Abstract
The objective of our intervention was to examine the benefits of incorporating traditional birth attendants (TBA) in HIV Prevention of Mother to Child Transmission (PMTCT) service delivery. We developed a training curriculum for TBAs related to PMTCT and current TBA roles in Malawi. Fourteen TBAs and seven TBA assistants serving 4 urban health centre catchment areas were assessed, trained and supervised. Focus group discussions with the TBAs were conducted after implementation of the program. From March 2008 to August 2009, a total of 4017 pregnant women visited TBAs, out of which 2133 (53.1%) were directly referred to health facilities and 1,884 (46.9%) women delivered at TBAs and subsequently referred. 168 HIV positive women were identified by TBAs. Of these, 86/168 (51.2%) women received nevirapine and 46/168 (27.4%) HIV exposed infants received nevirapine. The challenges in providing PMTCT services included lack of transportation for referrals and absence of a reporting system to confirm the woman’s arrival at the health center. Non-disclosure of HIV status by patients to the TBAs resulted in inability to assist nevirapine uptake. TBAs, when trained and well-supervised, can supplement efforts to provide PMTCT services in communities.
Keywords: Traditional Birth Attendants, PMTCT, Malawi
Introduction
Traditional birth attendants (TBAs) are commonly used in Malawi1. Of the 97% of pregnant women who access antenatal care in Malawi, 54% deliver in a health facility while 43% deliver in the community with TBAs2. While the role of TBAs working in Malawi has evolved over time, currently the primary role of TBAs is to provide community education and refer women to health centres, rather than performing deliveries. However, due to challenges with referrals and transportation, deliveries are commonly performed by TBAs.
The HIV prevalence rate among pregnant women in Malawi is high. In 2008, adult HIV prevalence among those aged 15–49 was at 12%3, and the current HIV prevalence is at 11%4. HIV prevalence in urban areas is estimated to be substantially higher than in rural areas and current estimates from the PMTCT program have suggested the Lilongwe urban antenatal prevalence is 15%5. Without a strong PMTC program, 14–45% of infants can become infected with HIV during labor, delivery and breastfeeding6. The mother to child transmission (MTCT) rate in Malawi without the use of ART prophylaxis is approximately 27% at 6 weeks7. Given the high prevalence of HIV and the frequency of TBA deliveries, engaging TBAs in PMTCT activities may improve the success of PMTCT programs and increase rates of nevirapine (NVP) uptake, the antiretroviral used as a prophylaxis for vertical HIV transmission at the time of this assessment.
Previous studies have shown that involving TBAs in HIV prevention and PMTCT programs could reduce HIV infant infections8. A study in rural Lilongwe described TBAs as being important members in the community based on their service delivery9. In Cameroon, TBAs dispensed NVP to HIV positive mothers and ensured that newborns receive postpartum NVP prophylaxis as part of an integrated strategy in the PMTCT program10. In Thyolo, Malawi, HIV pregnant women who delivered with TBAs were contacted and all reported their infants failed to receive NVP, suggesting a critical gap in PMTCT8.
We sought to conduct implementation research within our PMTCT program at Bwaila District Hospital to identify and examine the benefit of incorporating TBAs in the PMTCT process. Our hypothesis was that incorporating TBAs into the PTMCT process would result in more women and infants receiving single dose NVP after delivery.
Methods
We used both quantitative and qualitative methods to evaluate the feasibility and benefits of incorporating TBAs in PMTCT service delivery. TBA logs were designed to collect quantitative data; focus group discussions were used to collect qualitative data.
TBA pre-assessment
In January 2008, we collected a list of active TBAs conducting home deliveries surrounding our four PMTCT sites of Bwaila Hospital, Kawale, Area 18 and Area 25 Health Centers. We conducted a baseline assessment of the TBAs to determine suitability for participation. The research team, in collaboration with the Lilongwe District Health Office, visited the targeted areas to assess the TBAs based on the eligibility criteria. These included previous TBA training by the Malawi Ministry of Health, attendance to more than five deliveries per month, and presence of a placenta pit, delivery room, toilet, bathroom and a clean source of water at the TBAs’ home. Additionally, each site was assessed for the presence of TBA assistants. We selected 14 TBAs and seven TBA assistants whom we involved in the programme. The assistants were involved in the programme to assist TBAs who could not read and write on their own. Their main responsibility was record documentation.
PMTCT Training
In March 2008, we conducted PMTCT training for the TBAs that included eight days for didactic modules and two days for practical training. TBA assistants attended the last two days of practical training to learn how to identify HIV infected women and use the TBA log, as this was a vital instrument for monitoring and evaluation.
Based on the Ministry of Health TBA training manual, the didactic training included the following topics: HIV/AIDS and PMTCT, psychosocial aspects of HIV/AIDS, confidentiality, infection prevention, management of women during labour and delivery, postpartum care and administration of NVP, and monitoring and evaluation of TBA activities. For data collection, the existing Ministry of Health TBA log was modified to include three columns related to PMTCT and both TBA and TBA assistants were trained in its use (Figure 1). The practical training at Kawale Health Centre included observing NVP dosing of the infants, identifying HIV positive women using a health passbook, becoming oriented to the Maternal and Child Health activities, and learning how health workers handle clients at a health facility. Additionally, HIV infection prevention was emphasized through appropriate demonstration by the nurses on the labour ward.
Figure 1.
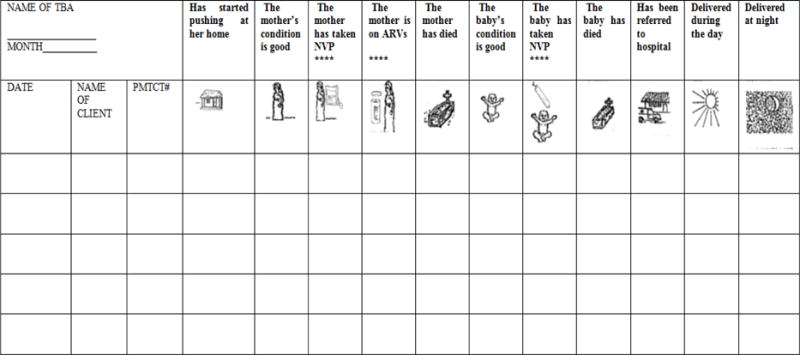
TBA Log
At the end of the training, the TBAs were provided with revised TBA logs and delivery kits which contained gloves, clean razor blades, string, matches, candles, cotton wool, and plastic sheets for facilitating the PMTCT intervention. The training was conducted in the local language (Chichewa).
Supervision
Bi-monthly from the end of April 2008, the programme supervisor visited the TBAs in their homes. During the visits, the supervisor reviewed the TBA logs, verified how they were identifying HIV positive women and how they administered NVP to HIV positive women and exposed babies. She also asked the TBAs if they had any implementation challenges or needed any re-training. The supervisor provided re-training on request and as needed if deficiencies were noted.
Focus Group Discussion (FGD)
Following six months of the program (August 2008), we conducted two focus group discussions with the TBAs to determine their level of willingness to participate in the PMTCT program. The discussions also focused on the incentives and barriers for TBA involvement in the PMTCT activities. Each group had seven TBAs, and no TBA assistants. The discussions were audio recorded, data were transcribed and expanded in Chichewa based on observations made during the discussions and then translated into English. Data was analyzed using grounded theory and manual coding.
The study was approved by the National Health Sciences Research Committee in Malawi and the University of North Carolina Institutional Review Board.
Results
Description of TBAs and TBA assistants
The TBAs were generally older women from 50 years and above, while the assistants were younger women. TBA assistants were typically relatives of TBAs and were unofficially apprenticing in the profession. Half of the TBAs were illiterate and were paired with a TBA assistant to assist with reading and writing (Table 1). Most TBAs were poor. Their lives depended largely on cultivating maize for home consumption. They also charged a fee for assisting women to deliver, a second source of income. Before the training, the TBAs conducted many deliveries in a month (median=10) (Table 1).
Table 1.
Characteristics of the Traditional Birth Attendants and Deliveries Pre-intervention.
| Deliveries conducted in a month | Literate | Assistant | |
|---|---|---|---|
| TBA 1 | 20 | Yes | None |
| TBA 2 | 3 | Yes | None |
| TBA 3 | 11 | Yes | None |
| TBA 4 | 8 | No | Yes (grand-daughter) |
| TBA 5 | 8 | No | Yes (Sister-in-law) |
| TBA 6 | 7 | Yes | None |
| TBA 7 | 6 | Yes | None |
| TBA 8 | 25 | No | Yes (grand-daughter) |
| TBA 9 | 10 | Yes | None |
| TBA 10 | 10 | No | Yes (grand-daughter) |
| TBA 11 | 20 | Yes | None |
| TBA 12 | 44 | No | Yes |
| TBA 13 | 5 | No | Yes (grand-daughter) |
| TBA 14 | 10 | No | Yes |
TBA Logs
We collected TBA logs once per month. From March 2008 to August 2009, a total of 4017 pregnant women visited the TBAs. Of these 2133 (53%) were referred directly to deliver in health facilities and 1884 (46.9%) delivered with the TBAs and were subsequently referred. Of the 1884 women, 168 (8.9%) were identified as HIV positive. Of the HIV positive women who delivered with a TBA 86/168 (51%) received NVP. Only 46/168 (27.4%) of the HIV exposed infants were given NVP by the TBA. All infants were referred.
Supervision visits
Supervision visits indicated that most TBAs correctly interpreted marks and pictures on the TBA log. Review of TBA logs demonstrated that 11 (78%) of the TBAs appropriately completed the logs and 3 (22%) TBAs required additional education to identify an HIV positive woman using the health passport book.
Focus Group Discussions
During the focus group discussions, we asked the TBAs what they had learned and put into practice. We also asked them about their incentives to participate in PMTCT service delivery and barriers that hinder access to PMTCT services.
Learning and applying what was taught
TBAs reported they had increased knowledge of HIV and PMTCT after the training. They expressed knowledge on modes of HIV transmission from mother to child during pregnancy, child birth, and breast feeding. They reported the significance of administering NVP: that if taken at the onset of labor, it can greatly reduce HIV transmission from mothers to babies.
Consistent with the training material, the TBAs referred all pregnant women to the nearest health facility for delivery care services. TBAs only delivered babies in unavoidable situations with prompt referral after delivery.
“…when we have conducted a delivery we don’t leave the person like that, we refer her to the hospital….”
TBAs also mentioned that they had reduced the numbers of deliveries upon receiving training:
“Some time back I used to conduct 10 deliveries but now I am conducting three or four and sometimes five deliveries. That’s the change that I have seen and I am also happy…”
“… since we were trained at Kamundi, things have really changed because we used to conduct deliveries anyhow…we were just conducting the deliveries without sending the women to the hospital. When we were trained you advised us that when a woman has delivered regardless of whether she is okay or not, she should be sent to the hospital for check-up and now things are better because we are sending any pregnant woman. That’s what has changed and the training should continue”.
“I am seeing a difference because there used to be many women for antenatal and delivery at my clinic. But now things have changed I am working well. Few people are coming showing that it is helping … because we are sending them to the hospital”.
During supervision and focus group discussions the TBAs stated they had the ability to identify HIV positive women which was confirmed by the logs which showed 168 HIV positive women were identified. One mentioned that “…when a woman comes to us we see in her health passbook if the woman has the virus.”
One mentioned that possession of a health passport book was crucial for knowing whether a woman is HIV positive or not:
“…we look on the card because the card is the book that we see when the person comes. We check to see what’s in the card and when we look in the card we know that this one they wrote X that means she is well [X meant being HIV negative, XX meant being HIV positive]”.
Women presenting to the TBAs without a health passport were advised to seek care at a health facility.
“…there are some women who will come and say I want to start antenatal. We ask her if she has a card/health passport book. If she says no I don’t have a card so we tell her that you should first go to the hospital for antenatal.”
TBAs also felt they had learned how to complete the logs. TBAs interpreted the log as follows:
“…When we find a number [ a number that is written in the health passport book] it means the person is HIV positive… and we take that number and write in the log. When a woman is negative we show a light in the log. On the woman who is HIV positive, there is a woman who is taking Nevirapine…”
“…and here where there is an ambulance, it is when she is referred to the hospital to deliver there.”
The TBAs felt that after the training they were following infection prevention measures when conducting deliveries as compared to the period before the training. During the baseline assessment, many inappropriate infection prevention problems were noted. Later, most TBAs reported avoiding sharing of delivery kits, wearing protective wear such as gloves and shoes, and washing hands with soap before and after delivery. One TBA said,
“We start by washing our hands when the woman comes then we wear gloves…and when the baby is born we make sure the fluids that discharge from the mother’s body should not get to the baby…and on the part of the tools, they have to be hers alone not of somebody who delivered…using like razor that you have used on somebody then when someone comes you use the same things, no.”
They also reported proper disposal of placenta and birthing kits. One TBA said, “We tell her not to reuse the paper; we tell her to do another way that is if the paper is dry she should burn it… We throw all her trash in the toilet.”
TBAs also performed other roles such as educating women to access timely antenatal care and deliver in health facilities; encouraging women to take an HIV test; and promoting couples counseling and nutrition counseling, especially for HIV positive women.
The TBAs felt that PMTCT training was the most important incentive to participate in PMTCT service delivery. They felt the training they received had enhanced their roles because they used the knowledge and skills to educate their communities on HIV and AIDS issues. The TBAs requested on-going refresher trainings on PMTCT to reach women and infants lacking access to PMTCT services. TBAs also mentioned supervision and report review as an incentive to improve work performance.
TBAs requested a stock of NVP for both mothers and infants to be used when the mother did not have her supply. However, one TBA said that stocking medicine would be a setback to promoting hospital delivery, stating that:
…”. If women see that we have a lot of medication they will not go to the hospital. They will say we have a big clinic; we have women [meaning TBAs] to help us to deliver.”
Barriers to accessing PMTCT services
TBAs mentioned a number of barriers to PMTCT access: disclosure, health care worker attitudes, and transport.
Disclosure
TBAs’ failed to determine whether a woman took NVP or not when she did not disclose her HIV status to the TBA. TBAs described that some pregnant women did not bring their health passport thereby presenting a challenge to confirm HIV status and to determine if whether NVP was needed or not. The TBAs mentioned that:
“Since the training we meet such types of women who are HIV positive, they come but they hide their status. Did you take medication (nevirapine)? They ask you what medication? I tell them the pill which one takes when labor starts. They would say no, I didn’t receive. I look in their book and ask what are you hiding? They wrote here that you should take this medication when labor starts so what are you hiding? Ah I did not receive… saying that she didn’t take it, she was not given. Refusing, hiding… but I tell them that they are hiding, lying that they didn’t receive the medication…”
“A certain woman came here. I checked in her book. She was HIV positive but when I asked her she refused.”
Bad attitude of health workers
TBAs reported that a woman’s preference to deliver with a TBA instead of at a health facility was a barrier to accessing PMTCT services. TBAs reported that women did not always reach the health facilities when referred. They suggested that negative attitudes of nurses and doctors towards pregnant women were reasons why women continued to avoid health facility services. Additionally, pregnant women were left unattended and delivered alone in the absence of health professionals. One described that “going to the hospital was bad because they [meaning pregnant women] were saying that the doctors leave you in labour, they go outside and chat. People from the village will want to push once they arrive”.
Transportation
TBAs reported that lack of transportation is a constraint hindering pregnant women from presenting to a health facility during labor. Some health facilities are located 8 to 15 km away from their communities, presenting a challenge to facility delivery. TBAs said that when a request for an ambulance was made, health officials favored some TBAs compared to others. Similarly, they said that “In our areas there’s not even one. But we hear that it is only TBA12 that you sent the ambulance so we say what is the difference between us and her? We will have accidents in our communities.” TBAs lamented using their money to hire taxis, describing their work as voluntary. While TBAs reported referring women to health facilities, they did not always know if referred women successfully arrived or went to another TBA instead.
Discussion
In Malawi, TBAs continue to play a significant role in the delivery of maternal health services. We have shown that with training and supervision TBAs have the potential to be part of the PMTCT program in Malawi. Training helped TBAs to understand and participate in PMTCT activities. Barriers to success included failure of women to disclose their status to the TBA, lack of appropriate transport for referrals to the clinic both pre and post-delivery, and perceived negative attitudes of health workers at health facilities toward TBAs and their clients. Our findings suggest that if TBAs receive ongoing training and supervision, they could perform safer deliveries and identify women who need referral and treatment.
Training and the provision of birth kits resulted in a reported increase in safe deliveries with improved infection control practices. Consistent with our finding, another TBA programme in Malawi concluded that empowering TBAs through supervision and provision of supplies helped them to comply with the requirement of ensuring infection free deliveries1. Assisting TBAs to adopt more modern delivery services, with an emphasis on infection control and early identification of high risk situations requiring referral, may allow more HIV positive women to be reached11–12.
Both supervision and focus group discussions demonstrated that TBAs were able to learn to use the TBA data collection log. The pictures and symbols on logs, which represented different PMTCT activities, were easily understood and interpreted by many TBAs. TBAs did not find documentation of their work as a challenge as they were already using pictorial records for charting6. Similar simplified antenatal cards have been used in other setting with good understanding by other illiterate TBAs13. Since many TBAs have low levels of literacy and some may not be interested in further training, attention must be given to making instructions relevant to the local culture in which TBAs practice14. The finding that TBAs checked for a documented HIV status (from antenatal cards/health passport books) and asked women if they had taken NVP during labour demonstrates that TBAs may have the potential to facilitate drug uptake and adherence. While Malawi has now moved to universal ART for all pregnant women rather than single dose NVP, TBAs can still play a role in identifying positive clients and counseling on the importance of ART adherence for PMTCT.
Disclosure issues may have affected NVP uptake. TBAs did not help all HIV positive women and exposed babies to receive NVP. Only 51% of HIV positive women and 27% of HIV exposed infants had taken NVP. TBAs mentioned that some women refused to disclose their status while some had forgotten to bring their medication. While our 27% rate was sub-optimal, in a previous study conducted in Malawi, none of the babies born at home received NVP suggesting some improvement from engaging TBAs in the process. HIV positive women experience issues of fear, non-disclosure, discrimination, and stigma that act as barriers to deliver in hospitals or return to hospitals to receive NVP syrup for their babies8.
Lack of emergency transport at the TBAs home barred women from accessing PMTCT services at the health facility. TBAs mentioned the shortage of ambulances and drivers delayed the referred women from reaching health facilities. Most health facilities are far from the communities, making it difficult to utilize facilities at the time of labor and delivery. Distance, money, and being sick were some of the common reasons for not delivering in the hospital8. Though these reasons are not directly related to HIV, the issue of transport may have an implication for mothers and their infants not reaching health facilities to access NVP.
Negative attitudes of health workers were mentioned by the TBAs as a reason women did not report to the health facility. This finding concurs with findings in Kenya, in which women continued to prefer TBAs due to disrespectful attitudes of health care workers at the health facilities11. In Lilongwe, Malawi, women preferred TBAs because TBAs were more respectful9. While we did not discuss health care worker attitudes with the women seeking TBA services, understaffing at health centers in Malawi is common, suggesting the potential for overworked and stressed health workers. Until staffing deficiencies and a provision for an emergency transport system are addressed, strategies that incorporate and empower TBAs may be a feasible and reasonable interim solution.
Our study had both limitations and strengths. Our quantitative analysis was limited to evaluation of the TBA logs and is purely descriptive. We did not evaluate the impact of our intervention on the number of facility deliveries as our overall number of involved TBAs was small relative to those operating in the community. We did not have sufficient information to evaluate individual TBA performance because our sample size for each TBA was small. We did not interview mothers in the TBA programme and relied on the perception of the TBAs regarding mothers’ motivations. We were not able to track the outcome of all referrals because we did not have a data linking system. Our intervention was conducted when single dose NVP was the primary PMTCT modality in Malawi and more complicated regimens were not assessed. However, our findings regarding understanding of the logs and referral requirements are valid regardless of PMTCT regimen. Lastly, our findings are relevant to TBAs who met our eligibility criteria and may not be applicable to other settings or among TBAs who have less formal training than those included in our program.
Malawi has switched from single dose NVP prophylaxis, with the mother taking a dose at the onset of labor and the infant receiving a dose within 72 hours of delivery. Currently, Malawi uses the WHO Option B+ guidelines which provide all HIV positive women with three antiretroviral drugs for life. While this is the ideal treatment for women, uptake will not be 100%. Women will continue to deliver outside the hospital, making TBA involvement in PMTCT still relevant6.
Conclusion
If trained and supervised, TBAs can identify and reach women and babies who are in need of HIV services. Our findings show that the TBAs managed to identify HIV infected women and administer NVP indicating that they have the potential to implement PMTCT. However, training, supervision, a referral linking system and emergency transport are necessary requirements to optimize the involvement of TBAs.
Acknowledgments
This study was funded by the Elizabeth Glaser Pediatric AIDS foundation Operations Research award. We are indebted to the traditional birth attendants for voluntarily participating and contributing to this research; without them the research would not have been possible. Also we thank the PMTCT teams at Bwaila Hospital and Kawale, Area 18 and Area 25 Health Centers, as well as the Lilongwe District Hospital Office for their technical support towards the implementation of this research.
Footnotes
Contribution of Authors
All authors contributed extensively to the work presented in this manuscript. Francis Martinson, Irving Hoffman, Charlie van der Horst, Mina Hosseinipour, Innocent Mofolo, Christopher Sellers, R.C. Nakanga developed the concept and designed the study. Gloria Hamela, Charity Kabondo, Chifundo Zimba, Esmie Kamanga and Bertha Bulla collected and analyzed data. Charity Kabondo, Gloria Hamela, Mina Hosseinipour, Charlie van de Horst and Irving Hoffman worked tirelessly to prepare the manuscript. Clara Lee, Tapiwa Tembo, Gloria Hamela, Mina Hosseinipour, Irving Hoffman edited the paper. All authors also had provided an approval of this manuscript.
References
- 1.Bisika T. The Effectiveness of the TBA Programme in Reducing Maternal Mortality and Morbidity in Malawi. East African Journal of Public Heath. 2008;5(2):103–110. [PubMed] [Google Scholar]
- 2.Ministry of Health. National Sexual and Reproductive Health and Rights Policy. Lilongwe: 2009. [Google Scholar]
- 3.National Statistical Office (NSO) [Malawi] and ORC Macro. Malawi Demographic and Health Survey. Calverton, Maryland: NSO and ORC Macro; 2004. [Google Scholar]
- 4.National Statistical Office (NSO) [Malawi] and ORC Macro. Malawi Demographic and Health Survey. Calverton, Maryland: NSO and ORC Macro; 2010. [Google Scholar]
- 5.National AIDS Commission (NAC) HIV/AIDS Report in Malawi 2006. NAC; 2006. [Google Scholar]
- 6.Lippmann QK, Mofolo I, Bobrow E, Maida A, Kamanga E, Pagadala N, Martinson F, Van der Horst C, Hosseinipour M, Hoffman I. For the Call to Action Team. Exploring the Feasibility of Engaging Traditional Birth Attendants in a Prevention of Mother to Child HIV Transmission Program in Lilongwe, Malawi. [PMC free article] [PubMed] [Google Scholar]
- 7.Biggar RJ, Miotti PG, Taha TE, Mtimavalve L, Broadhord R, Justesen A, et al. Perinatal intervention trial in Africa: Effect of birth canal cleansing intervention to prevent HIV transmission. Lancet. 1996;347:1647–1650. doi: 10.1016/s0140-6736(96)91486-5. [DOI] [PubMed] [Google Scholar]
- 8.Kasenga F, Hurtig AK, Emmelin M. Home Deliveries: Implications for adherence to nevirapine in a PMTCT programme in rural Malawi. AIDS Care. 2007;19(5):646–652. doi: 10.1080/09540120701235651. [DOI] [PubMed] [Google Scholar]
- 9.O’Gorman DA, Nyirenda LJ, Theobald SJ. Prevention of mother-to-child transmission of HIV infection: Views and perceptions about swallowing nevirapine in rural Lilongwe, Malawi. BMC Public Health. 2010;10:354. doi: 10.1186/1471-2458-10-354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Perez F, Muffih TP. The Use of Traditional Birth Attendants in HIV Care. In: Marlink RG, Teitelman ST, editors. From the Ground Up: Building Comprehensive HIV/AIDS Care Programs in Resource-Limited Settings. Washington, DC: Elizabeth Glaser Pediatric AIDS Foundation; 2009. http://ftguonline.org. [Google Scholar]
- 11.Izugbara C, Ezeh A, Fotso JC. The persistence and challenges of homebirths: perspectives of traditional birth attendants in urban Kenya. Health Policy Plan. 2009;24:36–45. doi: 10.1093/heapol/czn042. [DOI] [PubMed] [Google Scholar]
- 12.Msaky H, Kironde S, Shuma J, Nzima M, Mlay V, Reeler A. Scaling the frontier: traditional birth attendant involvement in PMTCT service delivery in Hai and Kilombero districts of Tanzania. International Conference on AIDS 2004: Bangkok: Thailand. 2004 [Google Scholar]
- 13.Chabot HT, Rutten AM. Use of antenatal cards for literate health personnel and illiterate traditional birth attendants: an overview. Trop Doct. 1990;20(1):21–24. doi: 10.1177/004947559002000107. [DOI] [PubMed] [Google Scholar]
- 14.Madhivanan P, Kumar BN, Adamson P, Krupp K. Traditional Birth Attendants lack basic information on HIV and safe delivery practices in rural Mysore, India. BMC Public Health. 2010;10:57. doi: 10.1186/1471-2458-10-570. [DOI] [PMC free article] [PubMed] [Google Scholar]


