieto C. Patient dosimetry and image quality in digital radiology from online audit of the X-ray system. Radiat Prot Dosim. 2005;117(1–3):199–203. doi: 10.1093/rpd/nci716. [DOI] [PubMed] [Google Scholar]
- 4.Ng CK, Sun Z. Development of an online automatic diagnostic reference levels management system for digital radiography: a pilot experience. Comput Methods Prog Biomed. 2011;103:145–150. doi: 10.1016/j.cmpb.2010.07.008. [DOI] [PubMed] [Google Scholar]
- 5.Integrating the Healthcare Enterprise IHE Radiology Technical Framework Radiation Exposure Monitoring (REM) Integration Profile. http://www.ihenet/Technical_Framework/upload/IHE_RAD_TF_Sup_Radiation_Exposure_Monitoring_Public_Comment_2008_02_29.pdf. Accessed 10 June 2014
- 6.United Nations Scientific Committee on the Effects of Atomic Radiation. UNSCEAR 2008 Report. Vol. I sources of ionizing radiation Annex A: Medical radiation exposures, 2010
- 7.Rehani M, Frush D. Patient exposure tracking: The IAEA smart card project. Radiat Prot Dosim. 2011;147(1–2):314–316. doi: 10.1093/rpd/ncr300. [DOI] [PubMed] [Google Scholar]
- 8.Sodickson A, Baeyens PF, Andriole KP, Prevedello LM, Nawfel RD, Hanson R, Khorasani RK. Recurrent CT, cumulative radiation exposure, associated radiation-induced cancer risks from CT of adults. Radiology. 2009;251(1):175–184. doi: 10.1148/radiol.2511081296. [DOI] [PubMed] [Google Scholar]
- 9.Vano E, Fernandez JM, Ten JI, Guibelalde E, Gonzalez L, Pedrosa CS. A real-time measurement and audit of radiation dose to patients undergoing computed radiography. Radiology. 2002;2251:283–288. doi: 10.1148/radiol.2243011331. [DOI] [PubMed] [Google Scholar]
- 10.Bongartz G, Golding S, Jurik A, Leonardi M, van Meerten EP, Geleijns J, Jessen KA, Panzer W, Shrimpton PC, Tosi G: European Guidelines for Multislice Computed Tomography. European Commission, 2004
- 11.Shrimpton PC, Hillier MC, Lewis MA, Dunn M. National survey of doses from CT in the UK: 2003. Br J Radiol. 2006;79:968–980. doi: 10.1259/bjr/93277434. [DOI] [PubMed] [Google Scholar]
- 12.Noumeir R. Benefits of the DICOM modality performed procedure step. J Digit Imaging. 2005;118(4):260–269. doi: 10.1007/s10278-005-6702-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Noumeir R. Benefits of the DICOM structured report. J Digit Imaging. 2006;119(4):295–306. doi: 10.1007/s10278-006-0631-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McCollough C, Cody D, Edyvean S, Geise R, Gould B, Keat N, Huda W, Judy P, Kalender W, McNitt-Gray M, et al. The Measurement, Reporting, Management of Radiation Dose in CT. Rep AAPM Task Group. 2008;23:1–28. [Google Scholar]
- 15.Charnock P, Moores BM, Wilde R. Establishing local and regional DRLs by means of electronic radiographical X-ray examination records. Radiat Prot Dosim. 2013;157(1):62–75. doi: 10.1093/rpd/nct125. [DOI] [PubMed] [Google Scholar]
- 16.Moores BM, Charnock P, Ward M. Web-based tools for quality assurance and radiation protection in diagnostic radiology. Radiat Prot Dosim. 2010;139(1–3):422–429. doi: 10.1093/rpd/ncq004. [DOI] [PubMed] [Google Scholar]
- 17.Cook TS, Zimmerman SL, Steingall SR, Maidment ADA, Kim WJ, Boonn WW. RADIANCE: an automated, enterprise-wide solution for archiving and reporting CT radiation dose estimates. Radiographics. 2011;31:1833–1846. doi: 10.1148/rg.317115048. [DOI] [PubMed] [Google Scholar]
- 18.Edmonds I. R: calculation of patient skin dose from diagnostic X-ray procedures. Br J Radiol. 1984;57:733–734. doi: 10.1259/0007-1285-57-680-733. [DOI] [PubMed] [Google Scholar]