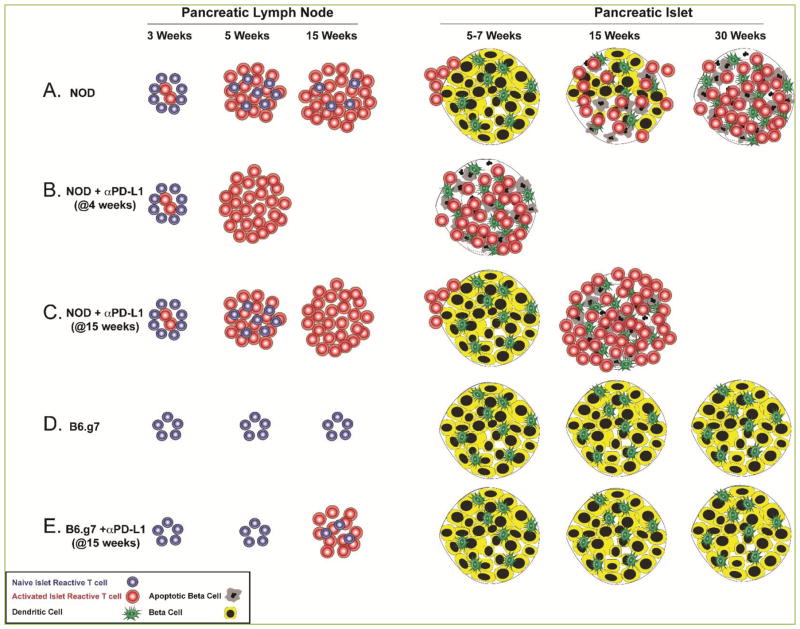
Figure 1. Model of islet antigen-specific CD4 T cell activation and islet inflammation timeline in NOD and B6.g7 mice.
(A) In NOD mice, insulin-specific CD4+ T cells encounter antigen in the pancreatic lymph node, expand and acquire the potential to traffic to the pancreas between 3 and 5 weeks of age. Pancreatic inflammation becomes more severe as mice age and peaks at disease onset, between 10 and 30 weeks (15 weeks as illustrated here). (B) Anti-PD-L1 treatment at 4 weeks of age significantly enhances T cell activation, thus leading to accelerated diabetes onset within 20 days in 90% of treated animals [38]. (C) PD-1 pathway blockade at a later time point when existing insulitis is extensive (at 15 weeks for example) [25], leads to a very rapid disease onset in NOD mice within 1–3 days [38]. (D) In B6.g7 mice, insulin-specific CD4+ T cells do not expand as mice age and ~80% of the islets remain uninfiltrated [25]. (E) PD-1 pathway blockade at 15 weeks of age leads to an increased number of activated insulin-specific CD4+ T cells in the pancreatic lymph node, but insulin reactive T cells do not traffic to the pancreas and the extent of islet inflammation does not change [25].