Abstract
Background
Though Janani Suraksha Yojana (JSY) under National Rural Health Mission (NRHM) is successful in increasing antenatal and natal care services, little is known on the cost coverage of out-of-pocket expenditure (OOPE) on maternal care services post-NRHM period.
Methods
Using data from a community-based study of 424 recently delivered women in Rajasthan, this paper examined the variation in OOPE in accessing maternal health services and the extent to which JSY incentives covered the burden of cost incurred. Descriptive statistics and logistic regression analyses are used to understand the differential and determinants of OOPE.
Results
The mean OOPE for antenatal care was US$26 at public health centres and US$64 at private health centres. The OOPE (antenatal and natal) per delivery was US$32 if delivery was conducted at home, US$78 at public facility and US$154 at private facility. The OOPE varied by the type of delivery, delivery with complications and place of ANC. The OOPE in public health centre was US$44 and US$145 for normal and complicated delivery, respectively. The share of JSY was 44 % of the total cost per delivery, 77 % in case of normal delivery and 23 % for complicated delivery. Results from the log linear model suggest that economic status, educational level and pregnancy complications are significant predictors of OOPE.
Conclusions
Our results suggest that JSY has increased the coverage of institutional delivery and reduced financial stress to household and families but not sufficient for complicated delivery. Provisioning of providing sonography/other test and treating complicated cases in public health centres need to be strengthened.
Keywords: OOPE, Antenatal care, Delivery care, Cash assistance scheme, India
Background
Since the millennium declaration, the global, national and regional efforts to improve health-related millennium goals (reduction of maternal mortality and child mortality) in developing countries were intensified. Improving the maternal health services become the leading strategy to reduce maternal and child mortality. Several innovative programmes from many developing countries including the conditional cash transfer schemes in India (Janani Surakhya Yojana), Nepal (safe delivery incentive program) and Bangladesh (maternal health voucher schemes in Bangladesh) were introduced to increase the demand for maternal health services specifically among poor and marginalised. A large and growing literature from these countries suggests the functioning, utility and limitations of these programmes [1–18]. Though these programmes were context specific and differ by design and implementation strategy, they had the common goal to reduce the out-of-pocket expenditure on maternal care and increase the access to maternal services among the poor and marginalised. A number of evaluation studies reported the spectacular success of the various schemes in increasing access to maternal services [9, 11, 16, 17, 19]. Despite these programmes in place, the progress in health-related Millennium Development Goals is slow and largely uneven across regions, income groups and by social attributes [20–23].
India accounts one fourth of child mortality and one fifth of maternal mortality worldwide [24, 25]. The inequalities in health outcome and health care utilisation are large across geography, economic status and education [26–29] and largely resulting from financial, cultural and social constraints. In India, in the year 2004–2005, about one fourth of the mothers who did not deliver at health centre reported cost as barrier for not availing the services [30]. Especially poor households consider spending a huge amount on child-bearing deterrent, leading to low health care utilisation among them. This is also corroborated by the fact that the out-of-pocket expenditure on health care accounts about two thirds of the total health expenditure [31] and health expenditure is often catastrophic [32, 33]. Though the maternal health services were free in public health centres, there were charges on medicine, bed, user fees and bribe [34–37].
Recognising that an increase in the level of utilisation of health care for child birth may lead to a reduction in the maternal mortality and neonatal mortality, the Ministry of Health and Family Welfare, Government of India, launched conditional cash transfer scheme, i.e., Janani Suraksha Yojana (JSY) (Janani denotes to mother, Surakasha for protection/safety and Yojana means scheme), to address the delays of decision-making, transportation and access to services. The JSY is a flagship intervention programme under National Rural Health Mission (NRHM), launched in April 2005. The JSY scheme covered transport cost, delivery cost and incentive to Accredited Social Health Activists (ASHAs) for motivating women to opt for institutional delivery. It also facilitated public-private partnerships by providing accreditation to private hospitals/nursing homes for delivery services. The cash incentive of INR 1400 (US$30) to recent mothers was given at the time of discharge from the hospital after verifying all the records.
Since the implementation of NRHM, the institutional deliveries in India had increased from 41 % in 2005–2006 to 81 % in 2013–2014 [30, 38] and the infant mortality declined from 58 infant deaths in 2005 [39] to 35 infant deaths per 1000 live births in 2013–2014 [38]. The maternal mortality ratio (MMR) had declined from 254 in 2004–2006 to 167 per 100,000 live births in 2011–2013 [40, 41]. A number of state specific studies were also undertaken to inform the functioning and progress of NRHM in general and JSY in particular [15, 42–45]. The gap (for institutional deliveries) between low and high performing states started reducing despite the fact that there was no differential change in the availability and access of any health facility [43]. This indicated that people were able to avail skilled care at the time of delivery irrespective of the economic status.
Studies on OOPE consistently report higher expenditure for deliveries conducted in private health care centres and for complicated deliveries and caesarean deliveries [32, 46–54]. The OOPE for antenatal care in child-bearing process was also found much higher than delivery care alone [55]. The expenses incurred during child bearing also varied with the place of antenatal care (ANC), indicating that the contact with private facility at any stage of pregnancy will increase cost per delivery [52]. A normal delivery in a health care facility in Nepal was US$64 compared to US$129 per caesarean delivery while excluding opportunity cost [54]. Similarly, in the case of India before NRHM, the cost per delivery in a public and private health institution was US$25 and USD$104, respectively, whereas average cost at antenatal care was US$10 [32]. For Bangladesh, these costs were US$85 and US$181 [56]. The cost per complicated delivery was significantly higher in Tanzania, Africa, Kenya, Burkina Faso and Lao PDR [46, 50–52].
Though a number of studies have examined on the coverage of maternal care services, differentials in OOPE by type of health facility, there are not many studies on cost of antenatal care and the coverage of JSY incentives. The aim of this study is to examine the variation in out-of-pocket expenditure in accessing maternal health services (antenatal and delivery care) and the extent to which the JSY incentives covered the burden of cost incurred.
The paper has been conceptualised with the rationale. First, the cost was one of the major barriers in availing the antenatal and natal care among poor and marginalised. This has particular bearing in the state of Rajasthan that has higher infant and maternal mortality than national average and large variation in maternal care utilisation among different population sub-groups within the state. Second, because of poor quality of the services at public health care institutions, utilisation of maternal health services from private sector increased over a period of time, which had a significant burden on the economic condition of households across various socio-economic groups. Also, women switch the service provider from public to private and vice versa during pregnancy and child birth. No attempt has been made to capture this pattern of service utilisation. Third, it is important to document to what extent the large investment on maternal care under the NRHM helped in the reduction of cost for end users. This is generally of great interest to policy makers and planners for evidence-based policy-making.
Methods
This paper is based on a cross-sectional study conducted in Rajasthan during April to May 2011. The state of Rajasthan with a population of 69 million in 2011 [57] had the second highest maternal mortality ratio in the country (255 per 100,000 live births) [41] and at low level of socio-economic development. The study was conducted in the four districts of Rajasthan, namely, Udaipur and Banswara (tribal districts—with 49.7 and 76.4 % tribal population, respectively), and Sikar and Sawai Madhopur (nontribal districts). A multi-stage sampling was used to select the sample. From each selected district, two blocks were identified based on the highest and lowest proportion of institutional deliveries. Data on number of deliveries was obtained from Pregnancy and Child Tracking System of Government of Rajasthan (Management Information System—MIS). In this system, information from each village of Rajasthan is being recorded with the help of ground level health care workers. Government claims to maintain the data on all the pregnancies occurred in Rajasthan. From each of the blocks, two primary health centres (PHCs) were selected based on their performance on institutional deliveries (highest and lowest). From each PHC (in total 16), two villages were selected randomly. All the women who gave births (JSY beneficiaries and non-beneficiaries) 1 year prior to survey (during April 2010–March 2011) were interviewed from 32 villages of four districts. A list of women who gave birth during the period was obtained from ASHA (Accredited Social Health Activist) and ANM (Auxiliary Nurse Midwife) of the village. A total of 424 women were successfully interviewed under the study. A structure interview schedule was prepared for data collection and pre-tested in a village before final survey. Data was collected on multiple issues related to accessibility, availability and utilisation of services including cost incurred during pregnancy, delivery and post-delivery and money received under JSY.
The direct cost incurred during childbearing (pregnancy and delivery) was termed as out-of-pocket expenditure (OOPE). The OOPE includes (a) expenditure during antenatal care such as registration fees, doctor’ fee, medicine, tests, sonography and transportation and (b) expenditure incurred during delivery—registration, transportation, doctor, medicine, tests, bed and food. The amount spend on bribe and gift was not included in the study. The cost incurred during postnatal care primarily included the cost on child health, therefore not included in the expenditure on maternal care. The OOPE in the paper is synonymous to the total expenditure incurred during a pregnancy/delivery irrespective of JSY amount. There were a few cases where the expenditure was very large. To reduce the variation, we have levelled the value at 95 % level; e.g., those 5 % women with higher than OOPE (antenatal care) of US$179 were kept at US$179, and similar approach was followed for computing expenditure during natal care. The total OOPE was adjusted to average US$ in the year 2010–2011 (US$1 = 46.2 INR) [58]. The term normal delivery is defined as the delivery without any complication.
Descriptive statistics (mean, confidence interval, per cent distribution) was carried out to understand the differentials in OOPE on antenatal and natal care. A log linear regression model was used to understand the significant predictors of OOPE. Log of OOPE (continues variable) is the dependent variable. The independent variables are both continuous and categorical. The continuous variables are education, age, duration of stay in hospital and birth order. The categorical variables are BPL status of the family, complications during pregnancy and delivery, received JSY incentives and place of ANC.
Ethics
Ethical clearance for conducting the study was taken from the ethical board of Indian Institute of Health Management Research (IIHMR), Jaipur. Verbal informed consent was taken from women participating in study with the assurance that confidentiality will be maintained and information obtained for this study will not be used for any other purposes except for research.
Results
Table 1 presents the descriptive statistics of the study population. The mean age of the women was 25.7 years, and about half of them were illiterate. Half of the women belonged to schedule caste/tribe, and more than half were working for wages or kind. About one third of the women were living below poverty line (BPL). Most of the women had received at least three or more antenatal check-ups with a mean of 3.5. The distribution of women by source of antenatal care showed that 43 % women availed the antenatal check-up exclusively from public facilities, 21 % from private facilities and 36 % from both public and private facilities. However, the coverage of full antenatal care (3 check-up + 2 tetanus toxoid (TT) injections + received 90 iron folic acid (IFA) tablets) was only 24 %. On the other hand, the proportion of institutional deliveries was 83: 62 % delivered in public health facilities, 17 % at private health facilities and 3.5 % at accredited private health facilities. Of total, 66 % of the women received incentives under JSY. Almost all women who delivered at public health facilities received JSY incentives (96 % had already received and 4 % were about to receive at the time of survey). More than half of the respondents (57 %) had received any postnatal care (PNC).
Table 1.
Sample profile of the women covered under the study in Rajasthan, 2011 (N = 424)
| Background characteristics | Percentage | n |
|---|---|---|
| Literacy rate | 44.8 | 190 |
| Caste | ||
| Schedule caste | 13.0 | 55 |
| Schedule tribe | 37.7 | 160 |
| Other backward saste | 34.7 | 147 |
| Others | 14.6 | 62 |
| Working | 52.8 | 224 |
| Households possessing BPL card | 33.3 | 141 |
| Mothers received 3 or more ANC | 76.9 | 326 |
| Full antenatal care (3 ANC + 2 TT + received 90 IFA) | 24.3 | 103 |
| Place of antenatal care | ||
| No ANC | 1.2 | 5 |
| Public facility | 42.9 | 182 |
| Private facility | 20.5 | 87 |
| At both public and private facility | 35.4 | 150 |
| Place of delivery | ||
| Public facility | 62.3 | 264 |
| Accredited private facility | 3.5 | 15 |
| Private facility | 17.2 | 73 |
| Home | 17.0 | 72 |
| Mothers received incentives under JSY | 65.8 | 279 |
| Mothers received postnatal care | 57.0 | 241 |
Figure 1 presents the out-of-pocket expenditure (OOPE) on antenatal care by place of antenatal care. It may be mentioned that the OOPE on antenatal services includes costs incurred on registration, fee to the doctor, medicines, blood and urine tests, sonography and transportation. The mean OOPE on antenatal care was US$41 (95 % CI 37–45), US$26 in public health facilities and US$64 for those availed services at private health facilities. Women, who availed antenatal care services exclusively from private facility, spend nearly two and a half times higher than women who availed services exclusively from public health facility. Women who availed at both public and private health facilities spent UD$49.
Fig. 1.
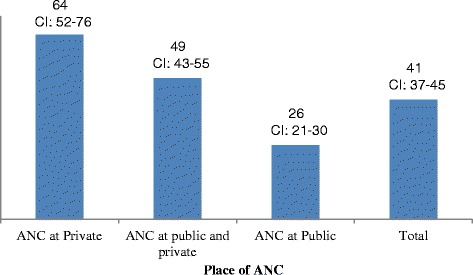
OOPE (in US$) on antenatal care by place of antenatal care, Rajasthan, 2011
Though all women reported the total cost on antenatal care, only 23 % could provide the expenditure incurred on various services during antenatal care. The share of medicine in OOPE was 59 % followed by sonography (18 %), blood tests (8 %), transporation (8 %) and doctor consultation (7 %). It varied almost in the similar proportion among women who received antenatal care exclusively from public facility, private facility or from both public and private facilities. If women received ANC from public sector, they spent 53 % on medicine, 19 % on sonography, 9 % on tests, 12 % on transportation and 7 % on doctor’s fee of total OOPE. And, this proportion was 60, 17, 7, 9 and 7 %, respectively, if they went to private sector for antenatal care.
OOPE on delivery care
The OOPE on delivery care and antenatal and delivery care (together) by place delivery is presented in Table 2. The OOPE on delivery was US$44, US$51 for institutional deliveries and US$10 for home deliveries. The OOPE at public health centre was estimated at US$39 compared to US$88 in private health facilities and US$72 for accredited private health facilities. By considering the expenditure on antenatal and delivery care, the total OOPE expenditure was estimated at US$85. The OOPE expenditure on antenatal and delivery care in public health centre was significantly lower (US$78 per delivery) compared to US$154 in private health centre and US$133 at accredited private health centre.
Table 2.
OOPE* (in US$) on delivery care and antenatal and delivery care by place of delivery in Rajasthan, 2011
| Place of Delivery | Expenditure (in US$) during | N | |||
|---|---|---|---|---|---|
| Delivery care | Antenatal and delivery care | ||||
| Mean | 95 % CI | Mean | 95 % CI | ||
| Institutiona | 51 | 46–56 | 96 | 87–105 | 352 |
| Public facility | 39 | 34–45 | 78 | 69–87 | 264 |
| Accredited private facility | 72 | 44–101 | 133 | 91–176 | 15 |
| Private facility | 88 | 75–102 | 154 | 131–176 | 73 |
| Home | 10 | 7–12 | 32 | 25–40 | 72 |
| Total | 44 | 39–49 | 85 | 78–93 | 424 |
*JSY incentive has not been deducted from OOPE
aInstitutional includes private, public and accredited private health facilities
A pregnant woman may avail antenatal care services from private health care facility and deliver at a public health facility or vice versa. This behaviour would affect the OOPE occurred during the child-bearing process. Percent distribution of women by place of antenatal care and delivery is shown in Table 3. Among women who delivered at public health centre, half of them obtained antenatal care services from public facility and nearly one third of them availed antenatal care services both from public and private facility. It is interesting to note that among women who delivered at private facility, 48 % of them received antenatal care services from both public and private health facility. Further analysis of OOPE revealed that the expenses incurred varied significantly with the place of antenatal care and delivery. When all antenatal check-ups were availed from public health facility, and the delivery too was conducted at public health facility, the average OOPE was US$59. However, when the place of delivery was private facility, the average expenditure increased to US$97 and exceeds spending of US$38 over the amount spent on delivery at public health facility (Table 3).
Table 3.
Place of delivery by place of ANC (%) and OOPE* by place of delivery and antenatal care (in US$) in Rajasthan, 2011
| Place of antenatal care | Place of delivery | |||||
|---|---|---|---|---|---|---|
| Percentage | OOPE (in US$) | |||||
| Public facility | Private facility | Home | Public facility | Private facility | Home | |
| Public facility | 52.7 | 14.8 | 44.9 | 59 (CI 50–69) | 97 (CI 39–154) | 21 (CI 12–30) |
| Private facility | 13.4 | 37.5 | 27.5 | 107 (CI 75–140) | 183 (CI 149–217) | 32 (CI 17–48) |
| Both public and private facility | 34.0 | 47.7 | 27.5 | 97 (CI 82–111) | 141 (CI 115–167) | 55 (CI 39–72) |
*JSY incentive has not been deducted from OOPE
When a woman availed antenatal services at private health facility but chose to deliver at public facility, the OOPE was US$107. As expected, the respondents who received ANC services at private and delivered at private health facility spend US$183. OOPE among women who availed ANC services both from public and private health facility or delivered at private revealed that the contact with private health facility at any stage of child-bearing process increased the OOPE.
Complications and OOPE
Table 4 describes the OOPE on antenatal and delivery care by complications. In general, the OOPE increases with complications both during pregnancy and delivery. For example, a normal delivery without any complication at home costs an average of US$14, US$44 at public facility and US$92 at private facility. Complications during pregnancy alone had contributed to increase in expenditure. Respondents who suffered from complications during pregnancy and delivered at public health facility had spent US$72. Women who suffered from complications both during pregnancy and delivery spent an average of US$145 in public facility delivery and US$197 for private health facility delivery.
Table 4.
OOPE* (in US$) on antenatal and delivery care by pregnancy and delivery complications# and place of delivery in Rajasthan, 2011
| Complications | Place of delivery | ||||
|---|---|---|---|---|---|
| Institutional | Public | Private | Home | ||
| Normal deliveries | Mean | 52 | 44 | 92 | 14 |
| 95 % CI | 41–62 | 33–55 | 61–124 | 8–20 | |
| N | 83 | 70 | 13 | 29 | |
| Complications during pregnancy but not during delivery | Mean | 90 | 72 | 141 | 44 |
| 95 % CI | 80−100 | 63−81 | 118−164 | 33−56 | |
| N | 189 | 140 | 49 | 36 | |
| Complications during pregnancy and delivery | Mean | 163 | 145 | 197 | 48 |
| 95 % CI | 139−187 | 124−173 | 152−243 | 13−84 | |
| N | 76 | 50 | 26 | 7 | |
| Complications during pregnancy or delivery | Mean | 110 | 90 | 160 | 45 |
| 95 % CI | 99−120 | 80−101 | 138−183 | 34−55 | |
| N | 269 | 194 | 75 | 43 | |
*JSY incentive has not been deducted from OOPE
#the number of cases was less (four each in public and private facility delivery) in the case of no complication during pregnancy but complications during delivery, therefore, dropped from analysis
Share of JSY incentives on cost of antenatal and delivery care
Figure 2 provides OOPE and JSY incentives provided by government per delivery. As stated elsewhere, the OOPE in public facility was US$78. Further, it was US$44 and 145 for normal and complicated delivery, respectively. Since the government was reimbursing US$34 directly to the beneficiary as JSY incentive, it was deducted from OOPE to get the actual expenditure made by the beneficiary per delivery. After deducting JSY incentives, OOPE per delivery was estimated at US$44. The government share accounts 44 % of OOPE per delivery, 77 % for normal delivery, 38 % for delivery that had complications during pregnancy or delivery and 23 % for those deliveries who had complications both during delivery and pregnancy.
Fig. 2.
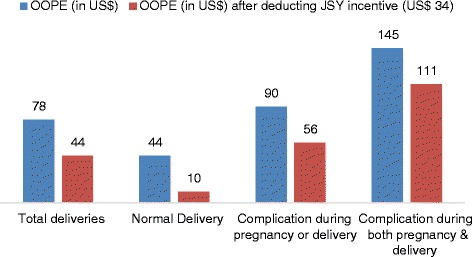
Cost (in US$) per delivery (OOPE and after deducting JSY incentives) in public facilities in Rajasthan, 2011
Socio-economic differentials in OOPE
Table 5 provides the socio-economic differentials in institutional delivery and OOPE. Comparatively larger proportion of younger women opted for institutional deliveries than older women. After deducting JSY incentives the mean OOPE of younger women (below 25 years) was US$57 compared to US$48 among women aged 25 years and above (US$57 vs. US$48). Similarly, women with general caste spend almost double than other caste women even after deducting JSY incentives. Nearly two-third women from BPL and 59 % from APL delivered at public health centre. Among these, a BPL family spends US$56 on antenatal and delivery care compared to US$91 among APL families. JSY incentives were received by both the sections. JSY incentives reduced the total cost by 47 % among BPL families and 32 % among APL families. Almost the same proportion of literate and illiterate women delivered in public facilities; their expenditure on antenatal and delivery care varied significantly (for illiterate US$68; for literate US$91). Results were similar by husband’s literacy status; in the case of literate husband, the spending on antenatal and natal care was almost double than when husband was illiterate. JSY incentives shared the expenditure to a greater extend in the family where husband was illiterate, even more than where a woman was illiterate. As the birth order increased, the proportion who delivered at institution and the expenditure on antenatal and delivery care reduced. Women, who delivered for the first time, spend US$90 as compared to women who delivered their second, third and more order births (US$82 and 62, respectively). Therefore, the reduction in the OOPE due to JSY was greater in the higher-order birth than in the lower-order birth. Nearly 60 % of the women who delivered their children in the hospital stayed for more than 48 h. Women who stayed for more than 48 h, 82 % of them delivered in public facilities. Increase stay in hospital also increased the expenditure on child birth. Those who stayed in public hospital for 48 h paid US$29 additional as compared to woman who stayed less than 48 h (US$59 vs. 88). This gap widened (US$82), when the delivery was conducted at private facility. The reduction in OOPE due to JSY was less among women staying for longer duration.
Table 5.
Place of delivery and expenditure by background characteristics. Percentage distribution of women by place of delivery, mean OOPE (in US$) and JSY incentive as percentage of total cost per delivery by background characteristics in Rajasthan, 2011
| Background characteristics | N | Percentage of women delivered at public facilities | Percentage of women delivered at private facilities | Expenditure during antenatal and natal care by place of delivery | ||||
|---|---|---|---|---|---|---|---|---|
| Public facility | OOPE in private facility | OOPE in home delivery | ||||||
| Total cost | Actual OOPE less of JSY incentives | Incentives as % of total cost | ||||||
| Age | ||||||||
| Less than 25 | 206 | 65.0 | 20.9 | 84 | 57 | 31.7 | 168 | 44 |
| 25 and above | 218 | 59.6 | 20.6 | 72 | 48 | 33.6 | 134 | 24 |
| Caste | ||||||||
| General | 62 | 54.8 | 35.5 | 116 | 82 | 28.8 | 177 | 32 |
| Others | 362 | 63.5 | 18.2 | 72 | 45 | 37.9 | 141 | 32 |
| Economic status | ||||||||
| BPL cardholder | 141 | 69.5 | 12.8 | 56 | 30 | 46.4 | 101 | 22 |
| APL | 283 | 58.7 | 24.7 | 91 | 61 | 32.4 | 163 | 38 |
| Type of family | ||||||||
| Nuclear | 111 | 55.8 | 15.3 | 92 | 63 | 31.5 | 162 | 24 |
| Joint/extended family | 313 | 64.6 | 22.7 | 74 | 46 | 38.0 | 147 | 39 |
| Literacy | ||||||||
| Illiterate | 234 | 64.9 | 12.4 | 68 | 42 | 38.6 | 134 | 26 |
| Literate | 190 | 59.0 | 31.1 | 91 | 60 | 33.8 | 158 | 35 |
| Work status | ||||||||
| Not working | 200 | 72.0 | 20.5 | 73 | 45 | 38.3 | 142 | 43 |
| Working | 224 | 53.6 | 21.0 | 71 | 55 | 22.8 | 157 | 23 |
| Husband’s literacy | ||||||||
| Illiterate | 84 | 60.7 | 14.3 | 48 | 23 | 51.3 | 117 | 24 |
| Literate | 340 | 62.6 | 22.3 | 85 | 56 | 34.1 | 155 | 36 |
| Birth order | ||||||||
| One | 140 | 66.5 | 22.9 | 92 | 61 | 33.2 | 165 | 50 |
| Two | 124 | 58.2 | 27.5 | 82 | 54 | 34.0 | 149 | 29 |
| Three and above | 160 | 61.9 | 13.8 | 62 | 36 | 42.2 | 149 | 27 |
| Place of ANCa | ||||||||
| Public facility | 182 | 75.9 | 7.1 | 59 | 34 | 42.4 | 97 | 21 |
| Private facilities | 87 | 40.3 | 38.0 | 107 | 76 | 29.7 | 183 | 32 |
| Both public and private facilities | 150 | 59.3 | 28.0 | 97 | 65 | 33.0 | 141 | 55 |
| Duration of stay in hospital after deliveryb | ||||||||
| Less than 48 h | 145 | 65.5 | 34.5 | 59 | 34 | 43.3 | 115 | NA |
| More than 48 h | 207 | 81.6 | 18.4 | 88 | 59 | 33.5 | 197 | NA |
| N | 424 | 279 | 145 | 264 | 264 | 264 | 88 | 72 |
aIncludes home deliveries
bOnly institutional deliveries
Determinant of OOPE
To understand the determinants of OOPE, a log linear regression model is used for all nonzero cases. Further log linear regression model is suitable for OOPE as the OOPE is skewed in nature. All variables except age and place of ANC (private) are significant in the model (Table 6). Educational attainment, duration of stay and complications are positively associated with OOPE. For example, with increase in educational attainment by 1 year, the OOPE is likely to increase by 2 %. The APL households are likely to incur 35 % more OOPE than BPL households. Those women experienced pregnancy complications are likely to spend 61 % more than normal deliveries. These results are in agreement with bivariate analyses and in expected direction. Those who received JSY were likely to spend 46 % less than those not under JSY categories. Similarly, those who had ANC at public hospital were less likely to spend more compared to others. The R2 value was .408 indicating that 41 % variation in the model is being explained. The F statistics (25.7) was significant, indicating the overall significance of the model.
Table 6.
Determinant of out-of-pocket expenditure (OOPE): dependent variable—log of out-of-pocket expenditure
| Independent variables | Unstandardized beta coefficients | Sig. | 95.0 % CI | |
|---|---|---|---|---|
| Lower limit | Upper limit | |||
| Age (in completed years) | −.010 | .477 | −.037 | .018 |
| Education (in completed years) | .020 | .047 | .000 | .041 |
| Birth order | −.084 | .214 | −.217 | .049 |
| Duration of stay in the hospital (in hr.) | .005 | .000 | .003 | .006 |
| Economic status of family (BPL®) | ||||
| APL | .353 | .001 | .149 | .557 |
| Complications during pregnancy/delivery (No®) | ||||
| Yes | .612 | .000 | .392 | .832 |
| Received JSY incentives (No®) | ||||
| Yes | −.458 | .000 | −.691 | −.225 |
| Place of ANC—public (No®) | ||||
| Yes | −.544 | .000 | −.753 | −.334 |
| Place of ANC—private (No®) | ||||
| Yes | .095 | .468 | −.160 | .351 |
| (Constant) | 7.833 | .000 | 7.127 | 8.538 |
Discussion
In India, enormous efforts were made by the government, nongovernmental organisations and bilateral and multi-lateral donors to increase the level of skilled birth attendance while launching or supporting dedicated policies and programmes since 1990s. In this series, National Rural Health Mission emerged as a milestone. About two third of national health budget is being spent on NRHM, and the NRHM is said to bring considerable changes in whole health care delivery system in India especially in reducing infant and maternal mortality. However, the national average conceals large disparities across the states and socio-economic group in the country. Numerous studies have shown the socio-economic inequality in the utilisation of health care services, and the increased services do not necessarily benefit the poor and marginalised. Prior to the launch of NRHM, empirical evidences and research studies suggest that the cost of the health care services was one of the major barriers for poor households to avail the services [30, 32, 59–62] especially for child bearing. After one decade of the implementation of NRHM, especially Janani Suraksha Yojana (JSY), the largest conditional cash transfer programme in the world [9], a phenomenal increase was observed in institutional deliveries across Indian states [38]. This study attempts to understand the OOPE by pattern of antenatal care and delivery care in post-NRHM period in the state of Rajasthan.
The following are the salient findings of this study. First, we found about three-fourth mothers received three and more antenatal care and nine out of ten women delivered in a health centre. This is significantly higher compared to 41 % coverage of three or more antenatal care and 32 % institutional delivery in Rajasthan in 2005–2006 [30]. It may be mentioned that majority of women in our sample were from scheduled caste and scheduled tribe. Hence, this is indicative that the NRHM may have resulted in positive effect on antenatal care and institutional delivery in the state of Rajasthan particularly among the poor and marginalised. The finding is in line with studies on the impact of JSY [44, 63, 64]. Second, we found varying OOPE on antenatal care by the type of provider. The mean OOPE of antenatal care among those availed from public health centre was US$26, US$64 from private health centres and US$49 for those who availed from both private and public health centres. This was higher than the cost of antenatal care in the state during pre-NRHM period [32] possibly due to increasing contact and awareness on institutionalised maternal care and the price effect. Third, half of the OOPE on antenatal care and delivery care was on medicines followed by sonography/test and transportation irrespective of type of service provider. Fourth, the JSY covered 77 % of the cost for normal delivery and 23 % of the cost of complicated delivery with an average of 44 %. This result of our study was higher than the study conducted by Gopalan et.al., where they mentioned that JSY covered 26 % of the maternal healthcare cost in rural areas [65]. The women, who suffered from complications during pregnancy and delivery, spent about three and a half times higher than those who had a normal delivery. The cost per complicated delivery was also significantly higher in African countries [46, 50].
The overall findings of the study suggest that JSY has been successful in reducing the OOPE of the beneficiaries opting for delivery at public health facility. Since the incentive was the highlight of the scheme, the increase in institutional deliveries could be attributed to the satisfaction with the incentives attached to the scheme [66]. Evidences support that incentives provided under JSY were able to meet the cost incurred by the family for the delivery to some extent. Therefore, the incentives worked in favour of institutional delivery addressing the financial barriers and enhancing utilisation of maternal care services in Rajasthan. Also, the NRHM strengthened the public health care system while addressing the other barriers for poor health care utilisation [67]. NRHM focused on the facilitating environment for safe motherhood, i.e., utmost care and attention provided to pregnant women and newborns by strong health care delivery system, i.e., availability of skilled health personnel, adequate health care facilities, equipment, medicines and emergency care along with the community mobilisation [67].
Conclusions
Based on the extent of antenatal and natal care coverage in our study, it is evident that most of the women were availing the services. Therefore, it can be said that the government’s intention to encourage mothers to deliver at a health facility by providing incentives along with improvement in health care system is reducing disparity and bringing women to the health care centre. Hence, the cash incentive should continue and extend to sonography/test during pregnancy period and complicated deliveries. Since complicated deliveries are largely carried out at private health centres, provisioning of financial incentive to complicated deliveries irrespective of the type of provider should be considered. The incentives have been able to substantially reduce the financial burden faced by the women who delivers at an institution. Last, the population based survey should not only collect the cost of delivery care but also cost of antenatal care.
Limitation of the study
The study followed a cross-sectional design due to limited resource and time. The study could not segregate the post-delivery care cost from child care cost, therefore addressed the expenditure related to prenatal and natal care.
Acknowledgements
We express our heartfelt thanks to express our gratitude to UNFPA, Bangkok, for funding the study; the officials at the Department of Health and Family Welfare, Rajasthan, for their support and co-operation in granting the permission to conduct the study in the State and providing relevant information. We are extremely grateful to our research staff Dr. Vrinda Mehra, Mr. Lalit Mohan Nayak and Dr. Sonia Luna for their assistant in collecting the data for the study.
Authors’ contributions
DG conceived and implemented (data collection) the study and drafted and finalised the manuscript. NP coordinated the research and helped in carrying out the data collection, analysis, and drafting of the manuscript. SDG participated in the design of the study, guided the whole process and edited the manuscript. SKM participated in the statistical analysis, sequence alignment and editing. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Xu L, Liu X, Sun X, Fang L, Hindle D. Maternal and infant health prepayment schemes in Shandong, China: a survey of demand and supply. Aust Health Rev. 2002;25(3):15–25. doi: 10.1071/AH020015. [DOI] [PubMed] [Google Scholar]
- 2.Ensor T, Clapham S, Prasad D. What drives health policy formulation: Insights from the Nepal maternity incentive scheme? Health Policy. 2009;90:247–53. doi: 10.1016/j.healthpol.2008.06.009. [DOI] [PubMed] [Google Scholar]
- 3.Urquieta J, Angeles G, Mroz T, Lamadrid-Figueroa H, Hernández B. Impact of oportunidades on skilled attendance at delivery in rural areas. Econ Dev Cult Change. 2009;57:539–58. doi: 10.1086/596598. [DOI] [Google Scholar]
- 4.Anastasia M. Bolivia tackles maternal and child deaths. Lancet. 2009;374:442. doi: 10.1016/S0140-6736(09)61438-0. [DOI] [PubMed] [Google Scholar]
- 5.Bhat R, Mavalanker DV, Singh PV, Singh N. Maternal healthcare financing: Gujarat’s Chiranjeevi scheme and its beneficiaries. J Health Popul Nutr. 2009;27(2):249–58. doi: 10.3329/jhpn.v27i2.3367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Morris SS. Conditional cash transfer programs and health. In: Adato M, Hoddinott J, editors. Conditional cash transfer in Latin America. Baltimore: The John Hopkins University Press; 2010. pp. 212–30. [Google Scholar]
- 7.Schmidt JO, Ensor T, Hossain A, Khan S. Vouchers as demand side financing instruments for health care: a review of the Bangladesh maternal voucher scheme. Health Policy. 2010;96(2):98–107. doi: 10.1016/j.healthpol.2010.01.008. [DOI] [PubMed] [Google Scholar]
- 8.Ir P, Horemans D, Souk N, Damme WV. Using targeted vouchers and health equity funds to improve access to skilled birth attendants for poor women: a case study in three rural districts in Cambodia. BMC Pregnancy Childbirth. 2010;10(1):1–11. doi: 10.1186/1471-2393-10-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lim SS, Dandona L, Hoisington JA, James SL, Hogan MC, Gakidou E. India’s Janani Suraksha Yojana, a conditional cash transfer programme to increase births in health facilities: an impact evaluation. Lancet. 2010;375(9730):2009–23. doi: 10.1016/S0140-6736(10)60744-1. [DOI] [PubMed] [Google Scholar]
- 10.de Brauw A, Peterman A. Can conditional cash transfers improve maternal health and birth outcomes? Evidence from El Salvador’s Comunidades Solidarias Rurales. IFPRI discussion paper no. 01080, International Food Policy Research Institute, Washington DC, 2011. p.12-17.
- 11.Ahmed S, Khan MM. A maternal health voucher scheme: what have we learned from the demand side financing scheme in Bangladesh? Health Policy Plan. 2011;26(1):25–32. doi: 10.1093/heapol/czq015. [DOI] [PubMed] [Google Scholar]
- 12.Sosa-Rubí SG, Walker D, Serván E, Bautista-Arredondo S. Learning effect of a conditional cash transfer programme on poor rural women’s selection of delivery care in Mexico. Health Policy Plan. 2011;26:496–507. doi: 10.1093/heapol/czq085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Agha S. Impact of a maternal health voucher scheme on institutional delivery among low income women in Pakistan. Reprod Health. 2011;8:10. doi: 10.1186/1742-4755-8-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Abuya T, Njuki R, Warren CE, Okal J, Obare F, Kanya L, et al. A policy analysis of the implementation of a reproductive health vouchers program in Kenya. BMC Public Health. 2012;12:540. doi: 10.1186/1471-2458-12-540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Randive B, Diwan V, De Costa A. India’s conditional cash transfer programme (the JSY) to promote institutional birth: is there an association between institutional birth proportion and maternal mortality? PLoS. 2013;8(6):e67452. doi: 10.1371/journal.pone.0067452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nguyen HTH, Hatt L, Islam M, Sloan NL, Chowdhury J, Schmidt J, et al. Encouraging maternal health service utilization: an evaluation of the Bangladesh voucher program. Soc Sci Med. 2014;74:989–96. doi: 10.1016/j.socscimed.2011.11.030. [DOI] [PubMed] [Google Scholar]
- 17.Poel EV, Flores G, Ir P, O’Donnell O, Doorslaer EV. Can vouchers deliver? An evaluation of subsidies for maternal health care in Cambodia. Bull World Health Organ. 2014;92(5):331–9. doi: 10.2471/BLT.13.129122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Arur A, Gitonga N, O’Hanlon B, Kundu F, Senkaali M, Ssemujju R. Insights from innovations: lessons from designing and implementing family planning/reproductive health voucher programs in Kenya and Uganda. Bethesda: Private Sector Partnerships-One project, Abt Associates Inc; 2009. pp. 23–38. [Google Scholar]
- 19.Grainger C. Lessons from sexual and reproductive health voucher program design and function: a comprehensive review. Int J Equity Health. 2014;13:33. doi: 10.1186/1475-9276-13-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lawn JE, Costello A, Mwansambo C, Osrin D. Countdown to 2015: will the Millennium Development Goal for child survival be met? Arch Dis Child. 2007;92:551–6. doi: 10.1136/adc.2006.099291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Houweling TAJ, Ronsmans C, Campbell OMR, Kunst AE. Huge poor-rich inequalities in maternity and child care in developing countries. Bull World Health Organ. 2007;85(10):745–54. doi: 10.2471/BLT.06.038588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Barros AJD, Ronsmans C, Axelson H, Loaiza E, Bertoldi AD, França GVA, et al. Equity in maternal, newborn, and child health interventions equity in maternal, newborn, and child health interventions in Countdown to 2015: a retrospective review of survey data from 54 countries. Lancet. 2012;379:1225–33. doi: 10.1016/S0140-6736(12)60113-5. [DOI] [PubMed] [Google Scholar]
- 23.United Nations . The millennium development goals report. New York: United Nations; 2014. pp. 4–5. [Google Scholar]
- 24.UNICEF . The situation of children in India: a profile. New Delhi: United Nations Children’s Fund (UNICEF); 2011. p. 3. [Google Scholar]
- 25.WHO, UNICEF, UNFPA, WB, UNDP . Trends in maternal mortality: 1990 to 2013. Geneva: World Health Organization; 2014. p. 21. [Google Scholar]
- 26.Say L, Raine R. A systematic review of inequalities in the use of maternal health care in developing countries: examining the scale of the problem and the importance of context. Bull World Health Organ. 2007;85(10):812–9. doi: 10.2471/BLT.06.035659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hatt L, Stanton C, Makowiecka K, Adisasmita A, Achadic E, Ronsmans C. Did the strategy of skilled attendance at birth reach the poor in Indonesia? Bull World Health Organ. 2007;85(10):774–83. doi: 10.2471/BLT.06.033472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mohanty SK, Pathak PK. Rich-poor gap in utilization of reproductive and child health care services in India, 1992-2005. J Biosoc Sci. 2009;41(3):381–98. doi: 10.1017/S002193200800309X. [DOI] [PubMed] [Google Scholar]
- 29.Balarajan Y, Selvaraj S, Subramanian SV. Health care and equity in India. Lancet. 2011;377(9764):505–15. doi: 10.1016/S0140-6736(10)61894-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.International Institute for Population Sciences and Macro International . National Family and Health Survey (NFHS 3) 2005-06—India. Mumbai: IIPS; 2007. p. 210. [Google Scholar]
- 31.Government of India. National Health Accounts Cell . National Health Accounts, India, 2004–05. New Delhi: Ministry of Health and Family Welfare, Government of India; 2009. p. 30. [Google Scholar]
- 32.Bonu S, Bhushan I, Rani M, Anderson I. Incidence and correlates of ‘catastrophic’ maternal health care expenditure in India. Health Plann Policy. 2009;24:445–56. doi: 10.1093/heapol/czp032. [DOI] [PubMed] [Google Scholar]
- 33.Skordis-Worrall J, Pace N, Bapat U, Das S, More NS, Joshi W, Pulkki-Brannstrom A, Osrin D. Maternal and neonatal health expenditure in Mumbai slum (India): a cross sectional study. BMC Public Health. 2011;11:150. doi: 10.1186/1471-2458-11-150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sengupta A, Nundy S. The private health sector in India is burgeoning, but at the cost of public health care. Br Med J. 2005;331:1157–8. doi: 10.1136/bmj.331.7526.1157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chatterjee P. How free healthcare became mired in corruption and murder in a key Indian state. Br Med J. 2012;344:e453. doi: 10.1136/bmj.e453. [DOI] [PubMed] [Google Scholar]
- 36.Chattopadhyay S. Corruption in healthcare and medicine: why should physicians and bioethicists care and what should they do? Indian J Med Ethics. 2013;10(3):153–9. doi: 10.20529/IJME.2013.049. [DOI] [PubMed] [Google Scholar]
- 37.Bajpai V. The challenges confronting public hospitals in India, their origins, and possible solutions. Advances in Public Health 2014; Article ID 898502. http://dx.doi.org/10.1155/2014/898502. Accessed 9 May 2016.
- 38.National Health Mission. Annual Report 2013-2014. Department of Health & Family Welfare, Ministry of Health & Family Welfare, Government of India. 2014; p.371. http://nrhm.gov.in/images/pdf/media/publication/Annual_Report-Mohfw.pdf. Accessed 10 May 2016.
- 39.Registrar General of India. SRS Bulletin. New Delhi, Vital Statistical Division, 2006; 41(1):1-6. ISSN 0971-3549. http://www.censusindia.gov.in/vital_statistics/SRS_Bulletins/SRS_Bulletins_links/SRS_Bulletin-October-2006.pdf. Accessed 10 May 2016.
- 40.Registrar General of India . Special bulletin on maternal mortality in India 2004-06. New Delhi: Vital Statistical Division; 2009. p. 3. [Google Scholar]
- 41.Registrar General of India . Maternal mortality ratio bulletin. Sample Registration System. New Delhi: Vital Statistical Division; 2014. [Google Scholar]
- 42.Khan ME, Hazra A, Bhatnagar I. Impact of Janani Suraksha Yojana on selected family health behaviour in rural Uttar Pradesh. J Fam Welf. 2010;56(Special Issue):9–22. [Google Scholar]
- 43.Dongre A. Effect of monetary incentives on institutional deliveries: evidence from the Janani Suraksha Yojana in India. Munich Personal RePEc Archive (MPRA), 2010; Paper No. 26339. https://mpra.ub.uni-muenchen.de/id/eprint/26339. Accessed on 10 May 2016.
- 44.United National Population Fund . Concurrent assessment of Janani Suraksha Yojana (JSY) in selected states Bihar, Madhya Pradesh, Orissa, Rajasthan, Uttar Pradesh. New Delhi: UNFPA; 2009. [Google Scholar]
- 45.Modugu HR, Kumar M, Kumar A, Millett C. State and socio-demographic group variation in out-of-pocket expenditure, borrowings and Janani Suraksha Yojana (JSY) programme use for birth deliveries in India. BMC Public Health. 2012;12:1048. doi: 10.1186/1471-2458-12-1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kowalewski M, Mujinja P, Jahn A. Can mother afford maternal health care costs? User costs of maternity services in rural Tanzania. Afr J Reprod Health. 2001;6(1):65–73. doi: 10.2307/3583147. [DOI] [PubMed] [Google Scholar]
- 47.Borghi J, Hanson K, Acquah CA, Ekanmian G, Filippi V, Ronsmans C, et al. Costs of near-miss obstetric complications for women and their families in Benin and Ghana. Health Policy Plan. 2003;18(4):383–90. doi: 10.1093/heapol/czg046. [DOI] [PubMed] [Google Scholar]
- 48.Mukherjee S, Singh A, Chandra R. Maternity or catastrophe: a study of household expenditure on maternal health care in India. Health. 2013;5(1):109–18. doi: 10.4236/health.2013.51015. [DOI] [Google Scholar]
- 49.Mohanty SK, Srivastava A. Cost and utilization of hospital based delivery care in Empowered Action Group (EAG) States of India. Matern Child Health J. 2013;17(8):1441–51. doi: 10.1007/s10995-012-1151-3. [DOI] [PubMed] [Google Scholar]
- 50.Perkins M, Brazier E, Themmen E, Bassane B, DjenebaDiallo D, Mutunga A, Mwakajonga T, Ngobola O. Out-of-pocket costs for facility-based maternity care in three African Countries. Health Policy Plan. 2009;24(4):289–300. doi: 10.1093/heapol/czp013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Douangvichit D, Liabsuetrakul T, McNeil E. Health care expenditure for hospital-based delivery care in Lao PDR. BMC Res Notes. 2012;5:30. doi: 10.1186/1756-0500-5-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Levin A, Dymatraczenko TT, McEuen M, Ssengooba F, Mangani R, Van Dyck G. Costs of maternal health care services in three Anglophone African Countries. Int J Health Plann Manag. 2003;18:3–22. doi: 10.1002/hpm.690. [DOI] [PubMed] [Google Scholar]
- 53.Borghi J, Sabina N, Blum LS, Hoque ME, Ronsmans C. Household costs of healthcare during pregnancy, delivery and the postpartum period: a case study from Matlab, Bangladesh. J Health Popul Nutr. 2006;24:446–55. [PMC free article] [PubMed] [Google Scholar]
- 54.Borghi J, Ensor T, Neupane BD, Tiwari S. Financial implications of skilled attendance at delivery in Nepal. Trop Med Int Health. 2006;11:228–37. doi: 10.1111/j.1365-3156.2005.01546.x. [DOI] [PubMed] [Google Scholar]
- 55.Tripathi N, Saini SK, Prinja S. Impact of Janani Shishu Suraksha Karyakram on out-of-pocket expenditure among urban slum dwellers in Northern India. Indian Pediatr. 2014;51:475–7. doi: 10.1007/s13312-014-0430-z. [DOI] [PubMed] [Google Scholar]
- 56.Khan SH. Free does not mean affordable: maternity patient expenditures in a public hospital in Bangladesh. Cost Eff Resour Alloc. 2005;3:1. doi: 10.1186/1478-7547-3-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Registrar General and Census Commissioner of India . Census of India, 2011, Provision Population Totals, Paper 1 of 2011. India: Government of India; 2011. [Google Scholar]
- 58.Reserve Bank of India . Handbook of statistics on Indian economy, 2011-12. Mumbai: Reserve Bank of India, Central Office Building; 2012. p. 236. [Google Scholar]
- 59.Kouyarw B, Flessa S. Catastrophic household expenditure for health care in low-income society: a study from Nouna District, Burkin Faso. Bull World Health Organ. 2006;84:21–7. doi: 10.2471/blt.05.023739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Agarwal S, Satyavada A, Kaushik S, Kumar R. Urbanization, urban poverty and health of the urban poor: status, challenges and the way forward. Demography India. 2007;36(1):121–34. [Google Scholar]
- 61.Simkhada B, Van Teijlingen ER, Porter M, Simkhada P. Factors affecting the utilization of antenatal care in developing countries: systematic review of the literature. J Adv Nurs. 2008;61(3):244–60. doi: 10.1111/j.1365-2648.2007.04532.x. [DOI] [PubMed] [Google Scholar]
- 62.International Institute for Population Sciences . District level household and facility survey (DLHS-3), 2007-08. India: International Institute for Population Sciences, Ministry of Health and Family Welfare Government of India; 2010. pp. 74–5. [Google Scholar]
- 63.Powell-Jacksona T, Mazumdar S, Mills A. Financial incentives in health: new evidence from India’s Janani Suraksha Yojana. J Health Econ. 2015;43:154–69. doi: 10.1016/j.jhealeco.2015.07.001. [DOI] [PubMed] [Google Scholar]
- 64.Gupta SK, Pal DK, Tiwari R, Garg R, Shrivastava AK, Sarawagi R, Patil R, Agarwal L, Gupta P, Lahariya C. Impact of Janani Suraksha Yojana on institutional delivery rate and maternal morbidity and mortality: an observational study in India. J Health Popul Nutr. 2012;30(4):464–71. doi: 10.3329/jhpn.v30i4.13416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Gopalan SS, Varatharajan D. Addressing maternal healthcare through demand side financial incentives: experience of Janani Suraksha Yojana program in India. BMC Health Serv Res. 2012;12:319. doi: 10.1186/1472-6963-12-319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Mohanty SK, Srivastava A. Out-of-pocket (OOP) expenditure on institutional delivery in India. Health Policy and Plan. 2012;28(3):247–62. doi: 10.1093/heapol/czs057. [DOI] [PubMed] [Google Scholar]
- 67.Government of India. Report of the working group on National Rural Health Mission (NRHM) for the twelfth five year plan (2012-2017), WG1: progress and performance of National Rural Health Mission (NRHM) and suggestions 2011; No. 2(6)2010-H&FW, Planning Commission, GoI. http://planningcommission.nic.in/aboutus/committee/wrkgrp12/health/WG_1NRHM.pdf


