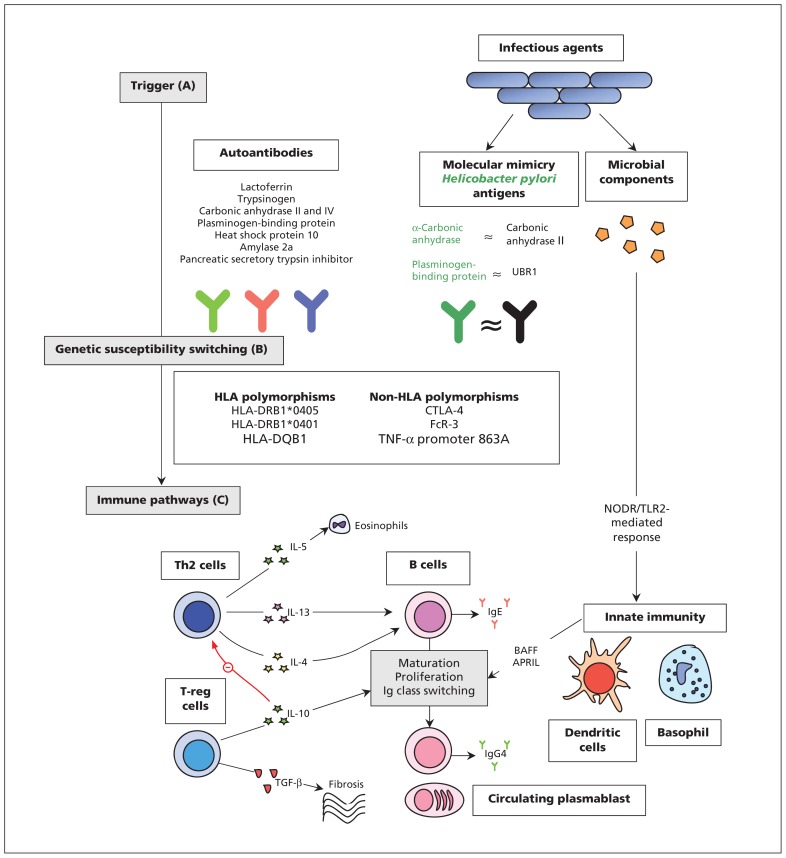
Figure 1:
Mechanisms of pathogenesis for IgG4-related disease. (A) Antibodies versus antigens commonly found in exocrine organs may drive Th2-cell response. Most have only been investigated in type 1 AIP, are nonspecific, and none have been consistently found in active disease.16–18 Molecular mimicry of Helicobacter pylori antigens with human counterparts may be a trigger for type 1 AIP.19,20 Microbial components may stimulate innate immune mechanisms by activating NODR and TLR2 to produce BAFF and APRIL which lead to changes to B cells in a T cell–independent manner.21 (B) Polymorphisms of both HLA and non-HLA antigens have been implicated in the development of type 1 AIP.15 (C) A dominant Th2-cell (and associated cytokine) response occurs systemically and within affected organs. An expansion in T-reg cells may contribute to both B-cell Ig class switching and fibrosis.22 A treatment-sensitive expansion in circulating plasmablasts is present in active disease,23 although their exact role in pathogenesis remains unclear. Elevated levels of IgG4 in serum is a hallmark of the disease and is a consequence of a modified Th2-cell response.15 Note: AIP = autoimmune pancreatitis, APRIL = a proliferation-inducing ligand, BAFF = B cell–activating factor belonging to the TNF family, B cell = beta cell, HLA = human leucocyte antigens, Ig = immunoglobulin, NODR = nucleotide-binding oligomerization domain receptor, T cell = T lymphocyte cell, TGF = transforming growth factor, Th2 = type 2 T helper, TLR2 = toll-like receptor 2, T-reg = regulatory T cell, TNF = tumour necrosis factor, UBR1 = ubiquitin-protein ligase E3 component n-recognin 1.