Abstract
Family systems therapy has shown to be a powerful adjunct to substance use treatment for couples and for adolescent substance users (Rowe, 2012). However, studies including children (8–16 years) in the treatment of their substance using mothers have been overlooked and are essentially non-existent. Addressing the quality of the mother-child relationship and communication through family systems therapy may prove to be a potent intervention focus for improving mothers’ substance use outcomes and parent-child interaction. As such, the current study recruited 183 mothers who sought outpatient treatment through a local substance use treatment facility and randomly assigned them to also receive family systems therapy or Women’s Health Education. Self-report and observational data were collected, and assessment interviews were completed at baseline, 3, 6, 12 and 18 months post-baseline. Findings showed that women assigned to family systems therapy showed a quicker decline in alcohol, marijuana and cocaine use, supporting the efficacy of family therapy as an important addition to mother’s substance use treatment plans. Data also revealed an association between change in observed autonomy-relatedness and substance use, though mediation was not found. To our knowledge this is the first effort to successfully document a family systems therapy for substance using mothers with minor children in their care.
Keywords: Substance use, mothers, family systems therapy
A limited number of studies evaluate treatments designed for women substance users (Tuchman, 2010). Given that women substance users have unique characteristics, often including responsibility for minor children, a focus on treatments designed for women is needed to improve treatment effectiveness. Women report more histories of physical or sexual abuse, more adverse psychological consequences and less social support than male substance users (Niccols et al., 2012). In addition, an estimated 12% of children under the age of 18 years live with a parent with an alcohol or other substance use disorder (HHS, Substance Abuse and Mental Health Services Administration (SAMHSA), Office of Applied Studies, 2009). Among those children, 70% are raised by single mothers with substance use problems (Lussier, Laventure, & Bertrand, 2010).
Substance use is considered a stressor that negatively impacts the parenting of mothers (Lussier et al., 2010) as well as relapse (Denton et al., 2014). Further, the parent-child relationship is often characterized by inconsistent care, unstable attachment and inadequate response to children’s needs (Lussier et al., 2010). When mothers seek substance use treatment, programming generally excludes their children even though including children in the treatment process of their mothers has the potential to positively impact mothers’ substance use outcomes, as well as parent-child interaction. That is, qualitative (Sword et al., 2009) as well as quantitative (Milligan et al., 2010) research shows that children provide a motivating presence in their mother’s substance use treatment that can sustain women’s recovery (Sword et al., 2009).
Many researchers have stressed the importance of involving family members in the treatment of substance users, as it can have a positive impact on relapse, client engagement, and psychiatric functioning (Rowe, 2012). From a family systems perspective, risk behaviors, such as substance use, are best understood when examining family interaction. For example, stressful parent-child interactions (Pelham et al., 1997), family discord (Denton et al., 2014) and living with a partner with a substance use disorder (Denton et al., 2014) have been associated with increased substance use among mothers. Given that parental and interpersonal stress have been associated with a greater risk of relapse, treatment recommendations have included targeting interpersonal stress to help maintain abstinence (Denton et al., 2014). Therefore, addressing potential stressful parent-child interactions through family therapy has high potential to lead to better long-term substance use outcomes for women with children in their care. While the literature reports positive outcomes of family therapy with adolescent substance users and couples (Fletcher, 2013; Rowe, 2012), it is somewhat surprising that no family therapy trials were identified in the literature that include children in the treatment of their substance using mothers.
Although it is important to know which treatment interventions are most effective for substance users, understanding factors associated with change in substance use can enhance the treatment effectiveness through directing therapists to potent intervention targets. Interpersonal factors have been identified as better predictors of substance use than intrapersonal factors (Kalyva & Melonashi, 2014). Many family systems therapies share an underlying belief that changing family interaction through improved communication and connection to underlying love and care results in new and improved interaction patterns, as well as reduced alcohol and drug use (Rowe, 2012). That is, theoretically, changes in family interaction are expected to mediate the relationship between family therapy and substance use. In particular, autonomy and relatedness have been identified as factors predictive of functional family interactions (Friedman et al., 2009; Murray et al., 2015) and recently, has received a great deal of research attention (Murray et al., 2015).
Autonomy refers to independent thinking and self-determination in social interactions while relatedness refers to the ability to maintain close and supportive relationships (Allen, Hauser, Bell, & O’Connor, 1994). Interpersonal behaviors that promote autonomy and relatedness are associated with positive psychosocial outcomes, while behaviors that undermine autonomy or relatedness are associated with poorer outcomes. Behaviors associated with undermining autonomy and relatedness include high levels of psychological control, criticism, stifling individuality, encouraging dependence and manipulation, whereas behaviors encouraging autonomy and relatedness include acceptance, approval, affection and emotional support.
Research is limited in that examinations of change in interaction associated with family therapy are often based on self-report questionnaires, single informant and cross-sectional approaches (Holmbeck et al., 2003). Observational methods that include coding of parent-child conversation over time can reduce bias and offer rich information on communication interactions. Research shows that higher observed undermining relatedness predicts increased alcohol use in emerging adults (Murray et al., 2015), however, the role of autonomy-relatedness on maternal substance use has not been investigated.
Current Study
The current study used a longitudinal, randomized design to examine the impact of family systems therapy, compared to a non-family therapy, among women seeking substance use treatment through a large community treatment program. Some assert that substance use treatment that does not address the full range of women’s needs, including parenting skills and overall emotional health, will fail and lead to higher relapse (Center for Substance Abuse Treatment, 2009). In this study, it was expected that women who received family therapy with their children would report better substance use outcomes than women who did not receive family therapy. It was further hypothesized that changes in mother-child interaction, specifically, observed autonomy-relatedness, would mediate substance use outcomes. Several factors have been shown to influence change in substance use, including history of childhood sexual and physical abuse (Greenfield et al., 2007), motivation to change (Miller & Rollnick, 2012) and living with a substance using partner (Denton et al., 2014). Further, child’s age and sex (Chaplin & Aldao, 2013), as well as mother’s history of childhood maltreatment (Enlow, Englund, & Egeland, 2016), can influence mother-child interaction. Therefore, these variables were controlled in the current study.
Method
Participants
Participants included N =183 substance use disordered mothers with at least one biological child in their care. Mothers were recruited from a community treatment center for substance use disorders in a large Midwestern city. To be eligible for the study, mothers had to (1) be seeking outpatient treatment for their substance use disorder, (2) meet diagnostic criteria for an alcohol or drug use disorder as defined by DSM IV, and (3) have a child between the age of 8 – 16 years who either resided with the participating mothers at least 50% of the time in the past 2 years or 100% of the time in the past 6 months (to ensure that the mother and child have had time to develop relational patterns and expectations that can be addressed and modified). If more than one eligible child was identified, the child reporting substance use or other problem behaviors was selected as the target child. Given the need for consistency, and to reduce confounding interaction patterns associated with different children, the target child participated in each of the observational tasks with the mother over time.
Mothers ranged in age from 22 to 54 years (M=33.9), were primarily white, non-Hispanic (53.6%) or African-American (42.6%). Only 19.1% of the women reported that they were married, and the majority of mothers (85%) had a high school degree or less. In addition, 60% of families had an annual income of $15,000 or below and only about 18% of families had an annual income greater than $30,000. Mothers reported having between 1 to 11 children (M = 3.21). The target child’s ages ranged from 8 to 16 (M = 11.54), with 51.9% male. See Table 1 for demographic characteristics.
Table 1.
Demographic Characteristics of the Current Sample
| Variable | n (%) | M | SD |
|---|---|---|---|
| Mothers | |||
| Race/ethnicity | |||
| White, not of Hispanic Origin | 98(53.6) | ||
| African American | 78(42.6) | ||
| Other | 7(3.8) | ||
| Marital status | |||
| Single, never married | 60(32.8) | ||
| In a romantic relationship | 64(34.9) | ||
| Legally married | 20(10.9) | ||
| Separated but still married | 15(8.2) | ||
| Divorced | 21(11.5) | ||
| Widowed | 3(1.6) | ||
| Annual family income | |||
| 0–$5,000 | 49(26.8) | ||
| $5,001–$15,000 | 61(33.3) | ||
| $15,001–$30,000 | 39(21.3) | ||
| $30,001–$45,000 | 16(8.7) | ||
| $45,001–$60,000 | 7(3.8) | ||
| $60,001–$75,000 | 6(3.3) | ||
| $75,001 or above | 4(2.2) | ||
| Employment status | |||
| Work 40+hours a week | 22(12.0) | ||
| Work fewer than 40 hours a week | 22(12.0) | ||
| Homemaker | 10(5.5) | ||
| Unemployed | 105(57.4) | ||
| Student | 19(10.4) | ||
| Others | 3(1.6) | ||
| Children | |||
| Gender | |||
| Male | 95(51.9) | ||
| Currently enrolled | 179(97.8) | ||
| GPA | 2.87 | .70 | |
| Children have ever been | |||
| Placed in a foster home | 20(10.9) | ||
| Placed in a group home | 7(3.8) | ||
| Kept in juvenile detention | 13(7.1) | ||
| Kept in jail overnight | 7(3.8) | ||
| A ward of the state | 8(4.4) | ||
Procedure
Mothers were screened for eligibility and interest in the research through the community treatment center. After obtaining parental permission from eligible mothers, research assistants contacted the target child and informed him or her of the research study. If more than one eligible child was identified, only the child with more severe substance use, as reported on the Form 90 (Miller, 1996), or a higher problem behavior score as measured on the Youth Self Report (Achenbach & Edelbrock, 1982) was included as the target child. All children, mothers’ romantic partners and other caregivers in the home were invited to participate in the family systems therapy sessions. In particular, 36% of all families included more than one child in the therapy sessions, 9% included the mother’s romantic partner and 10% included another family member.
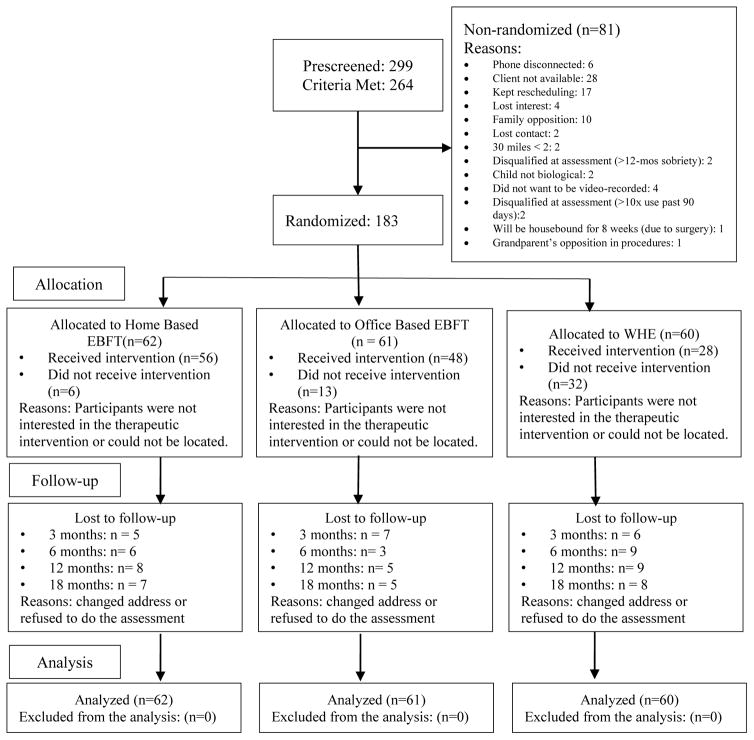
At baseline, both the mother and target child completed an assessment battery including several individual and family measures, a semi-structured substance use assessment, as well as a video-recorded mother-child interaction task. All families were then randomly assigned to one of the two intervention conditions: (1) Office- or home- based family systems therapy, n = 123, or (2) Women’s Health Education (WHE, mothers only), n = 60. Because of concerns that therapy location, office versus home-based, could impact substance use outcomes, the context of intervention on outcomes was examined. WHE, as a comparison condition, did not include other family members or family therapy techniques, but has been shown to result in positive substance use outcomes among substance using women (Hien et al., 2010). The substance use treatment facility offered individual counseling, one hour per week, and group counseling, one to three hours per week. The general counseling model is based on the Community Reinforcement Approach (CRA) but also encourages 12-Step recovery program involvement (Brigham, 2003). Sessions were offered weekly and had to be completed within six months post-baseline. See Figure 1 for intervention design and flow of participants.
Figure 1.
CONSORT flowchart. EBFT = Ecologically-Based Family Therapy; WHE= Women’s Health Education.
Assessment procedures for all research participants were identical. Participating families in the two conditions were assessed at 3 and 6, 12 and 18- months post-baseline, and the video-recorded mother-child interaction task was administered at baseline, 6 and 18-months post-baseline. The Ohio State University Institutional Review Board approved all study procedures. Participating mothers were offered a $75 gift card while children were offered a $40 gift card at completion of the baseline assessment and each follow-up assessment.
Treatment Intervention
Ecologically-Based Family Therapy (EBFT) is a 12-session family systems therapy that targets specific dysfunctional interactions linked to the development of problem behaviors. Based on a social ecological theoretical perspective (Bronfenbrenner, 1979), EBFT is a family systems therapy which recognizes that substance use and related individual and family problems are nested in multiple interrelated systems, and therefore, targets dysfunctional family interactions associated with the development and continuation of problem behaviors. The treatment sessions focus on guiding families to consider their current problems and solutions through techniques such as reframing and interpretations, interrupting problem behaviors through communication and problem-solving skills training, and assisting families in obtaining services such as medical care, job trainings, or self-help programs. Originally developed for substance using runaway adolescents and their families, (Slesnick, Guo, Brakenhoff, & Bantchevska, 2015; Slesnick & Prestopnik, 2005, 2009), the intervention has been rated as a promising evidence-based practice by the National Institute of Justice and as a supported evidence-based practice by the California Evidence-Based Clearinghouse. Even though EBFT has been effective for families with a substance using adolescent runaway, the effectiveness of EBFT for mothers seeking substance use treatment and their children has not been tested.
EBFT focuses on improving social interactions, emotional connectedness and problem resolution skills among family members. Specifically, the first 1–2 sessions aim to engage family members into the treatment, assess individual and family needs, strengths and weaknesses, and guide families towards considering current problems and potential solutions as residing in the family relationship. Sessions 3 – 12 target helping families identify and address aspects of the family relationship that contribute to the development and maintenance of parents’ substance use as well as aspects of the family relationship that serve a protective function. New problem-solving skills are taught and practiced. Family cohesion and individuals’ competence to appropriately communicate needs for change are facilitated. Discussion about mothers’ substance use and plans for how children can support mothers’ efforts towards sobriety unfolds over the course of the treatment, depending upon the parents’ willingness and tolerance. Cognitive-behavioral skills training is also done and is aimed at changing individuals’ symptom-related thoughts, communication and coping skills, and emotional reactions.
EBFT therapists were licensed counselors or clinical graduate students who received multi-step training including video and manual review, role play exercises, and discussion of the theoretical rationale and practical application of EBFT techniques. Ongoing supervision and independent treatment fidelity coding were employed to assure implementation quality and adherence to the intervention protocol.
Among the 123 families receiving EBFT, 61 families received the treatment in the office and 62 families received the treatment at home. Independent t-tests were performed to compare the group difference on mothers’ drug use (i.e., alcohol, marijuana, cocaine, and opioid) between office- and home-based EBFT groups across all five time points. No significant differences were found. Thus, the two groups were combined into one EBFT group.
Women’s Health Education (WHE) is a 12-session manualized educational intervention used as an attention control (Miller, Pagan, & Tross, 1998). N = 60 mothers were assigned to WHE which focused on helping mothers understand the woman’s body, human sexual behavior, pregnancy and childbirth, STD’s, HIV, and AIDS. WHE provided equivalent therapist attention and expectancy of benefits, but did not include family systems therapy techniques, and children were not engaged in the therapy. WHE has shown effectiveness in other research for reducing posttraumatic stress disorder symptoms among women in treatment for substance use disorders (Hien et al., 2009).
Measures
Mothers’ substance use was measured by the Form-90 (Miller, 1996), a structured interview that uses a timeline follow-back approach to assess daily substance use for the past 90 days. This measure has high test-retest reliability with kappas for different drug classes ranging from .74 to .95 (Tonigan, Miller, & Brown, 1997; Westerberg, Tonigan, & Miller, 1998). In the current study, the percentage of mothers’ total days of alcohol, marijuana, cocaine, and opioids use in the prior 90 days was assessed at baseline, 3-, 6-, 12- and 18 months post-baseline.
Mother-Child Interactions
Both the mother and child participated in a 10-minute interaction task at baseline, 6- and 18- month post-baselines. Mother-child relationship quality was assessed using an observational mother-child interaction task. First, mother and child independently rated 34 questions on the Areas of Change Questionnaire using a 7-point scale (ACQ; Margolin, Talovic, & Weinstien, 1983) addressing specific behaviors parents and children would like to change in their relationship. The item(s) in which parents and children most disagreed was identified as the discussion topic, and mother and child were asked to engage in a 10-minute discussion on the topic with the goal to work towards a resolution.
The 10-minute interaction was video-recorded and coded using the Autonomy and Relatedness coding system (Allen et al., 2000) on 10 behavioral categories. These behavioral categories were further grouped into four dimensions depending on whether the behavior promoted or undermined autonomy or relatedness (Allen, Porter, McFarland, McElhaney, & Marsh, 2007). Specifically, Autonomy Promoting behaviors included justifying one’s position with reasons, and demonstrating confidence in speaking to the other person. Relatedness Promoting behaviors included queries with a genuine interest in the other person’s thoughts, validating/agreeing/positively reacting to the other person, and high engagement in communication, and displaying empathy to the other person. Autonomy and relatedness promoting behaviors are examined as one single construct (Allen et al., 1994; Oudekerk, Allen, Hessel, & Molloy, 2015). Undermining Autonomy behaviors included recanting the other person’s statement, blurring the boundary between the other person and his/her position, and pressuring the other person to agree. Undermining Relatedness behaviors included interrupting or ignoring the other person, and using hostile/devaluing statements towards the other person. Mother’s interactive behaviors and child’s interactive behaviors were coded separately, generating eight relationship indices. In addition, the mothers’ behaviors and the children’s behaviors were averaged on each dimension, yielding an additional four indices reflecting the relationship quality at the dyadic level. Twenty percent of the observations were double-coded. Inter-rater reliability for the double-coded recordings was ICC = 0.86 on average, with the rater reliability good-to-excellent at baseline (ICC = .84), 6 months post-baseline (ICC = 0.87), and 18 months post-baseline (ICC = 0.89).
Baseline Demographic Characteristics
Mothers’ childhood abuse history (physical and sexual abuse) (0 as no, 1 as yes), motivation for change (both alcohol and drugs), and partner drug use (0 as no, 1 as yes) were controlled when examining the change trajectory of mothers’ substance use given that research shows that these variables are associated with individual’s drug use (DiClemente, 1999). Child’s age (0 as 8 to 12 years old, 1 as 13 to 16 years old) and substance use (the percentage of any substance use in the prior 90 days) were also controlled because research shows that child’s age and deviant behaviors are associated with parent-child interactions and subsequently, are likely to influence parental substance use (Chaplin & Aldao, 2013; Pelham et al., 1997). Motivation for change was evaluated using the Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES; Miller & Marlatt, 1984). The SOCRATES includes three subscales: Readiness, Ambivalence, and Taking Steps (Isenhart, 1994; Miller & Tonigan, 1996). Test-retest correlations for subscales range from .83 to .99 (ICC = .82 – .94). In the present study, the Cronbach alpha level for the three subscales ranged from .77 to .95 for drug use, and .88 to .97 for alcohol use. Children’s age, sex and mothers’ child abuse history were controlled when analyzing the change trajectory of mothers’ and children’s interaction behaviors because these variables have been shown to influence parent-child interactions (Chaplin & Aldao, 2013; Enlow, Englund, & Egeland, 2016).
Overview of Analyses
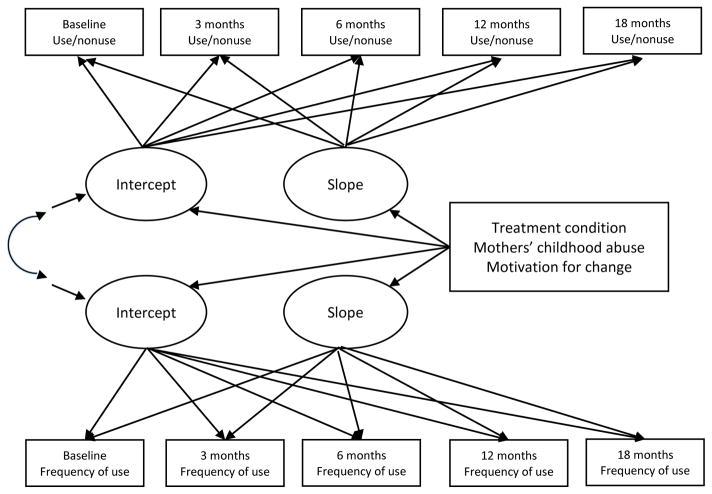
This study used an intent-to-treat design which consisted of the entire sample of 183 mothers. Data were analyzed in three steps. First, a series of two-part latent growth models (LGM) were performed to examine the change trajectory of mothers’ alcohol, marijuana, cocaine, and opioid use respectively (Muthén, 2002; Olens & Schafer, 2001). The percentage of mothers’ total days of alcohol, marijuana, cocaine, and opioid use in the prior 90 days included a preponderance of zeros across five time points. As a result, the data were highly skewed. By using the two-part model strategy, the original distribution of substance use was split into two parts, each modeled by separate, but correlated growth functions (Figure 2). In Part 1 of the model, a binary variable was created to distinguish between use (coded as 1) versus nonuse (coded as 0). Substance use (i.e., use versus nonuse) was modeled as a random-effects logistic growth model. Part 2 of the model examined the growth trajectory of frequency for non-zero substance use. The frequency of substance use was modeled as a traditional LGM. Treatment condition and background variables including partner drug use, mothers’ childhood abuse history, and motivation for change in alcohol and drug use were added to the model as covariates. Partner drug use was added to Level-1 of the model as a time-varying covariate. All other time-invariant variables including mothers’ child abuse history and motivation (e.g., readiness) for change at baseline were added to Level-2.
Figure 2.
Two-part latent growth model.
Second, a series of latent growth models (LGM) were tested to examine the change trajectory of mothers’ and children’s autonomy and relatedness promoting behaviors, autonomy undermining behaviors, and relatedness undermining behaviors. Treatment status and background variables including child’s gender and sex, and mothers’ childhood abuse history, were added to level 2 of the model as time-invariant covariates. In the third step, the mediating effects of mothers’ and children’s autonomy and relatedness behaviors were tested. The growth trajectories of mothers’ and children’s autonomy and relatedness behaviors (i.e., mediators) and mothers’ drug use were modelled as distinct parallel processes and treatment condition was included in the model as the independent variable (Cheong, MacKinnon, & Khoo, 2003).
Results
The follow-up completion rate across the four time points (3, 6, 12, and 18 months) ranged from 88% to 90%. No cases had missing data across all time points, therefore, all cases (n=183) were included in the analyses. Full information maximum likelihood in the Mplus software (Muthén & Muthén, 2012) was used to estimate missing data when performing the analyses. Table 2 presents the means and standard deviations for mothers’ substance use, and mothers’ and children’s autonomy and relatedness behaviors.
Table 2.
Means and Standard Deviations of Study Variables
| Variables | n | M | SD |
|---|---|---|---|
| % Days of alcohol use | |||
| Baseline | 183 | 21.24 | 29.64 |
| 3 months | 165 | 13.92 | 25.36 |
| 6 months | 165 | 11.73 | 22.08 |
| 12 months | 161 | 12.40 | 24.73 |
| 18 months | 163 | 11.11 | 22.62 |
| % Days of marijuana use | |||
| Baseline | 183 | 28.01 | 38.65 |
| 3 months | 165 | 19.17 | 34.09 |
| 6 months | 165 | 20.96 | 36.72 |
| 12 months | 161 | 17.18 | 33.62 |
| 18 months | 163 | 21.29 | 36.40 |
| % Days of cocaine use | |||
| Baseline | 183 | 9.59 | 21.95 |
| 3 months | 165 | 4.55 | 15.42 |
| 6 months | 165 | 4.46 | 16.05 |
| 12 months | 161 | 4.37 | 15.00 |
| 18 months | 163 | 4.24 | 16.23 |
| % Days of opioid use | |||
| Baseline | 183 | 33.09 | 41.15 |
| 3 months | 165 | 13.16 | 28.82 |
| 6 months | 165 | 13.85 | 31.31 |
| 12 months | 161 | 11.32 | 27.78 |
| 18 months | 163 | 14.33 | 32.08 |
| Mothers’ autonomy and relatedness promoting behaviors | |||
| Baseline | 181 | 6.93 | 2.19 |
| 6 months | 118 | 7.26 | 2.43 |
| 18 months | 111 | 7.06 | 2.23 |
| Mothers’ undermining autonomy behaviors | |||
| Baseline | 181 | 2.11 | 1.53 |
| 6 months | 118 | 1.94 | 1.56 |
| 18 months | 111 | 1.58 | 1.58 |
| Mothers’ undermining relatedness behaviors | |||
| Baseline | 181 | .92 | 1.07 |
| 6 months | 118 | 87 | 1.13 |
| 18 months | 111 | .50 | .77 |
| Children’s autonomy and relatedness promoting behaviors | |||
| Baseline | 181 | 4.06 | 2.58 |
| 6 months | 118 | 4.49 | 2.78 |
| 8 months | 111 | 4.13 | 2.55 |
| Children’s undermining autonomy behaviors | |||
| Baseline | 181 | 1.51 | 1.40 |
| 6 months | 118 | 1.14 | 1.31 |
| 18 months | 111 | .99 | 1.13 |
| Mothers’ undermining relatedness behaviors | |||
| Baseline | 181 | 1.13 | 1.33 |
| 6 months | 118 | 1.09 | 1.09 |
| 18 months | 111 | .79 | 1.03 |
Substance use
Table 3 presents information on the covariates. The majority of mothers reported the experience of physical abuse (62.8%), and 48.6% of the mothers reported sexual abuse. Also, at baseline, 32.3% of women reported that their romantic partner had substance use problems. Table 4 presents the treatment effects and also the effects of covariates on mothers’ alcohol, marijuana, cocaine, and opioid use.
Table 3.
Descriptive Statistics of Level-1 and -2 Covariates
| Variable | M | SD | Range |
|---|---|---|---|
| Level-1 | |||
| Partner drug use | |||
| baseline | 32.3% | - | - |
| 3 months | 9.8% | - | - |
| 6 months | 8.7% | - | - |
| 12 months | 9.8% | - | - |
| 18 months | 7.7% | - | - |
| Level-2 | |||
| Sexual abuse | 48.6% | - | - |
| Physical abuse | 62.8% | - | - |
| Ambivalence – alcohol | 9.40 | 5.10 | 4–20 |
| Recognition – alcohol | 17.43 | 10.15 | 7–35 |
| Taking steps – alcohol | 24.57 | 11.79 | 8–40 |
| Ambivalence – drug use | 13.48 | 4.70 | 4–20 |
| Recognition – drug use | 27.90 | 8.29 | 7–35 |
| Taking steps – drug use | 31.94 | 8.47 | 8–40 |
| Child’s age | 36.1% | - | - |
| Child’s substance use | 6.44 | 23.49 | 0–100 |
Note. Dashes indicate that data were not available
Table 4.
Fitted Model of Changes for Mothers’ Alcohol, Marijuana, Cocaine, and Opioid Use
| Slope grow factor | ||||||||
|---|---|---|---|---|---|---|---|---|
| Alcohol | Marijuana | Cocaine | Opioid | |||||
|
| ||||||||
| B | SE | B | SE | B | SE | B | SE | |
| Part 1 of the model | ||||||||
| Level 1 covariate | ||||||||
| Partner drug use | .45 | .36 | .10 | .56 | .30 | .47 | 1.06* | .47 |
| Level 2 covariate | ||||||||
| Intervention | .26 | .19 | −.05 | .34 | −.25 | .26 | .50 | .44 |
| Sexual abuse | .26 | .17 | .34 | .36 | −.10 | .26 | .01 | .44 |
| Physical abuse | −.18 | .19 | .52 | .44 | .43 | .33 | .28 | .47 |
| Ambivalence | .00 | .02 | .04 | .05 | .04 | .03 | −.06 | .05 |
| Readiness | .01 | .01 | −.01 | .03 | −.00 | .03 | .06 | .04 |
| Taking steps | −.01 | .01 | −.07** | .02 | −.04* | .02 | −.01 | .03 |
| Child’s age | .06 | .18 | .32 | .35 | .13 | .30 | −.34 | .47 |
| Child’s substance use | −.01* | .00 | .01 | .01 | −.01* | .01 | .01 | .01 |
| Part 2 of the model | ||||||||
| Level 1 covariate | ||||||||
| Partner drug use | .32 | .20 | −.03 | .22 | .70* | .35 | −.02 | .31 |
| Level 2 covariate | ||||||||
| Intervention | −.23* | .11 | −.23* | .11 | −.49* | 0.21 | −.04 | .16 |
| Sexual abuse | −.27* | .11 | −.30 | .16 | .12 | .20 | −.05 | .17 |
| Physical abuse | .07 | .12 | −.03 | .16 | .41 | .28 | −.15 | .23 |
| Ambivalence | −.01 | .02 | −.01 | .02 | −.04* | .02 | .00 | .02 |
| Recognition | .00 | .01 | .00 | .01 | .01 | .02 | .02 | .02 |
| Taking steps | −.02* | .01 | −.00 | .01 | .00 | .02 | −.01 | .01 |
| Child’s age | .02 | .11 | −.12 | .20 | −.10 | .20 | −.07 | .20 |
| Child’s substance use | .00 | .00 | .00 | .00 | .00 | .00 | 0.00 | .00 |
Note.
p <.05.
p < .01.
Alcohol use
The unconditional model of Parts 1 and 2 with time as the only Level-1 predictors were simultaneously estimated. Mothers showed a decreased likelihood of alcohol use in model Part1 (B= −.24, SE =.07, p < .001) and decreased frequency of alcohol use in model Part 2 (B= −.23, SE =.04, p < .001). The covariance between the intercept growth factor between model Parts 1 and 2 was significant (B=2.56, SE =.41, p < .001), suggesting that mothers with a lower probability to use alcohol showed less frequent alcohol use over time. Other covariance between growth parameters were nonsignificant and subsequently fixed at zero.
The treatment condition and individual variables were added to the model. For Part 2 of the model, the results showed that mothers receiving EBFT exhibited decreased alcohol use at a faster rate (B = −.23, SE =.11, p < .05). Mothers’ sexual abuse experiences and motivation for change (e.g., taking steps) were significant predictors of the time effect. Mothers with a history of childhood sexual abuse exhibited a faster decline of alcohol use (B = −.27, SE =.11, p < .05). Moreover, mothers with higher scores on motivation for change (taking steps) exhibited a faster decline of alcohol use (B = −.02, SE =.01, p < .05). In Part 1 of the model, a high level of child’s substance use was associated with a decreased likelihood of mother’s alcohol use (B = −.01, SE =. 00, p < .05).
Marijuana use
The unconditional model of Parts 1 and 2 with time as the only Level-1 predictor were simultaneously estimated. Mothers showed a decreased likelihood of marijuana use in model Part1 (B= −.35, SE =.10, p < .01) and decreased frequency of marijuana use in model Part 2 (B= −.14, SE =.05, p < .01). The covariance between the intercept growth factor between model Parts 1 and 2 was significant (B=3.80, SE =.70, p < .001), suggesting that mothers with a lower probability to use marijuana showed less frequent marijuana use over time. Other covariance between growth parameters were nonsignificant and subsequently fixed at zero.
The treatment condition and individual variables were added to the model. For Part 2, the results showed that mothers receiving EBFT exhibited decreased marijuana use at a faster rate (B = −.23, SE =.11, p < .05). In Part 1 of the model, mothers’ higher scores on motivation for change (taking steps) was associated with a greater rate of decline in their likelihood of using marijuana (B = −.07, SE =. 02, p < .01).
Cocaine use
The unconditional model of Parts 1 and 2 with time as the only Level-1 predictors were simultaneously estimated. Mothers showed a decreased likelihood of cocaine use in model Part1 (B= −.61, SE =.41, p < .01) and decreased frequency of cocaine use in model Part 2 (B= −.18, SE =.08, p < .05). The covariance between the intercept growth factor between model Parts 1 and 2 was significant (B=1.32, SE =.48, p < .01), suggesting that mothers with a lower probability to use cocaine showed less frequent cocaine use over time. The covariance between the intercept and slope growth factors were fixed to be zero for model convergence. The rest of the covariance between growth parameters were nonsignificant and subsequently fixed at zero.
The treatment condition and individual variables were added to the model. For Part 2, the results showed that treatment had a significant effect on mothers’ cocaine use, with mothers receiving EBFT exhibiting a faster rate of decrease (B = −.49, SE =.21, p <.05). Mothers with higher scores on motivation for change (ambivalence) exhibited a faster decline of cocaine use (B = −.04, SE =.02, p <.05). In Part 1 of the model, mothers’ higher scores on motivation for change (taking steps) was associated with a greater rate of decline in their likelihood of using cocaine (B = −.04, SE =. 02, p < .05). Moreover, higher levels of child’s substance use was associated with a decreased likelihood of mother’s cocaine use (B = −.01, SE =. 01, p < .05).
Opioid use
The unconditional model Parts 1 and 2 with time as the only Level-1 predictor were simultaneously estimated. Mothers showed a decreased likelihood of opioid use in model Part1 (B= −1.43, SE =.28, p < .001) and a decreased frequency of opioid use in model Part 2 (B= −.20, SE =.07, p < .01). None of the covariance between growth parameters were significant and subsequently fixed at zero. No treatment effects were found for opioid use. In Part 1 of the model, partner drug use was significantly associated with increased odds of opioid use among mothers (B= 1.06, SE =.47, p < .05).
Mother-Child Interactions
A series of unconditional models of mothers’ and children’s autonomy and relatedness behaviors were examined, with time as the only Level-1 predictor. Both mothers’ (B=.06, SE =.12, p > .05) and children’s (B=.06, SE =.14, p > .05) autonomy and relatedness promoting behaviors remained stable over time. In contrast, both mothers (B= −.25, SE =.09, p <.01) and children (B=−0.27, SE =.07, p <.001) showed decreased autonomy undermining behaviors. Similarly, both mothers (B= − .19, SE =.06, p <.01) and children (B= −.14, SE =.06, p < .05) showed decreased relatedness undermining behaviors. No treatment effects were found for parent-child interactions. Because treatment conditions were not associated with change trajectories of mothers’ and children’s interaction behaviors, mothers and children’s interaction behaviors did not serve to mediate the relationship between treatment conditions and mothers’ drug use. In order to further explore the association between mothers’ and children’s interaction behaviors and mothers’ drug use, the interaction effects between treatment conditions and mothers’ and children’s interaction behaviors were tested. Given that mothers’ and children’s autonomy and relatedness promoting behaviors remained stable, these variables were not included in the test of interaction effects.
Associations between Mothers’ Substance Use and Mother-Child Interactions
Mothers and children’s interaction behaviors were added to the two-part models of substance use (i.e., alcohol, marijuana, cocaine, and opioid) as time-varying covariates at Level 1 for both Parts 1 and 2. Cross-level interaction terms between interaction behaviors and treatment(interaction behaviors X treatment) were also added at Level 2 of the model. Nonsignificant covariates or interactions were not retained in the final model.
For alcohol use, the effects of mothers’ and children’s undermining autonomy on alcohol use were tested. Neither mothers’ nor children’s undermining autonomy was a significant predictor. The interaction between treatment condition and mothers’ and children’s undermining autonomy was not significant either. In the next step, the effects of mothers’ and children’s undermining relatedness on alcohol use were tested. Mother’s undermining relatedness was a significant predictor (B= .82, SE =.39, p <.05). That is, increased mothers’ relatedness was associated with decreased odds of alcohol use. The interaction between treatment condition and mothers’ and children’s undermining relatedness was not significant. For marijuana use, neither mothers’ nor children’s interaction behaviors were significantly associated with mothers’ marijuana use. None of the interaction terms between treatment condition and mothers’ and children’s interaction behaviors were significant.
For cocaine use, mothers’ and children’s undermining autonomy was added to the two-part model of cocaine. The main effects of undermining autonomy were not significant. Further examination of the interaction between treatment condition and mothers’ and children’s undermining autonomy did not detect any significant interaction effects. In the next step, the effects of mothers’ and children’s undermining relatedness were examined. Similarly, neither the main effects of undermining relatedness nor the interaction between undermining relatedness and treatment condition was significant.
For opioid use, mothers’ and children’s undermining autonomy was added to the two-part model of opioid use. In Part 2 of the model, mothers’ undermining autonomy was negatively associated with her frequency of opioid use (B = −.19, SE =.09, p <.05). That is, mothers’ increased autonomy was associated with her more frequent use of opioids. A further test of the interaction between mothers’ undermining autonomy and treatment condition detected significant interaction effects (B=.30, SE=.13, p < .05), and showed that this association was only found in the WHE group (B = −.36, SE =.14, p <.01). In the next step, mothers’ and children’s undermining relatedness was added to the two-part model for opioid use. In Part 2 model, children’s undermining relatedness was positively associated with mothers’ opioid use (B = .26, SE =.12, p <.05), that is, children’s increased relatedness was associated with mothers’ decreased opioid use. Mothers’ undermining relatedness was not a significant predictor. However, a further test of interactions detected significant interaction effects between mothers’ undermining relatedness and treatment condition (B=.80, SE=.21, p<.001), and showed that only in the WHE group, mothers’ increased relatedness was associated with her more frequent use of opioids (B = −.52, SE =.12, p <.001).
In summary, the findings revealed that all mothers showed decreased alcohol, marijuana, cocaine, and opioid use over time. Mothers receiving EBFT showed decreased frequency of alcohol, marijuana, and cocaine use at a faster rate compared to mothers in WHE condition. For alcohol use, mothers’ increased relatedness was associated with a decreased likelihood of alcohol use. For opioid use, children’s increased relatedness was associated with mothers’ less frequent use of opioid. Surprisingly, although the main effects of mothers’ undermining relatedness were not significant, the findings showed that in the WHE group, mothers’ increased relatedness was associated with her more frequent use of opioids. Similarly, mothers’ increased autonomy was associated with her more frequent use of opioids only for those receiving WHE.
Discussion
Much research supports the reciprocal relationship between family interaction and alcohol and drug use among family members (Rowe, 2012). Even though family systems therapies acknowledge the reciprocal nature of family interaction on behavior, and research has examined the impact of parent-child interaction on child/infant outcomes (Kosterman et al., 1997), no investigation of parent-child interaction on maternal substance use was identified in the literature. Children are usually not included in the treatment plans of their mothers, even though children are often adversely affected by their mother’s substance use (Lussier, 2010). Further, stress in the mother-child relationship has been shown to contribute to women’s substance use (Lang, Pelham, Johnston, & Glernter, 1989; Pelham et al., 1997), but children have also been shown to be a motivating source of change for women (Milligan et al., 2010; Sword et al., 2009). The impact of including children in their mother’s substance use treatment is an overlooked intervention target that may prove to be potent in improving substance use outcomes for women.
The findings of this study supported the first hypothesis. Women receiving family systems therapy reported a faster decline of alcohol, marijuana and cocaine use compared to women in the individual therapy comparison condition. These findings support a literature evidencing the positive effects of family therapy as more effective than individual therapy for adolescent substance users (Rowe, 2012) and for couples in which one or both partners report an alcohol or drug problem (McCrady et al., 2009; O’Farrell & Fals-Stewart, 2006). That is, a faster decline in substance use can have a positive impact on the mother’s physical health, as well mental health (e.g., experiencing the positive psychological effects of success), potentially reinforcing continued change efforts. Future research might determine that quicker positive outcomes reinforce continued positive outcomes over time, including an increase in hope and connection with the mothers’ children. In general, differences between family therapies have not been observed, likely because of the similarity in underlying theoretical orientations among them. Therefore, while EBFT was chosen as the family systems therapy in this study, future research may find that other family systems therapies, regardless of the varying emphasis of the particular family systems approach, will be more effective than individual therapy or non-family systems therapy for women with children between the ages of 8–16 years in their care.
In general, the findings support a broad literature concluding that family therapy is not only a viable substance use treatment option, but may be among the more effective substance use treatments (see reviews, Fletcher, 2013; Rowe, 2012). This study extends these findings to mothers with children in their care. Among mothers, research indicates that interpersonal stress, including parent-child stress, results in increased substance use (Kalyva & Melonashi, 2014; Pelham et al., 1997). Therefore, addressing women’s interpersonal relationships in therapy offers the opportunity to ameliorate known risk factors for substance use, and to support ongoing sobriety. In addition, while the current study reports on the positive effects of family therapy on the mothers’ substance use (primary outcome), data also showed that children included in family therapy showed better behavioral outcomes than children not included in family therapy (Zhang, Slesnick, & Feng, under review). The impact of treatment on other participating family members further highlights the differential positive impact of family therapy on not just the mother, but also on her children, not observed in the individual therapy condition.
The second hypothesis of this study was that parent-child autonomy-relatedness would mediate the association between therapy and substance use outcomes. Findings showed that mothers and children showed improved autonomy-relatedness over time, evidenced by a decline in undermining autonomy and relatedness in both treatment conditions. However, no treatment effects on autonomy-relatedness were found, therefore our second hypothesis was not supported. However, upon further examination of these data, changes in observed autonomy-relatedness were linked to changes in substance use. In particular, in regard to opioid use, data indicate that as parents’ interaction behaviors change (improve) with therapy, when children are not included in the treatment process, mothers’ interactional changes resulted in poorer substance use outcomes. Interestingly, increased relatedness and autonomy among the mothers was associated with higher opioid use, but only for those in the non-family therapy condition. Family interaction represents a reciprocal process in which observed communication indicates change in interpersonal interaction. Theoretically, it is possible that when mothers change, and children do not, discrepancies in expectations or interaction patterns occur, resulting in children not reinforcing and responding to the positive changes by their mothers, and also resulting in poorer maternal substance use outcomes. In fact, some literature supports the observation that excluding family members from the treatment of substance users results in quicker relapse and poorer substance use outcomes (Rowe, 2012). Though more research is needed, these data provide some evidence that not including children in their mothers in treatment can harm substance use outcomes.
Compared to other substances, opioid use showed a different pattern of change, and also a different pattern of association with mother-child autonomy and relatedness behaviors. This finding supports an accumulating literature indicating that different drugs of choice influence family interaction differently and can result in different treatment response (Kelley & Fals-Stewart, 2002; Slesnick, Bartle-Haring, Glebova & Glade, 2006; Slesnick, Feng, Brakenhoff, & Brigham, 2014). For example, parental illicit drug use is associated with more severe family chaos, social, legal and financial stress, than parental alcohol use (Cooke, Kelley, Fals-Stewart, & Golden, 2004). Little is known in regard to the comparative effects of different illicit drugs and alcohol on family interaction and treatment response, suggesting the need for more research to uncover the different associations, as treatment strategies may need to differ depending upon the drug of choice. In sum, this study’s findings suggest that opioid use may have its own unique impact on family dynamics and response to treatment, needing further investigation.
Limitations
Limitations of the study include the use of a sample of convenience recruited from one substance use treatment facility in the Midwest. The current sample of mothers with children in their care who seek treatment for their substance use disorder may be different, possibly more motivated for change, compared to mothers without children in their care and who are not seeking treatment. Many women reported opioid use as their primary drug of choice, however, only a small number of women received medically assisted maintenance medications such as buprenorphine or methadone (N=21, 11.5%). Also, when women relapsed or continued to use alcohol or drugs, they often refused to meet with their therapist. In this study, therapists emphasized to women that regardless of their substance use, they wished to continue to meet in therapy, noting that therapy can help with concerns other than alcohol and drug use. In this way, we were able to successfully engage women using opioids (and other drugs) who were not receiving maintenance medication. Finally, the lack of observed mediation may be due to the interaction task which was limited to a recorded ten minute conflict resolution task which may have resulted in some level of bias among participants being on their best behavior (e.g., Hawthorne Effect). This could have resulted in reduced effects, requiring a larger sample size in order to detect mediation. A naturalistic observation of mother-child interaction conducted in the home over a longer period of time might result in a better estimation of change in family interaction associated with family therapy.
Conclusions
This study offers a unique contribution to the substance use treatment literature, showing that offering family therapy for mothers and their children improves the mothers’ substance use outcomes and can provide relational support to both the mother and child. Based upon these findings, it is recommended that substance use treatment facilities engage children of mothers who seek treatment. Further, Morgan, Crane, Moore and Eggett (2013) concluded that including family therapy in healthcare programs is associated with decreased service utilization over time. And, compared to other types of therapy, including individual therapy, family therapy was associated with the least cost (Morgan et al., 2013), offering additional evidence to support the use of family therapy in substance use treatment programming.
Acknowledgments
This work was funded through an NIH grant #R01DA023062, to the first author.
References
- Achenbach TM, Edelbrock CS. Manual for the Child Behavior Checklist and Child Behavior Profile. Burlington, VT: Child Psychiatry, University of Vermont; 1982. [Google Scholar]
- Allen JP, Hauser ST, Bell KL, O’Connor TG. Longitudinal assessment of autonomy and relatedness in adolescent-family interactions as predictors of adolescent ego development and self-esteem. Child Development. 1994;65:179–194. doi: 10.1111/1467-8624.ep9406130688. [DOI] [PubMed] [Google Scholar]
- Allen JP, Hauser ST, Bell KL, Tate DC, Insabella GM, et al. The autonomy and relatedness coding system. University of Virginia; 2000. Unpublished manuscript. [Google Scholar]
- Allen JP, Porter M, McFarland C, McElhaney KB, Marsh P. The relation of attachment security to adolescents’ paternal and peer relationships, depression, and externalizing behavior. Child Development. 2007;78:1222–1239. doi: 10.1111/j.1467-8624.2007.01062.x. http://dx.doi.org/10.1111/j.1467-8624.2007.01062.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brigham GS. 12-Step participation as a pathway to recovery: the Maryhaven experience. NIDA Science & Practice Perspectives. 2003 Sep;2(1) doi: 10.1151/spp032143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Substance Abuse Treatment. Substance abuse treatment: addressing the specific needs of women. Rockville, MD: SAMHSA; 2009. (HHS Publication No. (SMA) 09-4426) [PubMed] [Google Scholar]
- Chaplin TM, Aldao A. Gender differences in emotion expression in children: A meta-analytic review. Psychological Bulletin. 2013;139:735–765. doi: 10.1037/a0030737. http://dx.doi.org/10.1037/a0030737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheong J, MacKinnon DP, Khoo ST. Investigation of mediational processes using parallel process latent growth curve modeling. Structural Equation Modeling. 2003;10:238–262. doi: 10.1207/S15328007SEM1002_5. http://dx.doi.org/10.1207/s15328007sem1002_5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooke CG, Kelley ML, Fals-Stewart W, Golden J. A comparison of the psychosocial functioning of children with drug-versus alcohol-dependent fathers. The American Journal of Drug and Alcohol Abuse. 2004;30:695–710. doi: 10.1081/ada-200037530. http://dx.doi.org/10.1081/ada-200037530. [DOI] [PubMed] [Google Scholar]
- Denton WH, Adinoff BH, Lewis D, Walker R, Winhusen T. Family discord is associated with increased substance use for pregnant substance users. Substance Use & Misuse. 2014;49:326–332. doi: 10.3109/10826084.2013.840002. http://dx.doi.org/10.3109/10826084.2013.840002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiClemente CC. Motivation for change: Implications for substance abuse treatment. Psychological Science. 1999;10:209–213. http://dx.doi.org/10.1111/1467-9280.00137. [Google Scholar]
- Enlow MB, Englund MM, Egeland B. Maternal childhood maltreatment history and child mental health: Mechanisms in intergenerational effects. Journal of Clinical Child & Adolescent Psychology. 2016 doi: 10.1080/15374416.2016.1144189. Online First: http://dx.doi.org/10.1080/15374416.2016.1144189. [DOI] [PMC free article] [PubMed]
- Fletcher K. Couple therapy treatment for substance use disorders: A systematic review. Journal of Social Work Practice in the Addictions. 2013;13:327–352. http://dx.doi.org/10.1080/1533256x.2013.840213. [Google Scholar]
- Friedman D, Holmbeck GN, DeLucia C, Jandasek B, Zebracki K. Trajectories of autonomy development across the adolescent transition in children with spina bifida. Rehabilitation Psychology. 2009;54:16–27. doi: 10.1037/a0014279. http://dx.doi.org/10.1037/a0014279. [DOI] [PubMed] [Google Scholar]
- Greenfield SF, Books AJ, Gordon SM, Green CA, Kropp F, McHugh RK, … Miele GM. Substance abuse treatment entry, retention, and outcome in women: A review of the literature. Drug and Alcohol Dependence. 2007;86:1–21. doi: 10.1016/j.drugalcdep.2006.05.012. http://dx.doi.org/10.1016/j.drugalcdep.2006.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hien DA, Jian H, Campbell ANC, Hu MC, Miele G, Cohen L, … Nunes E. Do treatment improvements in PTSD severity affect substance use outcomes? A secondary analysis from a randomized clinical trial in NIDA’s Clinical Trials Network. American Journal of Psychiatry. 2010;167:95–101. doi: 10.1176/appi.ajp.2009.09091261. http://dx.doi.org/10.1176/appi.ajp.2009.09091261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hien DA, Wells EA, Jiang H, Suarez-Morales L, Campbell A, Cohen LR, … Nunes EV. Multi-site randomized trial of behavioral interventions for women with co-occurring PTSD and substance use disorders. Journal of Consulting and Clinical Psychology. 2009;77:607–619. doi: 10.1037/a0016227. http://dx.doi.org/10.1037/a0016227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmbeck GN, Westhoven VC, Philips WS, Bowers R, Gruse C, Nikolopoulos T, … Davison K. A multimethod, multi-informant, and multidimensional perspective on psychosocial adjustment in preadolescents with spina bifida. Journal of Consulting and Clinical Psychology. 2003;71:782–796. doi: 10.1037/0022-006x.71.4.782. http://dx.doi.org/10.1037/0022-006x.71.4.782. [DOI] [PubMed] [Google Scholar]
- Isenhart CE. Motivational subtypes in an inpatient sample of substance abusers. Addictive Behaviors. 1994;19:463–475. doi: 10.1016/0306-4603(94)90002-7. http://dx.doi.org/10.1016/0306-4603(94)90002-7. [DOI] [PubMed] [Google Scholar]
- Kalyva E, Melonashi E. Reported maternal styles and substance use: A cross-sectional study among educated Albanian young adults. Substance Use & Misuse. 2014;49:654–660. doi: 10.3109/10826084.2013.846377. http://dx.doi.org/10.3109/10826084.2013.846377. [DOI] [PubMed] [Google Scholar]
- Kelley ML, Fals-Stewart W. Couples- versus individual-based therapy for alcohol and drug abuse: Effects on children’s psychosocial functioning. Journal of Consulting and Clinical Psychology. 2002;70(2):417–427. doi: 10.1037//0022-006x.70.2.417. http://dx.doi.org/10.1037/0022-006x.70.2.417. [DOI] [PubMed] [Google Scholar]
- Kosterman R, Hawkins JD, Spoth R, Haggerty KP, Zhu K. Effects of a preventative parent-training intervention on observed family interactions: Proximal outcomes from preparing for the drug free years. Journal of Community Psychology. 1997;25:337–352. http://dx.doi.org/10.1002/(sici)1520-6629(199707)25:4<337::aid-jcop3>3.0.co;2-r. [Google Scholar]
- Lang AR, Pelham WE, Johnston C, Gelernter S. Levels of adult alcohol consumption induced by interactions with child confederates exhibiting normal versus externalizing behaviors. Journal of Abnormal Psychology. 1989;98:294–299. doi: 10.1037//0021-843x.98.3.294. http://dx.doi.org/10.1037/0021-843x.98.3.294. [DOI] [PubMed] [Google Scholar]
- Lussier K, Laventure M, Bertrand K. Parenting and maternal substance addiction: Factors affecting utilization of child protective services. Substance Use & Misuse. 2010;45:1572–1588. doi: 10.3109/10826081003682123. http://dx.doi.org/10.1037/e516652013-080. [DOI] [PubMed] [Google Scholar]
- Margolin G, Talovic S, Weinstein CD. Areas of Change Questionnaire: A practical approach to marital assessment. Journal of Consulting and Clinical Psychology. 1983;51:920–931. http://dx.doi.org/10.1037//0022-006x.51.6.944. [Google Scholar]
- McCrady BS, Epstein EE, Cook SM, Jensen N, Hildebrandt T. A randomized trial of individual and couple behavioral alcohol treatment for women. Journal of Consulting and Clinical Psychology. 2009;77:243–256. doi: 10.1037/a0014686. http://dx.doi.org/10.1037/a0014686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR. Project MATCH Monograph Series. Vol. 5. U.S. Dept. of Health; Bethesda, MD: 1996. Form 90 a structured assessment interview for drinking and related problem behaviors. [Google Scholar]
- Miller WR, Marlatt GA. Manual for the Comprehensive Drinker Profile. Odessa, FL: Psychological Assessment Resources; 1984. [Google Scholar]
- Miller S, Pagan D, Tross S. Women’s Health Education. In Peer activism for female partners of injection drug users. Columbia University; 1998. Unpublished treatment manual. [Google Scholar]
- Miller WR, Rollnick S. Meeting in the middle: Motivational interviewing and self-determination theory. The International Journal of Behavioral Nutrition and Physical Activity. 2012;9:25. doi: 10.1186/1479-5868-9-25. http://dx.doi.org/10.1186/1479-5868-9-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, Tonigan JS. Assessing drinkers’ motivation for change: The Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES) Psychology of Addictive Behaviors. 1996;10:81–89. http://dx.doi.org/10.1037/10248-014. [Google Scholar]
- Milligan K, Niccols A, Sword W, Thabane L, Henderson J, Smith A, Liu J. Maternal substance use and integrated treatment programs for women with substance abuse issues and their children: A meta-analysis. Substance Abuse Treatment, Prevention, and Policy. 2010;5:21. doi: 10.1186/1747-597X-5-21. http://dx.doi.org/10.1186/1747-597x-5-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan TB, Crane DR, Moore AM, Eggett DL. The cost of treating substance use disorders: Individual versus family therapy. Journal of Family Therapy. 2013;35:2–23. http://dx.doi.org/10.1111/j.1467-6427.2012.00589.x. [Google Scholar]
- Murray CB, Amaro CM, Devine KA, Psihogios AM, Murphy LK, Holmbeck GN. Observed macro- and micro-level parenting behaviors during preadolescent family interactions as predictors of adjustment in emerging adults with and without spina bifida. Journal of Pediatric Psychology. 2015;40:18–32. doi: 10.1093/jpepsy/jsu030. http://dx.doi.org/10.1093/jpepsy/jsu030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén B. Beyond SEM: General latent variable modeling. Behaviormetrika. 2002;29:81–117. http://dx.doi.org/10.2333/bhmk.29.81. [Google Scholar]
- Muthén BO, Muthén LK. Mplus user’s guide. 7. Los Angeles, CA: Author; 2012. [Google Scholar]
- Niccols A, Milligan K, Sword W, Thabane L, Hendrson J, Smith A. Integrated programs for mothers with substance abuse issues: A systematic review of studies reporting on parenting outcomes. Harm Reduction Journal. 2012;9:14. doi: 10.1186/1477-7517-9-14. http://dx.doi.org/10.1186/1477-7517-9-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Farrell TJ, Fals-Stewart W. Behavioral couples therapy for alcoholism and drug abuse. New York: Guilford Press; 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olens MK, Schafer JL. A two-part random-effects model for semicontinuous longitudinal data. Journal of the American Statistical Association. 2001;96:730–745. http://dx.doi.org/10.1198/016214501753168389. [Google Scholar]
- Oudekerk BA, Allen JP, Hessel ET, Molloy LE. The cascading development of autonomy and relatedness from adolescence to adulthood. Child Development. 2015;86:472–485. doi: 10.1111/cdev.12313. http://dx.doi.org/10.1111/cdev.12313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelham WE, Lang AR, Atekson B, Murphy DA, Gnagy EM, Greiner AR, … Greenslade KE. Effects of deviant child behavior on parental distress and alcohol consumption in laboratory interactions. Journal of Abnormal Child Psychology. 1997;25:413–424. doi: 10.1023/a:1025789108958. [DOI] [PubMed] [Google Scholar]
- Rowe CL. Family therapy for drug abuse: Review and updates 2003–2010. Journal of Marital and Family Therapy. 2012;38:59–81. doi: 10.1111/j.1752-0606.2011.00280.x. http://dx.doi.org/10.1111/j.1752-0606.2011.00280.x. [DOI] [PubMed] [Google Scholar]
- Slesnick N, Bartle-Haring S, Glebova T, Glade A. Primary alcohol versus primary drug use among adolescents: An examination of differences. Addictive Behaviors. 2006;31:2080–2093. doi: 10.1016/j.addbeh.2006.02.006. http://dx.doi.org/10.1016/j.addbeh.2006.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slesnick N, Feng X, Brakenhoff B, Brigham G. Parenting under the influence: The effects of opioids, alcohol and cocaine on mother-child interaction. Addictive Behaviors. 2014;39:897–900. doi: 10.1016/j.addbeh.2014.02.003. http://dx.doi.org/10.1016/j.addbeh.2014.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slesnick N, Guo X, Brakenhoff B, Bantchevska D. A comparison of three interventions for homeless youth evidencing substance use disorders: Results of a randomized clinical trial. Journal of Substance Abuse Treatment. 2015;54:1–13. doi: 10.1016/j.jsat.2015.02.001. http://dx.doi.org/10.1016/j.jsat.2015.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slesnick N, Prestopnik J. Comparison of family therapy outcome with alcohol abusing, runaway adolescents. Journal of Marital and Family Therapy. 2009;35:255–277. doi: 10.1111/j.1752-0606.2009.00121.x. http://dx.doi.org/10.1111/j.1752-0606.2009.00121.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slesnick &, Prestopnik J. Ecologically-based family therapy outcome with substance abusing runaway adolescents. Journal of Adolescence. 2005;28:277–298. doi: 10.1016/j.adolescence.2005.02.008. http://dx.doi.org/10.1016/j.adolescence.2005.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA) Summary of findings from the 2008 National Household Survey on Drug Use and Health. Rockville, MD: SAMHSA; 2009. [Google Scholar]
- Sword W, Jack S, Niccols A, Milligan K, Henderson J, Thabane L. Integrated programs for women with substance use issues and their children: A qualitative meta-synthesis of processes and outcomes. Harm Reduction Journal. 2009;6:32. doi: 10.1186/1477-7517-6-32. http://dx.doi.org/10.1186/1477-7517-6-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tonigan J, Miller WR, Brown JM. The reliability of Form 90: An instrument for assessing alcohol treatment outcome. Journal of Studies on Alcohol. 1997;58:358–364. doi: 10.15288/jsa.1997.58.358. http://dx.doi.org/10.15288/jsa.1997.58.358. [DOI] [PubMed] [Google Scholar]
- Tuchman E. Women and addiction: The importance of gender issues in substance abuse research. Journal of Addictive Diseases. 2010;29:127–138. doi: 10.1080/10550881003684582. http://dx.doi.org/10.1176/foc.9.1.foce90. [DOI] [PubMed] [Google Scholar]
- Westerberg VS, Tonigan JS, Miller WR. Reliability of Form 90D: An instrument for quantifying drug use. Substance Use. 1998;19:179–189. doi: 10.1080/08897079809511386. http://dx.doi.org/10.1080/08897079809511386. [DOI] [PubMed] [Google Scholar]