Abstract
Purpose
The purpose of this study is to examine the relationship between depressive symptoms and diabetes self-care in African American and Hispanic/Latino patients with type 2 diabetes and whether the association (if any) is mediated by diabetes-related self-efficacy.
Methods
The sample included self-report baseline data of African American and Hispanic/Latino patients with type 2 diabetes aged ≥18 years enrolled in a diabetes self-management intervention study. Depressive symptoms were assessed with the 9-item Patient Health Questionnaire. The Summary of Diabetes Self-Care Activities measured engagement in healthy eating, physical activity, blood glucose checking, foot care, and smoking. The Diabetes Empowerment Scale-Short Form assessed diabetes-related psychosocial self-efficacy. Indirect effects were examined using the Baron and Kenny regression technique and Sobel testing.
Results
Sample characteristics (n=250) were: Mean age of 53 years; 68% female; 54% African American; 74% with income <$20,000. Depressive symptoms showed a significant negative association with self-care domains of general diet, specific diet, physical activity, and glucose monitoring in the African American group. In Hispanics/Latinos, depression was inversely associated with specific diet. Self-efficacy served a significant mediational role in the relation between depression and foot care among African Americans.
Conclusions
Self-efficacy mediated the relationship between depression and foot care in the African American group, but was not found to be a mediator of any self-care areas within the Hispanic/Latino group. In clinical practice, alleviation of depressive symptoms may improve self-care behavior adherence. Diabetes education may consider inclusion of components to build self-efficacy related to diabetes self-care, especially among African American patients.
Keywords: diabetes self-care, depressive symptoms, self-efficacy, empowerment, type 2 diabetes, underserved/minority populations
Diabetes is the seventh leading cause of mortality in the US and its prevalence among Americans continues to grow.1 Racial/ethnic minority groups experience a greater diabetes burden with a documented prevalence rate two times that of their non-Hispanic white counterparts of similar age.1–4 These underrepresented groups also disproportionately experience worse glycemic control, higher rates of diabetes-related microvascular complications, and elevated rates of disease-related mortality.5–7 Patient engagement in self-management behaviors recommended by the American Diabetes Association (ADA) remains relatively low among low socioeconomic and ethnic minority populations despite documented benefits of diabetes self-care for overall disease management and for optimization of disease-related outcomes.8–10 Symptoms of depressed and anxious mood, which tend to co-occur in approximately one-third of individuals with diabetes,11 is an evident detrimental factor negatively affecting consistent and effective engagement in self-care practices such as physical activity and glucose monitoring.12 There is a critical need to identify the role of psychological factors and potential mechanistic intermediaries given low engagement levels across multiple diabetes self-care behaviors in low socioeconomic populations and ethnic/racial minorities.10
Existing literature reveals an additive detrimental effect and increased adverse health risk with depression and diabetes co-occurrence.13 Negative effects of comorbid depression and diabetes include lower medication adherence, decreased engagement in self-care and self-management, and increased medical expenditures among others.13,14 Despite the documented robust inverse association, the mechanism through which depression exerts its influence on diabetes self-care remains uncertain. Informed by the social learning theory, it is hypothesized that depressive symptoms encompassing low-affect, anhedonia, and hopelessness unfavorably impact individual-level confidence for successful engagement in diabetes self-care behaviors. Deteriorated confidence, i.e., low levels of self-efficacy, would in turn impede completion of multiple diabetes-related self-care practices. Self-efficacy is a strong determinant of engagement levels across behavioral domains of diabetes self-care activities consequently making it a plausible mechanistic intermediary.15,16 Ample evidence links low levels of perceived confidence for self-care behaviors performance to low levels of engagement across multiple diabetes-related health domains, particularly physical activity, diet, and glucose monitoring.15–18 There do not appear to be any studies of the association between depressive symptoms and diabetes-related self-efficacy in the context of diabetes self-care activities, particularly in low socioeconomic populations and ethnic/racial minorities.
Informed by the limited available evidence, the current study addressed the following research questions: (1) What is the association of depressive symptoms and diabetes self-care behaviors in low-income African American and Hispanic/Latino patients with type 2 diabetes?, and (2) Does diabetes-related self-efficacy mediate the relationship between depression and diabetes self-care in these minority patients? It is hypothesized that higher levels of depressive symptomatology will be associated with lower engagement levels for diabetes self-care behaviors, and that this association will be mediated by diabetes-related self-efficacy.
Materials and Methods
Study population and data source
The original data source for this study is the large randomized clinical trial (RCT) “Improving Diabetes Self-Management in Minorities.” Details of recruitment and the RCT study protocol have been published previously.19,20
Briefly, original study participants were recruited by clinic research staff across four federally qualified health centers (FQHCs) in underserved areas of Chicago. Inclusion criteria were as follows: (1) African American or Hispanic/Latino adult diagnosed with type 2 diabetes, (2) aged 18 years or older, (3) informed and consenting adult, (4) English or Spanish fluency, (5) recent (within 3 months of baseline enrollment) A1C lab values greater than or equal to 6.5% (48 mmol/mol), (6) currently receiving hypoglycemic medication (insulin and/or oral agents), and (7) minimum six-month clinical diagnosis for extant diabetes. Race/ethnicity categorization was based on self-identification using descriptors similar to the US Census Bureau. Participants were excluded if they: (1) were currently pregnant or planning for pregnancy during the study period, (2) presented with serious comorbid medical (e.g., cancer) or mental health conditions, or serious complications of diabetes (e.g., dialysis) and (3) were unavailable via phone. Study approval was obtained through the Institutional Review Board (IRB) at the University of Illinois at Chicago.
Study measures
Outcome variable of self-care
Engagement in self-care behaviors was evaluated using the Summary of Diabetes Self-Care Activities (SDSCA) measure.21 The SDSCA is a 13-item self-report questionnaire which inventories the relative frequency of completion of routine self-care tasks over the previous week. Evaluated self-care subcomponents include healthy eating (general [consistency in following healthful eating plan] and specific diet [consumption of fruits, vegetables, and high fat foods]), physical activity, blood glucose monitoring, foot care, medication adherence, and smoking status. Psychometric testing reveals suitable validity and reliability for both the English- and Spanish-language versions of the instrument.22 A sample item includes: “On how many of the last seven days did you eat five or more servings of fruits and vegetables?” With the exception of the dichotomous item capturing smoking status, items for each of the diabetes self-care behaviors captured the frequency of adherence from 0 to 7 days. Items within each self-care domain were averaged to calculate the mean number of days for which the self-care behaviors occurred (range from 0 days to 7). Self-care measures related to medication use were excluded from multivariable analyses due to a ceiling effect which, consistent with other previous studies,21 limited the utility of items estimating hypoglycemic medication use.
Depressive symptoms
The 9-item Patient Health Questionnaire (PHQ-9) is a psychometrically effective screening tool for depressive symptoms.23,24 The PHQ-9 uses a 4-point Likert scale (0—Not at all to 3—Nearly every day) to probe the extent to which an individual has been troubled by depressive symptoms within the last two weeks; scores range from 0–27. For descriptive analyses, depressive symptomatology was dichotomized into categories of minimal (PHQ-9 <10) versus moderate to severe (PHQ-9 ≥10) using the clinically recommended cut-off score of 10.24
Diabetes-related self-efficacy
Psychosocial self-efficacy in the context of diabetes self-management was measured using the Diabetes Empowerment Scale-Short Form (DES-SF).25 This instrument which has been validated across multiple populations in the English and Spanish language contains 8 items. A sample item includes, “In general, I believe that I am able to turn my diabetes goals into a workable plan.” Interviewees are asked to rate associated statements on a scale ranging from (1) strongly disagree to (5) strongly agree.
Covariates
Covariates included information on sociodemographic characteristics (age and income) and body mass index (BMI). BMI was calculated using self-reported measures of height (m2) and weight (kg).
Statistical analyses
Data analyses were conducted using statistical software (SAS 9.4; SAS, Inc, Cary, North Carolina). While 266 patients enrolled in the RCT, the current sample size across regression analyses included 250 patients with complete self-report data on the main variables of interest. Descriptive characteristics for the total sample are provided by depressive symptomatology status distinguishing those with minimal depression (PHQ-9<10) from those with moderate to severe depression (PHQ-9 ≥10). Group differences in participant characteristics across dichotomized depression categories and race/ethnicity were examined using F-tests and/or χ2-tests.
To test whether diabetes self-efficacy served as a mediator in the relationship between depression and diabetes self-care, mediational analysis was performed through use of the classic Baron and Kenny method.26 The predictor variable of depression was treated as a continuous measure and based on variable distribution, the self-care subcomponents were treated as count data (i.e., healthy eating, physical activity, glucose self-testing, foot care) or dichotomous data (i.e., smoking status). A three step modeling procedure was used as follows: (1) examination of the association between the dependent variable (i.e., diabetes self-care) and the independent variable of depressive symptomatology; (2) examination of the relationship between the hypothesized mediator of self-efficacy and the dependent variable (i.e., diabetes self-care); (3) the last step was to control for self-efficacy when examining the association between diabetes self-care and depressive symptoms. As a final step, the Sobel test27 was used to determine significant reductions in variance accounted for by the independent variable (i.e., depressive symptoms) after inclusion of hypothesized mediator (i.e., diabetes-related psychosocial self-efficacy). Covariates in the adjusted regression models included age, income, and BMI.
Results
Characteristics of the study sample
Table 1 provides characteristics for the total sample along with a stratified summary by depression status and race/ethnicity. The sample was evenly distributed by race/ethnicity with 53.7% self-identifying as African American and 46.3% as Hispanic/Latino. The sample was primarily female (68.4%) and ranged in age from 25 to 86 years (M=53.2, SD=12.3). This sample was of low socioeconomic status based on education and income. Overall, 60.0% of participants had less than a high school education and three-fourths reported an annual income below $20,000 (74.0%). Self-identification patterns for marital status were married (38.4%), never married, (24.0%), divorced (13.2%), widowed (13.2%) and separated (11.2%). A total of 95 (38.4%) patients reported being currently employed and 60.3% had some type of medical care coverage. In stratified analyses, participants classified as having moderate to severe symptoms of depression (i.e., PHQ-9 ≥ 10) were significantly younger (50.3 years vs. 53.9 years), more likely to be of African American descent, reported lower levels of annual income, and were less likely to be married.
Table 1.
Characteristics of the Study Sample by Depression Status and Race/Ethnicity (N =250)
| Variable | Total | Moderate to Severe Depressive Symptoms (PHQ-9≥10) |
Minimal Depressive Symptoms (PHQ-9<10) |
P-value | African American | Latino | P-value |
|---|---|---|---|---|---|---|---|
| Sociodemographic Characteristics | N = 250 | ||||||
| Age, M (SD) | 53.2 ± 12.3 | 50.3 ± 12.1 | 53.8 ± 12.1 | 0.04 | 51.8 ± 13.0 | 54.7 ± 11.5 | 0.06 |
| Female, % | 68.4 | 70.5 | 67.6 | 0.63 | 65.8 | 71.4 | 0.32 |
| Race/Ethnicity, % | |||||||
| African American | 53.7 | 67.2 | 48.4 | 0.01 | -- | -- | -- |
| Hispanic/Latino | 46.3 | 32.8 | 51.6 | -- | -- | -- | |
| Education, % | |||||||
| < High School | 60.0 | 58.0 | 61.1 | 0.64 | 37.9 | 85.2 | <0.001 |
| High School Graduate | 18.8 | 22.6 | 17.3 | 29.5 | 7.0 | ||
| > High School | 21.2 | 19.4 | 21.6 | 32.6 | 7.8 | ||
| Annual household income, % | |||||||
| Less than $20,000 | 74.0 | 85.4 | 70.7 | 0.04 | 70.9 | 78.9 | 0.21 |
| More than $20,000 | 26.0 | 14.6 | 29.3 | 29.1 | 21.1 | ||
| Employment Status, % | |||||||
| Currently Employed | 38.4 | 38.7 | 38.4 | 0.98 | 31.8 | t46.1 | 0.06 |
| Unemployed | 21.6 | 21.0 | 22.2 | 22.7 | 20.9 | ||
| Other | 40.0 | 40.3 | 39.4 | 45.5 | 33.1 | ||
| Health Insurance, % | |||||||
| Yes | 60.3 | 69.0 | 57.1 | 0.11 | 66.4 | 53.5 | 0.04 |
| No | 39.7 | 31.0 | 42.9 | 33.6 | 46.5 | ||
| Marital Status, % | |||||||
| Married | 38.4 | 27.4 | 42.2 | 0.01 | 22.7 | 56.5 | <0.001 |
| Never Married | 24.0 | 37.1 | 19.5 | 38.6 | 7.0 | ||
| Other | 37.6 | 35.5 | 38.4 | 38.6 | 36.5 | ||
| Biobehavioral Factors | |||||||
| BMI, M (SD) | 33.1 ± 7.1 | 34.4 ± 9.2 | 32.8 ± 6.2 | 0.21 | 34.6 ± 7.7 | 31.6 ± 5.9 | 0.001 |
| General Diet, M (SD) | 3.7 ± 2.3 | 3.1 ± 2.2 | 3.8 ±2.3 | 0.03 | 3.6 ± 2.2 | 3.7 ±2.4 | 0.89 |
| Specific Diet, M (SD) | 4.0 ± 1.6 | 3.1 ± 1.3 | 4.2 ±1.7 | < 0.001 | 3.7 ± 1.4 | 4.3 ± 1.8 | 0.008 |
| Physical Activity, M (SD) | 2.5 ± 2.1 | 2.3 ± 1.9 | 2.6 ±2.2 | 0.41 | 2.7 ± 1.9 | 2.3 ± 2.3 | 0.20 |
| Blood Glucose Checking, M (SD) | 3.6 ± 2.7 | 3.7 ± 2.4 | 3.6 ±2.8 | 0.77 | 4.1 ± 2.5 | 3.0 ± 2.8 | 0.001 |
| Medication, M (SD) | |||||||
| Insulin | 4.9 ± 0.7 | 4.2 ± 3.1 | 5.2 ±2.8 | 0.07 | 5.2 ±2.7 | 4.3 ± 3.2 | 0.12 |
| Oral Medication/Pills | 6.2 ± 2.0 | 5.5 ± 2.6 | 6.5 ±1.6 | 0.01 | 5.7 ±2.4 | 6.8 ± 1.1 | <0.001 |
| Foot Care, M (SD) | 4.5 ± 2.5 | 4.3 ± 2.5 | 4.6 ±2.4 | 0.39 | 4.6 ± 2.4 | 4.5 ± 2.5 | 0.84 |
| Smoking, % | |||||||
| Yes | 21.3 | 32.3 | 18.1 | 0.02 | 27.6 | 14.7 | 0.013 |
| No | 78.7 | 67.7 | 81.9 | 72.4 | 85.3 |
Descriptive information is also presented in Table 1 for profiles of body mass index and engagement levels across diabetes self-care activities. A mean BMI score of 33.2 (SD=7.1) was documented with this average value indicative of obesity using criteria from national guidelines.28,29 A total of 35.3% of patients self-reported use of insulin as part of their diabetes regimen. Over a 7-day period, self-reported diabetes self-care rates across multiple self-care behaviors ranged from engagement in the activity an average of 2.5 days to 6.2 days per week. Participants reported the highest diabetes self-care scores for oral medication use (6.2 days/week) and lowest for physical activity (2.5 days/week). Patients presenting elevated symptoms of depression reported significantly lower diabetes self-care scores for the behaviors of general diet, specific diet, and oral medication use. Those identifying as current smokers were also more likely to display elevated depressive symptom profiles. Also see in Table 1, African Americans displayed higher BMI scores and had a greater percentage of members identifying as current smokers. Finally, the African American subgroup had higher self-care scores for blood glucose self-testing, but lower scores for the behaviors of specific diet and oral medication use.
Association of depressive symptoms and diabetes self-care
The first step in mediational testing is to determine whether an association exists between the main predictor of interest and the behavioral outcome variable(s). Table 2 presents stratified analysis, by race/ethnicity, on the multivariable association of depression with the diabetes self-care behaviors of diet, physical activity, glucose self-testing, foot care, and smoking. In the African-American subgroup, depressive symptoms were found to be significantly associated with the self-care domains of general (β = −0.032; P = 0.01) and specific diet (β = −0.020; P = 0.02), physical activity (β = −0.046; P < 0.01), and glucose monitoring (β = −0.020; P = 0.01); a trend toward significance was evident for the self-care domain of foot care (β = −0.013; P = 0.09). Negative parameter estimates reveal an inverse relationship between depressive symptomatology and the above-mentioned self-care behaviors suggesting that higher depressive symptoms scores are associated with lower self-care performance levels. Only specific diet was significantly associated with depressive symptoms in the Hispanic/Latino subgroup with a negative beta suggesting an inverse relationship (see Table 2); trends toward significance were observed for the self-care behaviors of general diet and foot care.
Table 2.
Standardized regression weights (P values) for diabetes self-care measures regressed on covariates and depressive symptoms (PHQ-9)a, by race/ethnicity
| General Diet | Specific Diet | Physical Activity | Glucose Monitoring | Foot Care | Smoking Status | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Race/Ethnic Subgroup |
Coefficient Est. (β), SE |
P- value |
Coefficient Est. (β), SE |
P- value |
Coefficient Est. (β), SE |
P- value |
Coefficient Est. (β), SE |
P- value |
Coefficient Est. (β), SE |
P-value | Coefficient Est. (β), SE |
P- value |
| African American | −0.032 (0.01) | <0.01 | −0.020 (0.009) | 0.02 | −0.046 (0.01) | <0.01 | −0.020 (0.008) | 0.01 | −0.013 (0.008) | 0.09 | −0.053 (0.04) | 0.13 |
| Hispanic/Latino | −0.021 (0.01) | 0.06 | −0.030 (0.01) | <0.01 | −0.001 (0.01) | 0.92 | 0.013 (0.01) | 0.25 | −0.019 (0.01) | 0.06 | −0.076 (0.05) | 0.15 |
Adjusted for age, income, and body mass index.
Mediational testing procedures and role of self-efficacy
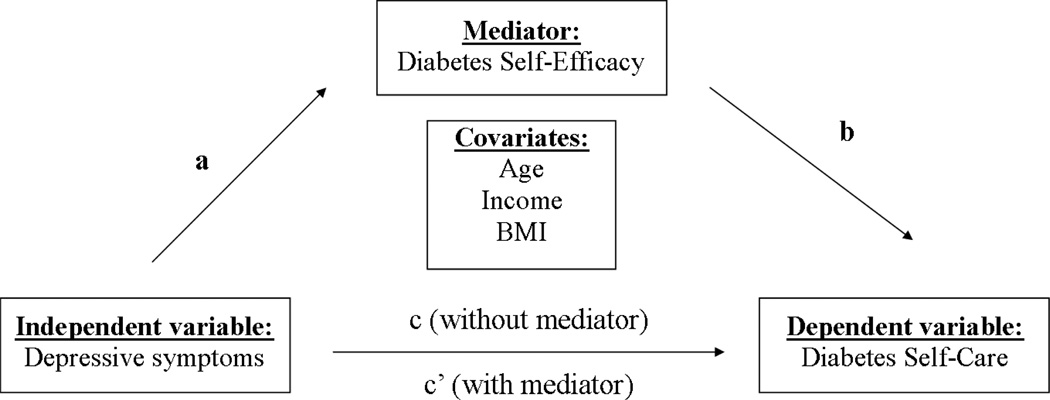
As illustrated in Figure 1, Step 2 of the mediational analysis (path a) requires examination of the direct effect of depressive symptoms on self-efficacy. For the African American subgroup (see Table 3), depressive symptomatology was significantly associated with self-efficacy in the unadjusted model (β = −0.024; P = 0.01), while displaying a trend toward significance after addition of relevant covariates (β = −0.019; P = 0.06). No such association was evident in the Hispanic/Latino patient subgroup. In lieu of results for initial mediational testing, i.e., paths a and c depicted in Figure 1, final analytic regression steps were conducted only for the African American subgroup for the self-care behaviors of diet, physical activity, glucose self-testing, and foot care.
Figure 1.
Baron and Kenny Mediational Model Test
Table 3.
Standardized regression weights (P value) for diabetes self-efficacy regressed on covariates and depressive symptoms (PHQ-9) a, by race ethnicity
| Hispanic/Latino Subgroup | African American Subgroup | |||
|---|---|---|---|---|
| Depressive Symptoms | Coefficient Est. (β), SE |
P-value | Coefficient Est. (β), SE |
P-value |
| M1: Unadjusted | 0.004 (0.012) | 0.73 | −0.024 (0.010) | 0.01 |
| M2: Multivariable Adjusteda | 0.004 (0.012) | 0.75 | −0.019 (0.010) | 0.06 |
Adjusted for age, income, and body mass index.
Table 4 presents the results for the final step of the mediational analysis for the African American subsample. Across self-care behaviors of general diet (β = −0.029; P < 0.01), specific diet (β = −0.019; P = 0.04), and glucose self-testing (β = −0.020; P = 0.02), consistency and robustness of statistical significance for depression was evident even after inclusion of the hypothesized mediator of self-efficacy. This suggests that complete and partial mediation via self-efficacy was not achieved. Self-efficacy was found to be significantly associated with physical activity (P=0.02) and foot care (P=0.02), with larger self-efficacy scores associated with higher self-care performance levels. In the mediational model, diabetes-specific self-efficacy was significantly associated with physical activity with an observed decrease in magnitude for the P-value corresponding to depressive symptomatology. Nonetheless, the Sobel test confirmed that partial mediation was not achieved for the outcome measure of physical activity given the minor change in magnitude in the P-value for the construct of depression; not depicted in the tables, the Sobel test resulted in an associated P-value of 0.12. For the outcome measure of foot care, depressive symptomatology was no longer significant after the inclusion of diabetes-related self-efficacy, suggesting a significant mediational role via the construct of self-efficacy; note, a significant bivariate association was evident in unadjusted models displaying a correlational P-value of 0.03 for depressive symptoms and foot care in the African American cohort.
Table 4.
Standardized regression weights (P values) for diabetes self-care measures regressed on covariates and depressive symptoms (PHQ-9)a, with addition of diabetes self-efficacy (DES-SF) in the mediational model for the African American Subgroup
| General Diet | Specific Diet | Physical Activity | Glucose Monitoring | Foot Care | Smoking Status | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| African American | Coefficient Est. (β), SE |
P- value |
Coefficient Est. (β), SE |
P- value |
Coefficient Est. (β), SE |
P- value |
Coefficient Est. (β), SE |
P- value |
Coefficient Est. (β), SE |
P-value | Coefficient Est. (β), SE |
P- value |
| Depressive Symptoms | −0.029 (0.01) | <0.01 | −0.019 (0.009) | 0.04 | −0.042 (0.01) | <0.01 | −0.020 (0.01) | 0.02 | −0.010 (0.01) | 0.22 | −0.048 (0.04) | 0.18 |
| Self-Efficacy | 0.132 (0.08) | 0.09 | 0.059 (0.08) | 0.43 | 0.207 (0.09) | 0.02 | 0.035 (0.07) | 0.62 | 0.163 (0.07) | 0.02 | 0.324 (0.33) | 0.32 |
Adjusted for age, income, and body mass index.
Discussion
In the context of the current state of knowledge, what follows is a discussion of the association between depressive symptoms and diabetes self-care behaviors in low-income African American and Hispanic/Latino patients, with consideration of whether self-efficacy plays a mediational role. Recruited from federally qualified health centers in Chicago, the current study included a clinical sample of adult, low income, African American and Hispanic/Latino patients with type 2 diabetes. Exceeding rates expected for the general US population, 24.8% of the current cohort was considered to have moderate to severe symptoms of depression based on the PHQ-9. Engagement in diabetes self-care behaviors displayed a considerable range from 2.5 days/week for physical activity to 6.2 days/week for oral medication adherence. This is consistent with prior work suggesting low self-care adherence levels in minority populations, particularly in the complex areas of exercise and home glucose monitoring.10 In the African American subgroup, self-efficacy was shown to mediate the relationship between depressive symptoms and foot care.
The first stage of mediational testing revealed that higher depressive symptomatology scores were associated with lower engagement levels across self-care activities of diet, physical activity, glucose monitoring, and an evident trend toward significance for the domain of foot care. The current cross-sectional findings are consistent with prior research.13,14 Multiple studies with and without inclusion of racial/ethnic minority subsamples with type 1 and 2 diabetes produce robust evidence documenting an inverse relationship between depressive symptomatology and performance of self-care activities, with higher depression scores associated with lower levels of self-care activities. Research also indicates that the magnitude of depressive symptoms experienced, i.e., minor versus major depression, seems of less import as even subthreshold levels can reduce engagement in positive health behaviors.30 Although there are multiple hypotheses, the mechanistic pathway through which depression impacts engagement in self-care activities remains relatively obscure.
The current study documents differential effects by race/ethnicity, whereby the negative link between depressive symptoms and self-care was more robust for the African American subgroup. Differential experience of and disease-specific manifestation across ethnic/racial groups has been suggested in prior literature.31,32 Methodological limitations, i.e., sample size and low variance in depression scores, could explain less robust associations of depression and self-care in the Hispanic/Latino subsample. The sample size of 112 could have limited the power to detect clinically meaningful associations, with relatively fewer Hispanic/Latino adults reporting elevated depressive symptom thresholds, i.e., 17.2% (H/L) vs. 31.3% (AA). The larger number of Hispanics/Latinos with favorable psychological well-being and limited variance in depression scores could have impacted findings.
The current study appears to be the first to explore the role of self-efficacy in the relationship between depressive symptoms and self-care in a low-income cohort of ethnic/racial minority patients with diabetes. Self-efficacy was an important construct in the relational pathway between depressive symptoms in only one self-care area, foot care, and only for the African American cohort. Foot care results for the African American subgroup are consistent with prior research. Among African Americans with a chronic condition (e.g., hypertension), greater self-efficacy scores have been linked with more favorable health behavior profiles such as augmented participation in physical activity, medication adherence, and healthful dietary intake. Schoenthaler et al.33 found self-efficacy to mediate the relationship between depressive symptoms and medication adherence in African American adults with hypertension. Similar results are evident in the context of type 2 diabetes.34 It is hypothesized that negative cognitive appraisals resulting from depression diminish personal confidence and subsequent engagement in self-care activities.33 Replication studies using large epidemiologic cohorts are needed to confirm the mechanistic role of self-efficacy in the relationship between depressive symptoms and foot care to refute possibility of a false positive relationship. Nuanced investigations should additionally test why and to what extent self-efficacy is of import for foot care but not other self-care areas and only in one racial/ethnic subgroup.
Emphasizing the importance of not treating minority groups in aggregate, divergent functioning of self-efficacy was evident by race/ethnicity when examining the link between depressive symptoms and foot care. It is possible that ethnic or cultural factors lead to differential manifestations of depression31,32 and to divergent effects on feelings of confidence and mastery. Multiple studies document the concept of fatalismo in the Hispanic/Latino community in the context of chronic illness management;35 fatalismo is defined as, “a doctrine that events are fixed in advance so that human beings are powerless to change them.”36,37 Intrinsic belief that illness management is outside of the individual locus of control may serve to attenuate the negative effects triggered by symptoms of depression. In effect, it is possible that fatalistic beliefs that diabetes and its complications are inevitable may result in an overall reduction in confidence in the performance of diabetes self-management behaviors over and above that produced by depression and its associated symptoms. This hypothesis is supported by findings linking higher scores of diabetes-related fatalism with lower engagement levels across diabetes self-care activities.35 A second hypothesis posits that depression may be more intricately tied to self-efficacy in the African American subgroup (for foot care and when compared to Hispanics/Latinos), if Hispanics/Latinos with literacy and language barriers already experience deteriorations in self-confidence beyond the additive effect brought about by symptoms of depression. Challenges associated with limited English proficiency include reduced effectiveness in the use of health information, multiple barriers when attempting to navigate the health service system, and the mandatory need for interpretation services when attempting to communicate with non-Spanish speaking health providers.
The present study has multiple strengths. This is the first study to examine the mediational role of self-efficacy in the relationship between depressive symptoms and diabetes self-care in a population composed of underserved U.S. Hispanic/Latino and African American patients with diabetes. Well-validated instruments were used to assess symptoms of depression, diabetes-related self-efficacy, and self-care behaviors across multiple domains. Social desirability bias was possibly reduced as assessments were completed on a computerized tablet. However, study limitations should be considered when interpreting findings. As self-report instruments were employed, measurement error and misclassification bias are plausible across psychosocial constructs and behavioral engagement levels. Determination of depression status was based solely on a self-report measure (i.e., PHQ-9) and not a clinical diagnosis made by a mental health provider. As with all cross-sectional studies, the design does not permit for assumptions of inferences about causality. Specifically, it is possible that individuals display lower levels of depressive symptomatology as a consequence of elevated feelings of positive affect related to favorable profiles of diabetes self-care activities.38 Longitudinal studies are needed to adequately address uncertainties regarding temporality of the association. Finally, although the majority of enrolled Latino participants were of Mexican background, this study was limited in characterizing the heterogeneity across the Hispanic/Latino subgroup (e.g., excluding information such as cultural assimilation).
Implications and Recommendations
The findings for the current study offer multiple implications for healthcare practitioners seeking to optimize diabetes management in minority populations. Findings confirm low levels of self-care in African American and Hispanic/Latino adult with type 2 diabetes, particularly for complex behavior such as physical activity and glucose self-monitoring. Innovative, accessible, and cost-effective behavioral and educational interventions are needed to augment and support engagement in diabetes self-management behaviors in these underserved groups.
Second, heightened co-occurrence of depressive symptoms in patients with diabetes suggests the need to bolster screening efforts to detect psychological challenges with implementation of interventions as needed (e.g., cognitive behavioral therapy). Proper treatment, pharmacological and/or psychotherapeutic, should be implemented to improve psychological functioning given its impact of self-care adherence. Finally, given the mediational role of diabetes-related self-efficacy, it may be beneficial to measure this construct across patient populations with an action plan to provide support as necessary. Previous studies have made similar clinical practice recommendations regarding the need to augment diabetes-related self-efficacy, with interventions developed to empower patients to take charge of their physical and emotional well-being.39 In clinical practice, diabetes education may consider inclusion of components to build self-efficacy related to diabetes self-care, especially among African American patients.
Acknowledgments
Funding. The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Research reported in this publication was supported by National Institute of Nursing Research of the National Institutes of Health under Grant R01 NR010313 (L. Ruggiero, PI). The content and views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the National Institute of Nursing Research, the United States government, or the National Institute of Health.
The authors would like to acknowledge the support of the following individuals and groups: Roxana Barron, Mike Berbaum, PhD, Desiree Bond, Paula Butler, MD, Young-Ku Choi, PhD, Daisy Cintron, MA, Nilsa Dominguez, Mickey Eder, PhD, Ben Gerber, MD, MPH, Lauretta Quinn, Ph.D., Amparo Castillo, MD, Joseph Day, Dr.PH, Diana Ingram, Ph.D., Berenice Hernandez, Jairo Mejia, MD, Sandra Franklin, Sonya Hopkins, Teresa Mantinan, Ada Moadsiri, DrPH, Erica Seltzer, DrPH, Yashika Watkins, PhD, Steve Whitman, PhD, and Shikhi Bhansari, along with the entire Diabetes Self-Care research team and the Access Community Health Network Clinic Staff at study sites.
References
- 1.Centers for Disease Control and Prevention. National diabetes statistics report: estimates of diabetes and its burden in the United States, 2014. Atlanta, GA: US Department of Health and Human Services; 2014. [Google Scholar]
- 2.Daviglus ML, Talavera GA, Aviles-Santa ML, et al. Prevalence of Major Cardiovascular Risk Factors and Cardiovascular Diseases Among Hispanic/Latino Individuals of Diverse Backgrounds in the United States. Jama-J Am Med Assoc. 2012;308(17):1775–1784. doi: 10.1001/jama.2012.14517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cowie CC, Rust KF, Ford ES, et al. Full Accounting of Diabetes and Pre-Diabetes in the US Population in 1988–1994 and 2005–2006. Diabetes Care. 2009;32(2):287–294. doi: 10.2337/dc08-1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Flegal KM, Ezzati TM, Harris MI, et al. Prevalence of Diabetes in Mexican-Americans, Cubans, and Puerto-Ricans from the Hispanic Health and Nutrition Examination Survey, 1982–1984. Diabetes Care. 1991;14(7):628–638. doi: 10.2337/diacare.14.7.628. [DOI] [PubMed] [Google Scholar]
- 5.Harris MI. Racial and ethnic differences in health care access and health outcomes for adults with type 1 diabetes. Diabetes Care. 2001;24(3):454–459. doi: 10.2337/diacare.24.3.454. [DOI] [PubMed] [Google Scholar]
- 6.Campbell JA, Walker RJ, Smalls BL, Egede LE. Glucose control in diabetes: the impact of racial differences on monitoring and outcomes. Endocrine. 2012;42(3):471–482. doi: 10.1007/s12020-012-9744-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lanting LC, Joung IMA, Mackenbach JP, Lamberts SWJ, Bootsma AH. Ethnic differences in mortality, end-stage complications, and quality of care among diabetic patients - A review. Diabetes Care. 2005;28(9):2280–2288. doi: 10.2337/diacare.28.9.2280. [DOI] [PubMed] [Google Scholar]
- 8.Choi S, Lee JA, Rush E. Ethnic and Language Disparities in Diabetes Care among California Residents. Ethnic Dis. 2011;21(2):183–189. [PubMed] [Google Scholar]
- 9.Levine DA, Allison JJ, Cherrington A, Richman J, Scarinci IC, Houston TK. Disparities in Self-Monitoring of Blood Glucose among Low-Income Ethnic Minority Populations with Diabetes, United States. Ethnic Dis. 2009;19(2):97–103. [PubMed] [Google Scholar]
- 10.Nwasuruba C, Khan M, Egede LE. Racial/ethnic differences in multiple self-care behaviors in adults with diabetes. J Gen Intern Med. 2007;22(1):115–120. doi: 10.1007/s11606-007-0120-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes - A meta-analysis. Diabetes Care. 2001;24(6):1069–1078. doi: 10.2337/diacare.24.6.1069. [DOI] [PubMed] [Google Scholar]
- 12.Ciechanowski PS, Katon WJ, Russo JE. Depression and diabetes: impact of depressive symptoms on adherence, function, and costs. Arch Intern Med. 2000;160(21):3278–3285. doi: 10.1001/archinte.160.21.3278. [DOI] [PubMed] [Google Scholar]
- 13.Lin EHB, Katon W, Von Korff M, et al. Relationship of depression and diabetes self-care, medication adherence, and preventive care. Diabetes Care. 2004;27(9):2154–2160. doi: 10.2337/diacare.27.9.2154. [DOI] [PubMed] [Google Scholar]
- 14.Gonzalez JS, Peyrot M, McCarl LA, et al. Depression and Diabetes Treatment Nonadherence: A Meta-Analysis. Diabetes Care. 2008;31(12):2398–2403. doi: 10.2337/dc08-1341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hurley AC, Shea CA. Self-efficacy: strategy for enhancing diabetes self-care. Diabetes Educ. 1992;18(2):146–150. doi: 10.1177/014572179201800208. [DOI] [PubMed] [Google Scholar]
- 16.Aljasem LI, Peyrot M, Wissow L, Rubin RR. The impact of barriers and self-efficacy on self-care behaviors in type 2 diabetes. Diabetes Educ. 2001;27(3):393–404. doi: 10.1177/014572170102700309. [DOI] [PubMed] [Google Scholar]
- 17.Nouwen A, Ford T, Balan AT, Twisk J, Ruggiero L, White D. Longitudinal motivational predictors of dietary self-care and diabetes control in adults with newly diagnosed type 2 diabetes mellitus. Health Psychol. 2011;30(6):771. doi: 10.1037/a0024500. [DOI] [PubMed] [Google Scholar]
- 18.Johnston-Brooks CH, Lewis MA, Garg S. Self-efficacy impacts self-care and HbA1c in young adults with Type I diabetes. Psychosom Med. 2002;64(1):43–51. doi: 10.1097/00006842-200201000-00007. [DOI] [PubMed] [Google Scholar]
- 19.Hernandez R, Ruggiero L, Riley BB, et al. Correlates of self-care in low-income African American and Latino patients with diabetes. Health Psychol. 2014;33(7):597. doi: 10.1037/hea0000043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ruggiero L, Riley BB, Hernandez R, et al. Medical Assistant Coaching to Support Diabetes Self-Care Among Low-Income Racial/Ethnic Minority Populations Randomized Controlled Trial. West J Nurs Res. 2014 doi: 10.1177/0193945914522862. 0193945914522862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Toobert DJ, Hampson SE, Glasgow RE. The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes Care. 2000;23(7):943–950. doi: 10.2337/diacare.23.7.943. [DOI] [PubMed] [Google Scholar]
- 22.Vincent D, McEwen MM, Pasvogel A. The validity and reliability of a Spanish version of the summary of diabetes self-care activities questionnaire. Nurs Res. 2008;57(2):101–106. doi: 10.1097/01.NNR.0000313484.18670.ab. [DOI] [PubMed] [Google Scholar]
- 23.Kroenke K, Spitzer RL. The PHQ-9: A new depression diagnostic and severity measure. Psychiat Ann. 2002;32(9):509–515. [Google Scholar]
- 24.Kroenke K, Spitzer RL, Williams JBW. The PHQ-9 - Validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Anderson RM, Fitzgerald JT, Gruppen LD, Funnell MM, Oh MS. The Diabetes Empowerment Scale-Short Form (DES-SF) Diabetes Care. 2003;26(5):1641–1642. doi: 10.2337/diacare.26.5.1641-a. [DOI] [PubMed] [Google Scholar]
- 26.Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 27.Sobel ME. Asymptotic intervals for indirect effects in structural equation models. In: Leinhart S, editor. Sociological Methodology. San Francisco, CA: Jossey-Bass; 1982. pp. 290–3122. [Google Scholar]
- 28.Ben-Menachem E. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: The evidence report. Epilepsia. 2007;48:42–45. [Google Scholar]
- 29.Pi-Sunyer FX, Becker DM, Bouchard C, et al. Executive summary of the clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults. J Am Diet Assoc. 1998;98(10):1178–1191. [Google Scholar]
- 30.Egede LE, Ellis C, Grubaugh AL. The effect of depression on self-care behaviors and quality of care in a national sample of adults with diabetes. Gen Hosp Psychiatry. 2009;31(5):422–427. doi: 10.1016/j.genhosppsych.2009.06.007. [DOI] [PubMed] [Google Scholar]
- 31.Ayalon L, Young MA. A comparison of depressive symptoms in African Americans and Caucasian Americans. J Cross Cult Psychol. 2003;34(1):111–124. [Google Scholar]
- 32.Kim G, Chiriboga DA, Jang Y. Cultural Equivalence in Depressive Symptoms in Older White, Black, and Mexican-American Adults. Am Geriatr Soc. 2009;57(5):790–796. doi: 10.1111/j.1532-5415.2009.02188.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schoenthaler A, Ogedegbe G, Allegrante JP. Self-Efficacy Mediates the Relationship Between Depressive Symptoms and Medication Adherence Among Hypertensive African Americans. Health Educ Behav. 2009;36(1):127–137. doi: 10.1177/1090198107309459. [DOI] [PubMed] [Google Scholar]
- 34.Sacco WP, Wells KJ, Vaughan CA, Friedman A, Perez S, Matthew R. Depression in adults with type 2 diabetes: The role of adherence, body mass index, and self-efficacy. Health Psychol. 2005;24(6):630–634. doi: 10.1037/0278-6133.24.6.630. [DOI] [PubMed] [Google Scholar]
- 35.Walker RJ, Smalls BL, Hernandez-Tejada MA, Campbell JA, Davis KS, Egede LE. Effect of diabetes fatalism on medication adherence and self-care behaviors in adults with diabetes. Gen Hosp Psychiatry. 2012;34(6):598–603. doi: 10.1016/j.genhosppsych.2012.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bernal G, Enchautegui-de-Jesús N. Latinos and Latinas in community psychology: A review of the literature. Am J Commun Psychol. 1994;22(4):531–557. doi: 10.1007/BF02506892. [DOI] [PubMed] [Google Scholar]
- 37.Bernal G, Sáez-Santiago E. Culturally centered psychosocial interventions. J Community Psychol. 2006;34(2):121. [Google Scholar]
- 38.Katon W, Von Korff M, Ciechanowski P, et al. Behavioral and clinical factors associated with depression among individuals with diabetes. Diabetes Care. 2004;27(4):914–920. doi: 10.2337/diacare.27.4.914. [DOI] [PubMed] [Google Scholar]
- 39.Funnell MM, Anderson RM, Arnold MS, et al. Empowerment: an idea whose time has come in diabetes education. Diabetes Educ. 1991;17(1):37–41. doi: 10.1177/014572179101700108. [DOI] [PubMed] [Google Scholar]