Abstract
Breast cancer is the leading cause of cancer death among Hispanic women. Certain dietary factors have been associated with the risk of breast cancer recurrence, but data in Hispanic survivors is scarce.
Objective
to examine dietary patterns and diet quality in two groups of Hispanic breast cancer survivors.
Methods
23 Mexican American (MA) and 22 Puerto Rican (PR) female breast cancer survivors completed a culturally adapted validated food frequency questionnaire. Intake was standardized per 1,000 kcal and compared to US Dietary Guidelines and the DASH-style diet adherence score was calculated.
Results
Overweight/obese was 70% in MA and 91% in PR. PR consumed diets rich in fruit/100% fruit juices and beans, while MA diets were high in vegetables, beans, and total grains. Both groups consumed high amounts of starchy vegetables, refined grains, animal protein and calories from solid fats and added sugars but low intakes of whole grains, dairy products and nuts and seeds. DASH scores were relatively low.
Conclusion
MA and PR female breast cancer survivors have different dietary patterns but both groups had relatively low diet quality. These groups could benefit from culturally tailored interventions to improve diet quality, which could potentially reduce cancer recurrence.
Keywords: Dietary patterns, DASH-style diet, breast cancer survivors, Puerto Ricans, Mexican Americans
INTRODUCTION
Breast cancer is one of the leading causes of morbidity and mortality in the world. Breast cancer survivors comprise the largest group of cancer survivors in the US, with an estimated 2.8 million survivors (1). Breast cancer is the leading cause of cancer death among Hispanic women, the second largest race/ethnic group in the US (2). Even though the breast cancer prevalence is lower in Hispanics compared to non-Hispanic whites, Hispanic women are more likely to die from breast cancer than non-Hispanic whites (3), which could be related to differences in access to treatment and preventive screening. In Puerto Rico, breast cancer accounts for 34% of cancers (4). In the US, breast cancer accounts for 28% of cancers in Hispanics (5), of which most are Mexican Americans.
Certain dietary factors have been associated with a decreased risk of breast cancer recurrence. These include diets low in fat but high in fruits, vegetables and soy based foods (6, 7). On the contrary, diets high in alcohol intake and fat dairy products increases the risk of recurrence (8, 9). Interventions to encourage a high quality dietary pattern should be studied in breast cancer survivors. However, current eating patterns in Hispanic breast cancer survivors require investigation in order to appropriately adapt dietary interventions for this population.
Within the Hispanic ethnicity, there are differences in race, country of origin, levels of acculturation, English language proficiency, foods preferences, etc., all of which interact with parameters that affect health behaviors, including dietary patterns. Data from the Hispanic Community Health Study/Study of Latinos, a population-based cohort study of Hispanic/Latino adults of diverse backgrounds showed a large variation in dietary patterns between the group studied, which included Mexican Americans, Puerto Ricans, Dominicans, Cubans, Central Americans and South Americans (10). For example, this study found the lowest fruit intake among Puerto Ricans and the highest among Dominicans and the lowest vegetable intake among Dominicans and the highest intake among Mexicans Americans.
Thus, it is important to study how dietary patterns differ between and within specific ethnic populations so that culturally relevant behavioral interventions to improve dietary patterns can be developed. However, little is known about dietary patterns among the different Hispanic groups of breast cancer survivors. Therefore, the aims of this study were to examine the dietary patterns (fruits, vegetables, meats, water, sugary beverages, fats, refined and whole grains, dairy products, seeds and nuts, alcohol and diet quality) in two groups of Hispanic breast cancer survivors, Mexicans-Americans and Puerto Ricans. Results from this study could increase our understanding of the dietary patterns in this group of at-risk women.
METHODS
Study design
We report on dietary intake from women who participated in Project VIVA!, a randomized controlled trial designed to pilot test the effectiveness and feasibility of a 16-week culturally tailored exercise intervention for sedentary Mexican American and Puerto Rican breast cancer survivors. The study was conducted in two sites: The University of Texas MD Anderson Cancer Center in Houston, Texas and The University of Puerto Rico Cancer Center in San Juan, Puerto Rico. Participants were randomized to a 16-week culturally-adapted exercise program, a non-culturally adapted standard exercise intervention or a wait-list control group. At the end of the trial, participants completed a culturally adapted and validated food frequency questionnaire (FFQ).
The study was reviewed and approved by an institutional review board at both sites and all participants provided consent to participate.
Participants
Eligibility criteria of the main study were: 21 years of age or older; self-reported Mexican American or Puerto-Rican; at least 3 months post-treatment of breast cancer; not meeting the American College of Sports Medicine guidelines for physical activity (11), not taking cancer treatment medications (except hormonal therapy) and having completed the FFQ.
Study procedures and measures
Demographics and health
A short demographic survey was administered to participants at baseline only. Information on age, race and ethnicity, educational level, household income, medical history and current medications were collected. Physical activity and sedentary time in the past seven days was assessed using the short version of the International Physical Activity Questionnaire at 16 weeks.
Body composition
Height (m) and weight (kg) were measured following standard procedures (12). Participants were classified as healthy weight if BMI was <25 kg/m2; overweight if BMI was 25-29.9 kg/m2 and obese if BMI was ≥30 kg/m2.
Food Frequency Questionnaire (FFQ)
A culturally adapted and validated FFQ was administered at the end of the 16 weeks. Interviewers were trained under the same protocol procedures to conduct thorough and comparable dietary assessment interviews at both sites (using the same prompts, portion models, etc.).
For the Puerto Rican site, a semi-quantitative FFQ developed for Puerto Ricans living in Boston, Massachusetts (13) and further adapted and validated for Puerto Ricans living in Puerto Rico (14) was used. The FFQ has 193 items with their frequency of consumption in the last 12 months and portion size for some of the items. For certain items, participants were asked if the food was “regular” or “whole grain” or if it was “regular”, “reduced sugar/fat” or “without sugar/fat”. Summary questions were also included at the end of each section and at the end of the FFQ on the use of salt at the table, most often used fat in cooking, frequency of dining out, and the usual meal location. Open-ended questions were included for participants to specify the breakfast cereals and the type of breads most frequently consumed, and to specify frequently consumed foods not included on the FFQ. Finally, it included a section on supplement use. The FFQ was interviewer-administered by phone or in person. To help participants estimate the portion sizes, a portion size booklet was sent by mail prior to the call. This booklet contained black and white drawings of actual serving portions, including images of spoons, bowls, cups, and serving sizes, of the foods included in the FFQ. Nutrient profiles and food groups intakes (servings) were calculated with the Nutrition Data System for Research (NDSR, program 2.8, version 25, University of Minnesota, Minneapolis, MN). Intake of food groups were transformed from servings to MyPyramid Equivalents when necessary.
For Mexican-Americans, the FFQ used was a version of the National Cancer Institute Block Health Habits and History Questionnaire (15) further modified to include commonly consumed ethnic foods that are major contributors to nutrient intake in Texas (16). The FFQ queries the frequency of consumption of 170 items over the last 12 months and includes a section on supplements. The FFQ was interviewed-administered with portion size models (measuring cups and spoons, and 8 and 12 oz Styrofoam cups). The questionnaire first included questions on recent diet changes (if they were on a special diet in the last year) and general queries on how often they consumed fruits, vegetables, cold cereals, milk, and fats typically used in cooking. For each item, the medium portion size was presented and participants were asked to select if their usual portion size was small, medium (the reference provided), large or extra-large (for certain items). In addition, for certain items, participants were asked if it was regular, reduced or without fat. For orange juice, participants were asked if it was fortified with calcium. An open-ended question was included at the end for participants to specify any frequently consumed foods not included in the FFQ. The frequency and portion size of each food item was integrated into MyPyramid Equivalents Database, 2.0 for USDA Survey Foods, 2003–2004 (MPED 2.0), which calculates the cup/ounce equivalent for each ingredient and assigns components to food groups, based on MyPyramid (17).
Although the two FFQs contain different queries for some of the individual food items, we used uniform standard methods (described above) to create comparable food groups (e.g., fruits, vegetables, dairy) from these items. Thus while the list of food items within each food group may be slightly different between the two sites, both FFQs had been validated for total energy intake and they both represented the whole diet for each group. Therefore, when adjusted for total energy intake (by site/FFQ instrument), they are considered comparable for derived food groups.
Food group intake and diet quality assessment
Intake of nutrients and food groups from the FFQs were adjusted for 1,000 kcals for all participants. Key nutrients, including energy intake, macronutrients and micronutrients, were compared between these two groups. Intake of food groups was also compared between the 2 groups. In addition, we also compared intake from both groups to the US Dietary Guidelines, which recommends a number of portions from each food groups for the general population. Also, we compared percent calories from protein, carbohydrate and fat to the recommended ranges as reported by the Acceptable Macronutrient Distribution Ranges (AMDR) (18). Lastly, we calculated the Dietary Approach to Stop Hypertension (DASH)-style diet adherence score (19). Although the DASH diet was originally designed to lower blood pressure, the objectives of this diet (increasing fruits, vegetables, whole grains, low fat dairy, leans meats and fishes, nuts, seeds, and legumes; and reducing saturated fats, sweetened beverages and sodium) are relevant to health outcomes in overweight/obese breast cancer survivors. As mentioned previously, diets high in fruits and vegetables and low in fat have been associated with a decreased risk of breast cancer recurrence (6, 7). Studies using the DASH diet score have found an inverse association between a high score and the risk of obesity, cardiovascular diseases, diabetes mellitus and cancer (19-21) in different populations, including Hispanics (22).
Briefly, this scores ranks intake from 8 key diet components: fruits, vegetables, nuts and legumes, lowfat dairy products, whole grains, sodium, red and processed meats, and sugar sweetened beverages (19). Women are classified into quintiles according to their intake ranking. For the first 5 components (fruits, vegetables, nuts and legumes, low-fat dairy products, whole grains) a score of 5 is given for those classified into quintile 5 while a score of 1 is given to those classified into quintile. 1. For sodium, red and processed meats, and sugar sweetened beverages, a reversed score is used, as low intake of those foods is desirable. Therefore, those classified in quintile 1 are assigned a score of 5 points while those classified in quintile 5 are assigned a score of 1 point. The component scores are then added to obtain an overall DASH-style diet adherence score ranging from 8 to 40.
Statistical Analyses
Mean and standard errors were computed for continuous variables and frequencies for categorical values. Socio-demographic characteristics were compared among Puerto Ricans and Mexican-Americans using a two-tailed T-test or Fisher's exact test, when appropriate. Intake of macronutrients and food groups were compared among Puerto Ricans and Mexican-Americans using Analysis of Variance (ANOVA), adjusting for age (significant variable between groups) and for energy intake as continuous variables. DASH-style diet adherence score was categorized into tertiles and compared by BMI groups and also by exercise treatment groups using ANOVA and ANCOVA. All analyses were performed using Microsoft Excel (2007, Microsoft) and the SAS software (Version 9.2, SAS Institute, Cary, NC). Statistical significance was set at P<0.05.
Results
A total of 22 Puerto Rican and 23 Mexican American female breast-cancer survivors completed the FFQ at the end of the parent study. Table 1 shows the socio-demographic characteristics of these groups. Puerto Rican women sampled tended to be older than the Mexican American women (p<0.05). Most Puerto Rican and Mexican American women had some college or a college degree (54.5 and 56.6%, respectively) and most were married (45.5% and 60.9%, respectively; p>0.05). More Puerto Rican women were overweight/obese (90.9%) as compared to Mexican American women (69.5%), but this difference was not statistically significant (p>0.05).
Table 1.
Socio-Demographic characteristics of Hispanic breast cancer survivor women
| Variable | Hispanic – Puerto Ricans N=22 | Hispanic – Mexican Americans N=23 |
|---|---|---|
| Age (y) | 59.1±9.3 | 48.7±9.9* |
| Education (%) | ||
| ≤ High school | 45.5% | 43.5% |
| Some college or college degree | 54.5% | 56.5% |
| Marital status (%) | ||
| Single | 18.2% | 21.7% |
| Married | 45.5% | 60.9% |
| Separated/divorced | 13.6% | 13.0% |
| Widowed | 22.7% | 4.30% |
| Category of BMI (%) | ||
| Healthy weight | 9.10% | 30.4% |
| Overweight | 50.0% | 21.7% |
| Obese | 40.9% | 47.8% |
| Physical activity (vigorous and moderate minutes per week) | 39.1±82.4 | 117±169* |
| Smoked > 100 cigarettes in life | 13.6% | 30.4% |
Significantly different from Puerto Ricans at p<0.05 by T-test
Table 2 shows energy and macronutrient intake in the sample. Energy intake was similar between groups. Puerto Rican women had higher proportion of calories from fat, saturated fatty acids, monounsaturated fatty acids and polyunsaturated fatty acids but lower proportion of calories from carbohydrate and less fiber intake compared to Mexican American women. Compared to the recommendations, calories from protein and carbohydrate were within the AMDR in both groups, while calories from fat and saturated fatty acids were above the recommended levels in Puerto Ricans. Fiber intake was half of the recommended level in Puerto Ricans but on target in Mexican Americans.
Table 2.
Energy and macronutrient intakes in Hispanic breast cancer survivors
| Nutrients | Hispanic – Puerto Ricans | Hispanic – Mexican Americans | Dietary reference intakes1 | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | EAR/ AMDR | |
| Energy (kcal) | 1884 ± 621 | 2397 ± 1331 | - | ||
| Calories from protein (%) | 15.6 ± 3.05 | 15.8 ± 3.07 | 10-35% | ||
| Calories from carbohydrate (%) | 46.4 ± 8.91 | 56.8 ± 8.92* | 45-65% | ||
| Calories from fat (%) | 37.5 ± 6.94 | 30.3 ± 6.95* | 25-35% | ||
| Saturated fatty acids (%) | 12.4 ± 3.19 | 9.3 ± 3.21* | 10% | ||
| Monounsaturated fatty acids (%) | 14.5 ± 3.10 | 11.2 ± 3.12* | 10-25% | ||
| Polyunsaturated fatty acids (%) | 8 ± 1.97 | 6.5 ± 1.97* | 10-25% | ||
| Total Dietary Fiber (g/1000 kcal)2 | 7.4 ± 4.22 | 17.8 ± 4.22* | 14 g/1000 kcal | ||
Recommendation for total protein, carbohydrate and fat are expressed as percent calories from the Acceptable Macronutrient Distribution Ranges (AMDR). EAR: Estimated Adequate Requirements.
Mean fiber intake is adjusted for age and energy.
Significantly different from Puerto Ricans at p<0.05 by ANCOVA.
Table 3 shows food groups intake in the sample adjusted for age and energy intake. Mexican American women had higher intake of fruits, total vegetables, total grains, whole grains, added fat, and calories from solid fats and added sugars compared to Puerto Rican women (p<0.05). However, Puerto Rican women had higher intakes of starchy vegetables and added sugar compared to Mexican Americans (p<0.05). Compared to general recommendations, Puerto Ricans had intakes similar to the recommended levels for fruit and 100% fruit juices and beans while Mexican Americans had intakes similar to the recommended levels for vegetables, beans, and total grains. Both groups had intakes greater than recommended levels for starchy vegetables, refined grains, foods from the protein group and calories from solid fats and added sugars, while consumption of whole grains, dairy products and nuts and seeds were well below recommended levels for both groups. In addition, Mexican Americans had intakes well above the recommendations from fruits, which also includes 100% fruit juices.
Table 3.
Food groups intake in Hispanic breast cancer survivors1
| Food group intake (servings) | Unit | Hispanic – Puerto Ricans | Hispanic – Mexican Americans1 | US Dietary Guidelines per 1,000 kcal | ||
|---|---|---|---|---|---|---|
| Mean1 | SD | Mean1 | SD | |||
| Fruits/100% juices | cup | 1.08 ± 1.78 | 2.97 ± 1.77* | 1 cup/d | ||
| Total vegetables | cup | 0.65 ± 1.03 | 2.76 ± 1.06* | 1 cup/d | ||
| Starchy vegetables | cup/wk | 4.62 ± 1.64 | 2.8 ± 1.68 | 2 cups/wk | ||
| Beans | cup/wk | 3.43 ± 2.63 | 2.87 ± 2.69 | ½ cup/wk | ||
| Total grains | oz | 2.01 ± 0.98 | 3.13 ± 1.01* | 3 oz-eq | ||
| Whole grains | oz | 0.16 ± 0.33 | 0.6 ± 0.34* | 1½ oz-eq | ||
| Refined grains | oz | 1.85 ± 0.98 | 2.53 ± 0.96 | 1½ oz-eq | ||
| Red meat including pork | oz | 0.64 ± 0.56 | 0.91 ± 0.58 | |||
| Chicken | oz | 0.93 ± 0.38 | 0.42 ± 0.38 | 2 oz-eq | ||
| Fish | oz | 0.4 ± 0.38 | 0.41 ± 0.38 | |||
| Cold meats | oz | 0.38 ± 0.33 | 0.18 ± 0.34 | |||
| Eggs | oz | 0.31 ± 0.19 | 0.23 ± 0.19 | |||
| Nuts/seeds | oz/wk | 0.49 ± 0.66 | 0.56 ± 0.67 | 6 oz-eq/wk | ||
| Dairy products | cup | 1.15 ± 0.70 | 0.74 ± 0.72 | 2 cups/d | ||
| Alcohol | # | 0.18 ± 0.28 | 0.06 ± 0.29 | - | ||
| Added fat | gr | 16.7 ± 6.85 | 26.8 ± 6.86* | - | ||
| Added sugar | tsp | 9.9 ± 5.58 | 4.55 ± 5.61 | - | ||
| Estimated SoFAS | calories (%) | 300 (30%) | 322 (32%)* | 137 (14%) | ||
Means are age- and energy- adjusted for 1,000 kcal/d.
SoFAS: calories from solid fats and added sugars
Significant difference from Puerto Ricans at p<0.05 by ANCOVA.
Table 4 shows the DASH-style diet adherence score in the sample. This was calculated separately for each group. The total DASH-style diet adherence score for Puerto Ricans is 23.9 and for Mexican Americans is 24.0 out of a total of 40 points. In general, mean servings of each food group were higher in Mexican Americans. Daily sugar sweetened beverage (SSB) intake was particularly high in Puerto Ricans, averaging 1.6 servings/d compared to approximately 0.36 servings in Mexican Americans (p<0.01).
Table 4.
DASH-style diet adherence score in Hispanic breast cancer survivors1
| Dash Score component | Unit | Hispanic – Puerto Ricans | Hispanic – Mexican Americans | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Fruits | servings | 0.60 ± 0.61 | 1.42 ± 1.00* | ||
| Vegetables | servings | 0.40 ± 0.20 | 1.31 ± 0.68* | ||
| Nuts and legumes | servings | 0.28 ± 0.13 | 2.03 ± 1.83* | ||
| Whole grains | servings | 0.23 ± 0.23 | 0.54 ± 0.35* | ||
| Low-fat dairy | servings | 0.54 ± 0.41 | 0.39 ± 0.68 | ||
| Sodium | mg | 1989 ± 398 | 1400 ± 302* | ||
| Red and processed meats | servings | 0.61 ± 0.47 | 0.33 ± 0.35* | ||
| Sugar sweetened beverages | servings | 1.61 ± 1.02 | 0.36 ± 0.61* | ||
| Total score | points | 23.9 ± 4.34 | 24.0 ± 3.84 | ||
Adjusted for 1,000 kcal/d.
Significantly different from Puerto Ricans at p<0.05 by T-test
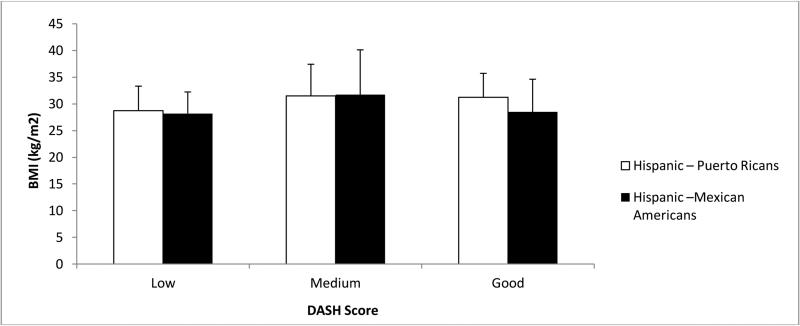
DASH-style diet adherence score tertiles, classified as low (≤22 points), medium (23-25 points) and high (≥26) score by BMI groups are shown in Figure 1. BMI was similar among the three groups (p>0.05). Also, DASH-style diet adherence score tertiles were compared among the three exercise treatment groups, with no differences among the groups (data not shown).
Figure 1. BMI by tertiles of total DASH score in the sample.
No significant differences in BMI by tertiles using ANOVA (p>0.05)
Discussion
In this pilot study, Puerto Rican and Mexican American female breast cancer survivors demonstrated different dietary patterns. Puerto Ricans consumed diets low in fiber and rich in fruit/100% fruit juices and beans, while Mexican Americans consumed diets rich in vegetables, beans, and total grains. Both groups consumed high amounts of starchy vegetables, refined grains, animal protein and calories from solid fats and added sugars but low intakes of whole grains, dairy products and nuts and seeds. Compared to the recommendations, both groups had low intakes of whole grains, dairy products and nuts and seeds and high intakes of starchy vegetables, refined grains, foods from the protein group, particularly red meat, and calories from solid fats and added sugars. Adherence to the DASH-style diet, which emphasizes the intake of plant proteins, fruits and vegetables, moderate amounts of low-fat dairy products, and low amounts of sweets and sodium, was somewhat low and not related to weight status.
These dietary patterns are consistent with those found in other studies in Puerto Rican and Mexican American individuals. Data from the Hispanic Community Health Study/Study of Latinos also reported different dietary patterns among these groups (10). Puerto Ricans had the lowest intake of fruits (1.4 servings/d), vegetables (2.5 servings/d) and fish (0.5 servings/d) and highest intake of sugar-sweetened beverages (1.8 servings/d) compared to the other groups. In addition, intake of whole grains was rather low (0.8 servings/d) compared to refined grains (5.6 servings/d) as well as dairy intake (1.6 servings/d). In Mexican Americans, intake of fruits (1.9 servings/d), vegetables (3.4 servings/d), and whole grains (2.8 servings/d) were higher, intake of dairy products (1.7 servings/d) was similar and intake of sweetened beverages (1.5 servings/day) was lower compared to Puerto Ricans. These results are consistent with what we found in the present study. In addition, baseline data from 3,088 breast cancer survivors in the Women's Healthy Eating and Living study, which included a mix of Hispanics from Mexico, the Caribbean, Central and South America, found similar intakes of fruits (2.7 servings/d) and vegetables (2.7 servings/d) (23) compared to the Mexican Americans in the present study.
The findings of the present study have important implications for developing interventions for Puerto Rican and Mexican American breast cancer survivors. Based on our results, diet quality in general needs improvement, specifically targeting strategies to increase intake of vegetables and whole grains, particularly in Puerto Ricans, increase intake of low-fat dairy products and reduce intake of red meat, added sugars and added fats, such as sugar sweetened beverages and fat used for cooking, particularly those high in saturated fat. This could potentially reduce breast cancer recurrence in these populations as evidenced by the few studies examining the relation between foods and dietary patterns and breast cancer recurrence (24-26). In 2522 postmenopausal breast cancer German women, consumption of a healthy dietary pattern (high intake of vegetables, fruits, vegetable oils, sauces/condiments, and soups/bouillons) lowered the risk of breast cancer recurrence (HR, 0.71; 95% CI, 0.48–1.06; P-trend <0.02). Although data from the Nurses’ Health Study in 86,621 women showed that a high adherence to the DASH style diet significantly decreased the risk of breast cancer (RR= 0.80, 95% CI: 0.64, 1.01; P trend = 0.02) (25) it was not significantly associated with breast cancer recurrence or mortality (26). Also, a high vegetable intake has been shown to decrease breast cancer recurrence (HR for highest vs lowest tertiles: 0.69, 95% CI 0.55-0.87) (27) while a high-fat dairy intake has been positively associated with breast cancer recurrence (8) in other cohorts. More research is needed to identify other dietary patterns that could decrease or increase breast cancer recurrence in specific populations, as scant data is available.
Some of the limitations of the study included the small sample size. Physical activity differed dramatically between the groups, being much higher in Mexican Americans compared to Puerto Ricans, but at the same time so did smoking habits, which were higher in the former; these different lifestyles could likely impact both diet quality and BMI. Due to the small sample size, we were not able to adjust for all the confounding factors in our analyses. Other limitations include the cross-sectional nature of the study, lack of data about income and differences in the questions included in the FFQs and their comparability. Also, the FFQs were completed after participants completed a 16-week exercise intervention; therefore, results are not generalized to all Puerto Rican and Mexican American breast cancer survivor. However, one of the strengths was the use of validated instruments for each ethnic group, which is important to capture the dietary patterns characteristic of each group. This study is highly unique, filling a critical gap towards designing effective interventions to reduce breast cancer recurrence in these at-risk groups.
In this sample of Puerto Rican and Mexican American breast cancer survivors, dietary patterns were characterized by low intakes of vegetables, whole grains (only in Puerto Ricans), low fat dairy products, and nuts and seeds and high intakes of starchy vegetables, sugar sweetened beverages, animal protein (red meat) and calories from added sugars and fats, particularly in Puerto Ricans. Overall diet quality assessed by DASH score was somewhat low in both group and was not related to weight status. These results could help design interventions specifically targeted to these groups to improve overall diet quality by reducing consumption of red meats, refined grains and calories from added sugars and fats and to increase intake of vegetables, low fat dairy products and whole grains. These interventions could potentially reduce breast cancer recurrence in the future in these groups.
Acknowledgements
This project was partially supported by the following NIH awards U54 CA 96297; P30 CA016672; NCR (2G12-RR003051), NIMHHD (5G12-MD007600-29), and the Center for Energy Balance in Cancer Prevention and Survivorship, Duncan Family Institute. The authors wish to acknowledge Janice Maras and Gladys Browman for their assistance with the dietary analysis.
Author's role: MTG and KBE designed study; VGM, LV and JL conducted research; CP conducted analysis and prepared manuscript; KBE, CRD and DCH provided critical review of the manuscript.
Footnotes
All authors have read and approved the submission of the manuscript; the manuscript has not been published and is not being considered for publication elsewhere, in whole or in part, in any language, except as an abstract. The authors have no conflict of interest.
ClinicalTrials.gov Identifier: NCT01504789
References
- 1.American Cancer Society [September 1, 2014];Cancer Facts & Figures 2014. Available at: http://www.cancer.org/research/cancerfactsstatistics/cancerfactsfigures2014/.
- 2.US Census Bureau Hispanic Heritage Month 2015. Available at: https://www.census.gov/newsroom/facts-for-features/2015/cb15-ff18.html. 2015.
- 3.Ooi SL, Martinez ME, Li CI. Disparities in breast cancer characteristics and outcomes by race/ethnicity. Breast Cancer Res Treat. 2011;127:729–738. doi: 10.1007/s10549-010-1191-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Puerto Rico Central Registry . Puerto Rico cancer incidence file. Division of Epidemiology, Puerto Rico Department of Health; 2008. [Google Scholar]
- 5.American Cancer Society [November 1, 2014];Cancer Facts & Figures for Hispanics/Latinos 2012-2014. Available at: http://www.cancer.org/acs/groups/content/@epidemiologysurveilance/documents/document/acspc-034778.pdf.
- 6.Chlebowski RT, Rose D, Buzzard IM, et al. Adjuvant dietary fat intake reduction in postmenopausal breast cancer patient management. The women's intervention nutrition study (WINS). Breast Cancer Res Treat. 1992;20:73–84. doi: 10.1007/BF01834637. [DOI] [PubMed] [Google Scholar]
- 7.Chi F, Wu R, Zeng YC, et al. Post-diagnosis soy food intake and breast cancer survival: A meta-analysis of cohort studies. Asian Pac J Cancer Prev. 2013;14:2407–2412. doi: 10.7314/apjcp.2013.14.4.2407. [DOI] [PubMed] [Google Scholar]
- 8.Kroenke CH, Kwan ML, Sweeney C, et al. J. High- and low-fat dairy intake, recurrence, and mortality after breast cancer diagnosis. J Natl Cancer Inst. 2013;105:616–623. doi: 10.1093/jnci/djt027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kwan ML, Kushi LH, Weltzien E, Tam EK, et al. Alcohol consumption and breast cancer recurrence and survival among women with early-stage breast cancer: The life after cancer epidemiology study. J Clin Oncol. 2010;28:4410–4416. doi: 10.1200/JCO.2010.29.2730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Siega-Riz AM, Sotres-Alvarez D, Ayala GX, et al. Food-group and nutrient-density intakes by Hispanic and Latino backgrounds in the Hispanic Community Health Study/Study of Latinos. Am J Clin Nutr. 2014;99:1487–1498. doi: 10.3945/ajcn.113.082685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Haskell WL, Lee IM, Pate RR, et al. Physical activity and public health: Updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39:1423–1434. doi: 10.1249/mss.0b013e3180616b27. [DOI] [PubMed] [Google Scholar]
- 12.Haff G, Dumke C. [September 29, 2014];Laboratory Manual for Exercise Physiology eBook With Web Resource. Available at: http://www.humankinetics.com/products/all-products/laboratory-manual-for-exercise-physiology-ebook-wweb-resource.
- 13.Tucker KL, Bianchi LA, Maras J, et al. Adaptation of a food frequency questionnaire to assess diets of Puerto Rican and non-Hispanic adults. Am J Epidemiol. 1998;148:507–518. doi: 10.1093/oxfordjournals.aje.a009676. [DOI] [PubMed] [Google Scholar]
- 14.Palacios C, Trak MA, Betancourt J, et al. Validation and reproducibility of a semi-quantitative FFQ as a measure of dietary intake in adults from Puerto Rico. Public Health Nutr. 2015;18:2550–8. doi: 10.1017/S1368980014003218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Block G, Hartman AM, Dresser CM, et al. A data-based approach to diet questionnaire design and testing. Am J Epidemiol. 1986;124:453–469. doi: 10.1093/oxfordjournals.aje.a114416. [DOI] [PubMed] [Google Scholar]
- 16.Pillow PC, Hursting SD, Duphorne CM, et al. Case-control assessment of diet and lung cancer risk in African Americans and Mexican Americans. Nutr Cancer. 1997;29:169–173. doi: 10.1080/01635589709514620. [DOI] [PubMed] [Google Scholar]
- 17.Yamamura Y, Oum R, Gbito KY, et al. Dietary intake of vegetables, fruits, and meats/beans as potential risk factors of acute myeloid leukemia: A Texas case-control study. Nutr Cancer. 2013;65:1132–1140. doi: 10.1080/01635581.2013.834946. [DOI] [PubMed] [Google Scholar]
- 18.Institute of Medicine (IOM) Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein, and amino acids. National Academy Press; Washington, D.C: 2002. [DOI] [PubMed] [Google Scholar]
- 19.Fung TT, Chiuve SE, McCullough ML, et al. Adherence to a DASH-style diet and risk of coronary heart disease and stroke in women. Arch Intern Med. 2008;168:713–720. doi: 10.1001/archinte.168.7.713. [DOI] [PubMed] [Google Scholar]
- 20.Randi G, Edefonti V, Ferraroni M, Vecchia C La, Decarli A. Dietary patterns and the risk of colorectal cancer and adenomas. Nutr Rev. 2010;68:389–408. doi: 10.1111/j.1753-4887.2010.00299.x. [DOI] [PubMed] [Google Scholar]
- 21.Alkerwi A, Vernier C, Crichton GE, Sauvageot N, Shivappa N, Hébert JR. Cross-comparison of diet quality indices for predicting chronic disease risk: findingsfrom the Observation of Cardiovascular Risk Factors in Luxembourg (ORISCAV-LUX) study. Br J Nutr. Dec. 2014;5:1–11. doi: 10.1017/S0007114514003456. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Harmon BE, Boushey CJ, Shvetsov YB, Ettienne R, Reedy J, Wilkens LR, Le Marchand L, Henderson BE, Kolonel LN. Associations of key diet-quality indexes with mortality in the Multiethnic Cohort: the Dietary Patterns Methods Project. Am J Clin Nutr. 2015 Mar;101(3):587–97. doi: 10.3945/ajcn.114.090688. doi:10.3945/ajcn.114.090688. Epub 2015 Jan 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hernandez-Valero MA, Thomson CA, Hernandez M, et al. Comparison of baseline dietary intake of Hispanic and matched non-Hispanic white breast cancer survivors enrolled in the Women's Healthy Eating and Living Study. J Am Diet Assoc. 2008;108:1323–1329. doi: 10.1016/j.jada.2008.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vrieling A, Buck K, Seibold P, et al. Dietary patterns and survival in German postmenopausal breast cancer survivors. Br J Cancer. 2013;108:188–192. doi: 10.1038/bjc.2012.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fung TT, Hu FB, Hankinson SE, et al. Low-carbohydrate diets, dietary approaches to stop hypertension-style diets, and the risk of postmenopausal breast cancer. Am J Epidemiol. 2011;174:652–660. doi: 10.1093/aje/kwr148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Izano MA, Fung TT, Chiuve SS, et al. Are diet quality scores after breast cancer diagnosis associated with improved breast cancer survival? Nutr Cancer. 2013;6:820–826. doi: 10.1080/01635581.2013.804939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Thomson CA, Rock CL, Thompson PA, et al. Vegetable intake is associated with reduced breast cancer recurrence in tamoxifen users: A secondary analysis from the women's healthy eating and living study. Breast Cancer Res Treat. 2011;125:519–527. doi: 10.1007/s10549-010-1014-9. [DOI] [PubMed] [Google Scholar]