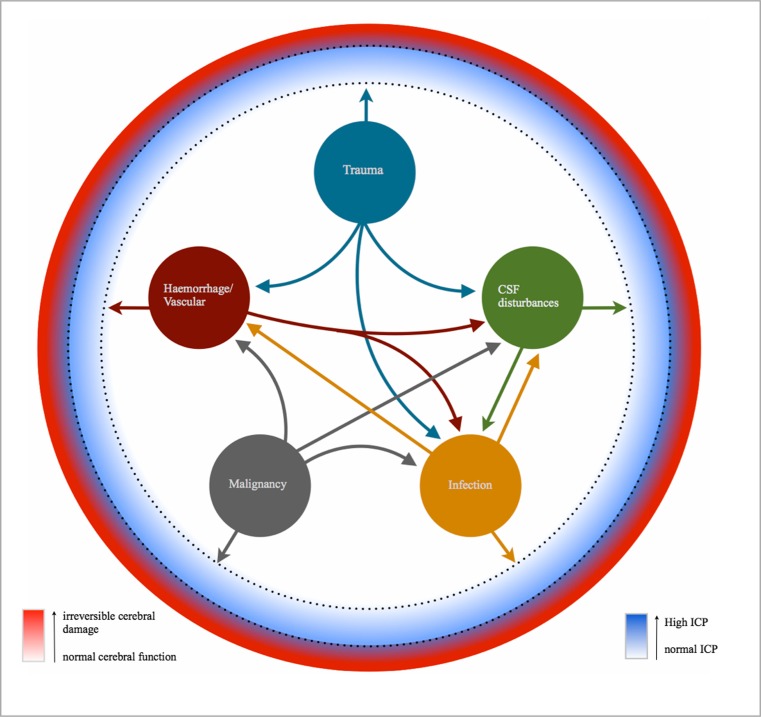
Fig. 5.
The relationship between the different intracranial pathological categories and the ICP, cerebral function, RAP index and AMP. Intracranial pathologies can be categorised into five main areas. The large circles represent the initial/primary pathology, with the arrows showing the potential secondary pathologies that can arise from the corresponding initial/primary pathology. For example, trauma can cause a direct increase in the ICP through the expansion of the cerebral parenchyma; however trauma can also result in damage to blood vessels with resulting haemorrhage, or a disturbance within CSF dynamics, e.g., expanding tissue resulting in blockage of the CSF drainage pathways or an increased risk of infection, which could cause a rise in the ICP through increased metabolic turnover. Note that the initial/primary pathology may itself not cause a significant rise in ICP; however the resulting secondary pathologies could be responsible for the rise in ICP, for example a malignant tumour itself may not cause a rise in ICP; however if the surrounding blood vessels rupture then it will be the resulting haemorrhage that will cause the rise in ICP. The nature of the primary pathology will determine what potential secondary pathologies could arise. The dotted circumferential lines represent the interval at which the RAP index and AMP would be most clinically useful. If changes in the AMP and/or RAP index are detected through ICP monitoring before the patient exhibits any signs/symptoms, then this could allow the clinician to implement a change in management sooner and therefore minimise irreversible damage to the brain tissue and subsequently improve patient outcome