Abstract
Background
Hospital medicine has grown rapidly, but hospital leaders’ perceptions of current and future drivers of hospitalist growth are unknown.
Objective
To determine hospital executives’ perceptions of factors leading to hospitalist implementation and their vision for hospitalists’ work roles.
Setting
Non-federal, acute care hospitals in California.
Participants
California hospital leaders (e.g., chief executive officers).
Intervention
Cross-sectional survey from 2006-07.
Measurements
We asked California hospital leaders whether their hospitals had a hospitalist service and the prospects for growth. In addition, we examined factors responsible for implementation, scope of hospitalists’ practices, and need for additional certification as perceived by hospital leaders.
Results
We received surveys from 179 of 334 hospitals (response rate of 54%). Of the 64% of respondents that reported the use of hospitalists, none intended to decrease the size of their hospitalist group, and 57% expected growth over 2 years. The most common reasons for implementing a hospitalist program were to care for uncovered patients (68%) and improve cost/length of stay (63%). Respondents also indicated that demand from other physicians was an important factor. Leaders reported that hospitalists provide a wide range of services, with a majority involved in quality improvement projects (72%) and medical co-management of surgical patients (66%). Most leaders favor additional certification for hospitalists.
Conclusions
There is widespread adoption of hospitalists in California hospitals, with an expectation of continued growth. The drivers of the field’s growth are evolving and dynamic. In particular, attentiveness to quality performance and demand from other physicians are increasingly important reasons for implementation.
Keywords: Attitude of Health Personnel, Delivery of Healthcare, Hospitalists / Organization, Hospitalists / Trends, Physician’s Practice Patterns
Introduction
In the late 1990s, hospitalist systems grew rapidly in an environment where cost containment was paramount, complexity of patients increased, and outpatient practices experienced increasing productivity and efficiency pressures.1-5 While the healthcare delivery environment has changed significantly since that time,6-8 hospitalists have continued to become more common. In fact, the field’s present size of more than 25,000 has already exceeded early projections, and there are no signs of slackening demand.9-11
Growth has been attributed to primary care physicians’ increasing focus on outpatient care, hospitals’ response to financial pressures, and the need to facilitate improved communication among various hospital care providers.12-16 Hospital leadership has played a similarly important role in fueling the growth of hospitalists, particularly since the vast majority of programs require and receive institutional (usually hospital) support.17 However, the factors that continue to influence leaders’ decisions to utilize hospitalists and the current and future needs that hospitalists are fulfilling are unknown. Each of these factors is likely to impact growth of the field, as well as the clinical and organizational identity of hospitalists. In addition, an understanding of the “market demand” for hospitalists’ competencies and the roles they play in the hospital may inform any changes in board certification and training for hospitalists.11,18-21
To gain a more complete understanding of a key part of the engine driving the growth of hospitalists, we performed a cross-sectional survey of California hospital leaders who were involved with the funding or administration of their hospitalist groups. Our survey aimed to understand: 1) the prevalence of hospitalist groups in California hospitals, 2) hospital leaders’ rationale for initiating the use of hospitalists, 3) the scope of clinical and non-clinical practice of hospitalists, and 4) hospital leaders’ perspective on the need for further training and/or certification.
Methods
Sites and Subjects
We targeted all non-federal, non-specialty, acute care hospitals in California (N = 334) for this survey. We limited our survey to California in order to maximize our local resources, and to improve implementation of and response to the survey. Additionally, California’s size and diversity gives it disproportionate impact and potential generalizability. At each site, we focused our efforts on identifying and surveying executives or administrative leaders involved in organizational and staff decisions, specifically the decision whether or not to hire and/or fund a hospitalist program and potentially direct their activities (described in more detail below). The University of California, San Francisco Committee on Human Research approved the research protocol.
We identified hospital leaders at each site by merging information from multiple sources. These included the American Hospital Association database, the California Hospital Association, the Hospital Association of Southern California (HASC), the California Health Care Safety Net Institute, and individual hospital websites.
Survey Development
Our survey was based upon instruments used in previous research examining hospital medicine group organizational structure15,22 and enhanced with questions developed by the research team (ADA, EEV, RMW). The survey was pre-tested in an advisory group of five hospital Chief Executive Officers (CEOs), Chief Medical Officers (CMOs), and Vice Presidents for Medical Affairs (VPMAs) from sites across California. Based on their input, we removed, edited, or added questions to our survey. This advisory group also helped the research team design our survey process.
Our final survey defined a “hospitalist” as a physician who spends all or the majority of his or her clinical, administrative, educational, or research activities in the care of hospitalized patients.4 We collected data in four areas. 1) We asked hospital leaders to confirm the presence or absence of at least one hospitalist group practicing within the surveyed hospital. We also asked for the year the first hospitalist group began practicing within the specified hospital. 2) We asked hospital leaders to indicate, among a pre-specified list of 11 choices, the reason(s) they implemented a hospitalist group at the surveyed hospital. Surveyed categories included: a) care for uncovered patients, b) improve costs, c) improve length of stay, d) improve emergency department throughput, e) primary care provider demand f) improve patient satisfaction, g) improve emergency room staffing, h) quality improvement needs, i) specialist physician demand, j) overnight coverage, and k) surgical co-management. Due to the close relationship between cost and length of stay, we combined these two categories into a single category for reporting and analysis. This resulted in 10 final categories. We asked leaders who did not identify a practicing hospitalist group about the likelihood of hospitalists practicing at their hospital within the next five years, and the reason(s) for future implementation. 3) We asked leaders to describe the services currently provided among a pre-specified list of clinical care duties that go beyond the scope of inpatient general internal medicine (e.g., surgical co-management, rapid response team leadership) as well as non-clinical duties (e.g., quality improvement activities, systems project implementation). If hospitalists did not currently provide the identified service, we asked leaders to indicate if they would be inclined to involve hospitalists in the specified service in the future. 4) Finally, we asked hospital leaders their opinion regarding the need for further training or certification for hospitalists.
Survey Protocol
We administered surveys between October 2006 and April 2007. We initially emailed the survey. We repeated this process for non-respondents at intervals of 1-3 weeks after the initial emailing. Next, we sent non-respondents a physical mailing with a reminder letter. Finally, we made phone calls to those who had not responded within 4 weeks of the last mailed letter. We asked survey recipients to respond only if they felt they had an adequate working knowledge of the hospitalist service at their hospital. If they did not feel they could adequately answer all questions, we allowed them to forward the instrument to others with a better working knowledge of the service.
Because we allowed recipients to forward the survey, we occasionally received two surveys from one site. In this case, we selected the survey according to the following prioritization order: 1) Chief Executive Officers (CEOs)/Chief Operating Officers (COOs), 2) Chief Medical Officers (CMOs), 3) Vice Presidents of Medical Affairs (VPMAs), 4) other vice presidents (VPs) or executive/administrative leaders with staff organization knowledge and responsibilities.
Hospital Descriptive Data
We obtained hospital organizational data from the California Office of Statewide Health Planning and Development’s (OSHPD) publicly available Case Mix Index Data, hospital Annual Financial Data, aggregated Patient Discharge Data, and Utilization data from 2006.23 Organizational characteristics included hospital size, location, profit status, payor mix, and diagnosis-related group based case-mix. Teaching status was determined from the 2005 American Hospital Association database. Membership status in California’s voluntary quality reporting initiative, California Hospital Assessment and Reporting Taskforce (CHART), was publicly available at http://www.calhospitalcompare.org.
Statistical Analyses
We performed univariable analyses to characterize survey respondents, followed by bivariable analyses to compare hospital characteristics and patient mix of responding and non-responding hospitals. We used similar methods to characterize respondent hospitals with and without at least one hospitalist group. We compared continuous data with the Student’s t-tests or Mann-Whitney tests as appropriate and categorical data with chi-square tests.
We then summarized the number of times a specific rationale was cited by hospital leaders for implementing a hospitalist group. Among hospitals that did not have a hospitalist system in place at the time of the survey, we asked if they were planning on starting one within the next five years. For these hospitals, we used content analysis to summarize open-ended responses in order to understand factors that are currently influencing these hospital leaders to consider implementing a hospitalist group.
Next, we aimed to understand what clinical and non-clinical roles hospitalists were performing in hospitals with established hospitalist programs. Clinical activities were divided into general clinical areas, triage/emergency-related, or administrative activities. First, we summarized the number and percent of programs performing each clinical and non-clinical activity. This was followed by logistic regression analyses to assess whether the time period that hospitalist groups began practicing or additional hospital characteristics predicted the performance of individual hospitalist activities. To guard against overfitting of models, analyses were limited to rationales that were cited a minimum of 50 times.24 Hospital factors were selected on the basis of face validity and advisory group input and included hospital bed size, ownership status (public vs. private), teaching status, and membership status in CHART. We divided the year of hospitalist program implementation into three time periods: 1) before 2002, 2) between 2002-04, and 3) 2005 or later.
Finally, we described the percentage of hospitals that favored having their hospitalist group(s) perform each of the identified clinical or non-clinical activities, if they were not already performing them. The institutional review board of the University of California, San Francisco approved the study. We performend analyses with statistical software (Stata Version 9.2, College Station, TX).
Results
Respondent Characteristics
We received 200 survey responses. Of those, we excluded 15 duplicates (e.g., a survey from both the CEO and VPMA) and six responses identified as coming from hospitalists who did not have a leadership position in the hospital. Thus, the final hospital leader survey response rate was 54% (N=179). Forty-six percent of the final responses were from CEOs or COOs; 37% of responses were from CMOs, VPMAs, and medical directors; and the remaining 17% of responses were from other VPs or administrative directors.
Respondent and non-respondent hospitals were statistically similar in terms of teaching status and participation in CHART. Hospital patient census, intensive care unit census, payer mix, and diagnosis-related group based case-mix revealed no statistically significant differences between groups (p > 0.05). Respondent hospitals tended to have fewer beds and were more often for-profit compared to non-respondents (p = 0.05 and p < 0.01, respectively).
Descriptive Characteristics of Hospitals with Hospitalists
Sixty-four percent (N = 115) of hospital leaders stated that they utilized hospitalists for at least some patients. Hospitals with hospitalists were statistically more likely (P < 0.05) to be larger, a major teaching hospital, or a member of a voluntary quality reporting initiative (Table 1).
Table 1.
Distribution of Hospitals With and Without at Least One Identified Hospitalist Group among Respondent Hospitals
| Variable | Hospitals Without Hospitalists = 64, N (%) |
Hospitals With Hospitalists = 115, N (%) |
P-value* |
|---|---|---|---|
| Hospital Size, Total # Beds | |||
| 0-99 | 33 (51.6) | 18 (15.7) | <0.001 |
| 100-199 | 19 (29.7) | 32 (27.8) | |
| 200-299 | 5 (7.8) | 23 (20.0) | |
| 300+ | 7 (10.9) | 42 (36.5) | |
| Hospital Control | 0.12 | ||
| City/County | 8 (12.5) | 7 (6.1) | |
| District | 15 (23.4) | 17 (14.8) | |
| For-Profit | 10 (15.6) | 16 (13.9) | |
| Non-Profit | 31 (48.4) | 71 (61.7) | |
| University of California | 0 (0.0) | 4 (3.5) | |
| Teaching Hospital | 8 (12.5) | 30 (26.1) | 0.03 |
| Member of Voluntary Quality Reporting Initiative |
27 (42.2) | 93 (80.9) | < 0.001 |
P-Values based on chi-square test of statistical independence for categorical data. Totals may not add to 100% due to rounding.
Among all hospitals with hospitalists, 39% estimated that hospitalists cared for at least one-half of admitted medical patients, and 7% stated that hospitalists cared for all patients. Twenty-four percent of respondents were unable to provide a quantitative estimate of the percent of patients cared for by hospitalists. When asked about expectations of growth in the coming year, 57% of respondents with hospitalists expected to see increases in the number of hospitalists at their hospital, and none expected a decrease. Among the 64 respondent hospitals that currently did not have a hospitalist program, 44% (N= 28) of the hospital leaders felt hospitalists would be managing patients in the future. Of those, 93% felt this would occur within the next 2 years.
Reasons for Implementing Hospitalists
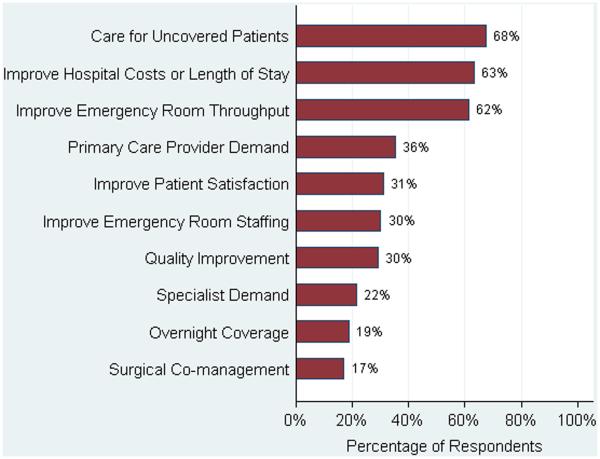
Hospital leaders reported that the most important reasons for implementing a hospitalist model included caring for “uncovered patients” (patients without an identified doctor and/or uninsured) (68%), decreasing hospital costs and length of stay (63%), and improving throughput in the emergency room (62%). We provide additional reasons in Figure 1. In addition, leaders often identified multiple factors in the decision to utilize hospitalists, including demand from primary care doctors, patient satisfaction, and quality improvement. Among the 28 hospitals that currently did not have hospitalists but anticipated that they would soon (data not shown), the need to improve quality was the most commonly cited reason (54% of respondents) for expecting to start a program within 2 years, followed by demand from primary care doctors (46% of respondents).
Figure 1.
Reasons for Implementing a Hospitalist System among Respondent Hospital Leaders with a Hospitalist System (N = 115)
Clinical Practice of Hospitalists and Expectations for Future Growth
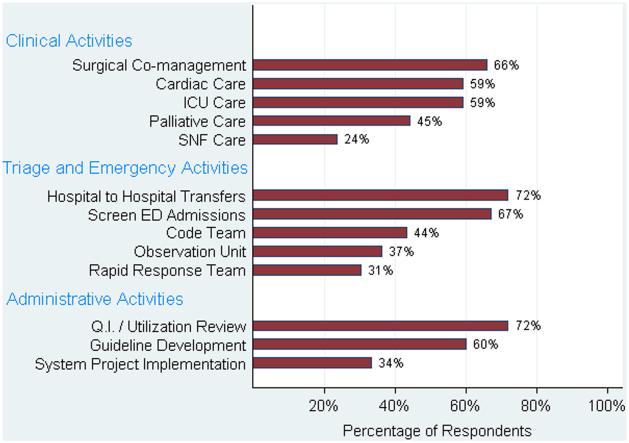
Hospitalists perform a wide array of clinical and non-clinical duties (Figure 2). In addition to general medical care, the most common clinical activities of hospitalists included screening medical admissions from the emergency room for appropriateness of admission and triaging to appropriate level of care (67%), triaging patients transferred from an outside hospital (72%), and co-managing surgical patients (66%). The most common non-clinical activity was participation in quality improvement activities (72%). Multivariable analyses demonstrated that the performance of the most prevalent activities was not usually associated with the year of hospitalist implementation or hospital characteristics. An exception was that newly initiated programs had a statistically significant decreased odds of involvement in clinical guideline development (OR 0.3, 95% CI 0.1 to 0.9) and a trend toward decreased leadership in quality improvement (OR 0.3, 95% CI 0.1 to 1.1). Hospitalists at teaching hospitals had increased odds of managing patient transfers (OR 4.7, 95% CI 1.0 to 21.2), whereas for-profit hospitals had lower odds of screening patients in the emergency room (OR 0.1, 95% CI 0.0 to 0.7).
Figure 2.
Activities Provided by Hospitalists among Respondent Hospitals with Hospitalists (N = 101)
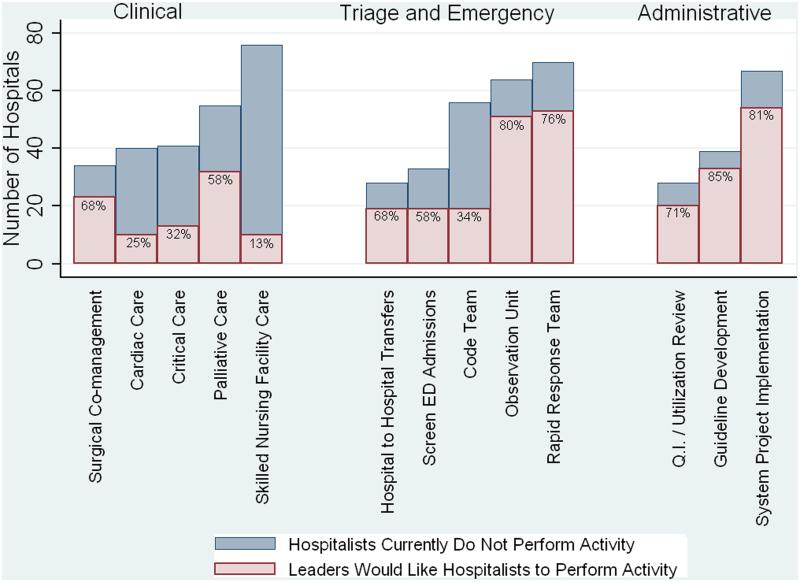
Among those hospitals with hospitalists who were not presently involved in any of the above activities, there was a widespread interest among hospital leaders to have their hospitalist group(s) lead or participate in them (Figure 3). The most commonly cited activities included participation in inpatient clinical guideline development (85%), implementation of system-wide projects (81%) (e.g., computerized physician order entry system), participation on a rapid response team (80%), and caring for patients in an observation unit (80%).
Figure 3.
Activities Hospital Leaders Would Like to Have Implemented by Their Current Hospitalist Group(s), if Not Currently Providing
Training and Certification for Hospitalists
About two-thirds (64%) of hospital leaders with a hospitalist group(s) agreed or strongly agreed that hospitalists should have additional training and/or certification. Seventeen percent were undecided, whereas 11% either disagreed or strongly disagreed, and the remaining 8% did not provide an opinion.
Discussion
Most California hospital leaders reported utilizing hospitalists, and a substantial number of those without a hospitalist service plan to implement one in the next five years. Our data suggest that the number of hospitalists and their roles will continue to expand, with quality improvement activities and participation in clinical roles outside of general medical care being key priorities for future growth. Interestingly, much of this growth may not be catalyzed by past drivers (such as need to contain costs or length of stay) but by increasing need to implement quality and safety initiatives, as well as demand from other physicians. As a result, the field of hospital medicine will grow in numbers and breadth of practice. Defining the “typical” practice of a hospitalist may become more challenging.
Consistent with previous work,11,16 our data suggest widespread adoption of hospitalists. While our data demonstrates that academic hospitals in California were more likely to have hospitalists, it is also important to note that hospitalist systems were widespread across a wide range of hospital sizes and ownership types. The prevalence appears likely to increase in the future. None of the hospitals surveyed planned to eliminate or reduce the size of their programs. Among hospitals without a hospitalist program, 44% (N= 28) reported they were going to implement a hospitalist group within the next 2 years. Future workforce development must consider this growth in order to increase physician supply to meet the demands of hospitalist growth.
Consistent with prior surveys of hospitalists and the healthcare marketplace,13,15,16,25 our survey of hospital leaders suggests that the care of uncovered patients and the goal of improving hospital efficiency are key reasons for implementing hospitalists. Although these are important, we found that hospital leaders have additional intentions when implementing or expanding hospitalist systems, including improving patient satisfaction and quality. Although quality improvement activities were not among the most common reasons that leaders originally implemented programs, the most established programs had increased odds (relative to the most recently implemented programs) of leading quality improvement and clinical guideline activities. This may reflect a natural progression over time for hospitalist groups to develop from a patient-focused clinical role, to one that incorporates responsibilities that increasingly impact the hospital system and organization. The interest in utilizing hospitalists for leadership in quality improvement was widely expressed among those leaders who had yet to utilize hospitalists. Interestingly, this driver remains even as evidence for whether hospitalist practices produce measurable differences in care outcomes is mixed.26,27 Nevertheless, hospital leaders are under increasing pressure to improve quality and safety (driven by public reporting and pay-for-performance initiatives), and many leaders appear to believe that hospitalists will be a key part of the solution.13,28
In addition to quality improvement, continued demand for hospitalists may result from growing clinical demands, including clinical support for medical specialists and surgeons. A majority of leaders acknowledged current or future interest in having hospitalists co-manage surgical patients, with the hope that such practices will improve surgeons’ productivity and clinical outcomes.16,29,30 In addition, hospitalists may address potential shortages in specialty areas. For example, having hospitalists participate in critical care may partly ameliorate the impact of a large national shortage of critical care physicians.12,31 If hospitalists are to assume major roles in the provision of critical care (particularly if not co-managing patients with intensivists), they may require some augmented training in the intensive care unit.
Our results paint a picture of a rapidly expanding field, both in scope and in number. Hospitalists appear to be performing a wide range of clinical, triage, and administrative activities, and there is demand among hospital leadership for hospitalists to take on additional responsibilities. Interestingly, it appears that participation in most clinical and non-clinical activities occur across the spectrum of organizational characteristics, and demand is not limited only to large or academic hospitals. Participation in such a broad array of activities brings into question the need for additional training and certification of hospitalists. While the need for hospitalists to receive additional training has been posited in the past, our data suggest there is a perceived need from the hospital administration as well. This additional training (and subsequent certification) would likely need to encompass many of the practices we have identified as core to hospitalists’ practice. In addition to ensuring adequate training, policymakers will need to consider the supply of physicians necessary to meet the present and, likely, future demand for hospitalists. This is especially important in light of recent evidence of continued decreasing interest in general internal medicine, the main pool from which hospitalists are drawn.32 A shortage of internists is likely to influence expansion plans by hospitals in terms of activities in which leaders ask hospitalists to engage, or the number of hospitalists overall.
Our study has several limitations. First, a substantial number of non-respondents may potentially bias our results. Despite this, we have drawn results across a wide range of hospitals, and the characteristics of responders and non-responders are very similar. In addition, our study exclusively examines the responses of leaders in California hospitals. Although we sampled a large and heterogeneous group of hospitals, these results may not be entirely generalizable to other regions. As a cross-sectional survey of hospital executives, responses are subject to leaders’ recall. In particular, the reasons for implementation provided by leaders of older programs may potentially reflect contemporary reasons for hospitalist utilization rather than the original reasons. Another limitation of our study is our focus on hospital leaders’ reports of prevalence and the clinical/non-clinical activities of hospitalists. Since senior executives often help begin a program but become less involved over time, executives' answers may well underestimate the prevalence of hospitalists and the breadth of their clinical practices, particularly in more mature programs. For instance, hospitalists that are part of an independent practice association (IPA) may provide functions for the IPA group that the hospital itself does not direct or fund. This effect may be more pronounced among the largest hospitals that may be organizationally complex, perhaps making suspect the responses from seven very large hospitals that claimed not to utilize hospitalists. Finally, we collected information regarding the reasons for hospitalist group implementation and the services they provide by means of a pre-specified list of answers. Although a thorough literature review and expert advisory panel guided the development of pre-specified lists, they are by no means exhaustive. As a result, our pre-specified lists may miss some important reasons for implementation, or services provided by hospitalists, that one could identify using an open-ended survey. In addition, in the case of multiple responses from hospital leaders, we gave equal weight to responses. This has the effect of over-estimating the weight of reasons that were less important, while under-estimating the weight of reasons that may have been more important in the decision making process of implementing a hospitalist group.
While non-hospitalist physicians continue to provide a considerable proportion of hospital care for medical patients, hospitalists are assuming a larger role in the care of a growing number of patients in the hospital. The ongoing need to increase care efficiency drives some of this growth, but pressures to improve care quality and demand from other physicians are increasingly important drivers of growth. As the field grows and clinical roles diversify, there must be increased focus placed on the training requirements of hospitalists to reflect the scope of current practice and meet hospital needs to improve quality and efficiency.
Acknowledgment
We acknowledge Teresa Chipps, BS, Department of Medicine (General Internal Medicine and Public Health), Center for Health Services Research, Vanderbilt University, Nashville, TN for her administrative and editorial assistance in the preparation of this manuscript. The research was supported by Grant #05-1755 from the California HealthCare Foundation. Dr. Auerbach was also supported by a K08 research and training grant (K08 HS11416-02) (from the Agency for Healthcare Research and Quality). Dr. Vasilevskis was supported by a Ruth L. Kirschstein National Research Service Award institutional research-training grant T32, the Veterans Affairs Clinical Research Center of Excellence, and the Geriatric Research Education and Clinical Center, Veterans Affairs, Tennessee Valley Healthcare, Nashville, Tennessee. The views expressed in this article do not necessarily represent the views of the Department of Veterans Affairs. Dr. Vasilevskis had full access to all of the data in the study and takes responsibility for the integrity and the analysis of data.
Reference List
- 1.Craig DE, Hartka L, Likosky WH, Caplan WM, Litsky P, Smithey J. Implementation of a hospitalist system in a large health maintenance organization: the Kaiser Permanente experience. Ann Intern Med. 1999;130:355–9. doi: 10.7326/0003-4819-130-4-199902161-00005. [DOI] [PubMed] [Google Scholar]
- 2.Smith PC, Westfall JM, Nichols RA. Primary care family physicians and 2 hospitalist models: comparison of outcomes, processes, and costs. J Fam Pract. 2002;51:1021–7. [PubMed] [Google Scholar]
- 3.Molinari C, Short R. Effects of an HMO hospitalist program on inpatient utilization. Am J Manag Care. 2001;7:1051–7. [PubMed] [Google Scholar]
- 4.Wachter RM, Goldman L. The emerging role of "hospitalists" in the American health care system. N Engl J Med. 1996;335:514–7. doi: 10.1056/NEJM199608153350713. [DOI] [PubMed] [Google Scholar]
- 5.Sox HC. The hospitalist model: perspectives of the patient, the Internist, and internal medicine. Ann Intern Med. 1999;130:368–72. doi: 10.7326/0003-4819-130-4-199902161-00008. [DOI] [PubMed] [Google Scholar]
- 6.Draper DA, Hurley RE, Lesser CS, Strunk BC. The changing face of managed care. Health Aff. 2002;21:11–23. doi: 10.1377/hlthaff.21.1.11. [DOI] [PubMed] [Google Scholar]
- 7.Hall MA. The Death of Managed Care: A regulatory autopsy. J Health Polit Policy Law. 2005;30:427–52. doi: 10.1215/03616878-30-3-427. [DOI] [PubMed] [Google Scholar]
- 8.Robinson JC. The end of managed care. JAMA. 2001;285:2622–8. doi: 10.1001/jama.285.20.2622. [DOI] [PubMed] [Google Scholar]
- 9.Auerbach AD, Chlouber R, Singler J, Lurie JD, Bostrom A, Wachter RM. Trends in market demand for internal medicine 1999 to 2004: an analysis of physician job advertisements. J Gen Intern Med. 2006;21:1079–85. doi: 10.1111/j.1525-1497.2006.00558.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kuo YF, Sharma G, Freeman JL, Goodwin JS. Growth in the care of older patients by hospitalists in the United States. N Engl J Med. 2009;360:1102–12. doi: 10.1056/NEJMsa0802381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kralovec PD, Miller JA, Wellikson L, Huddleston JM. The status of hospital medicine groups in the United States. J Hosp Med. 2006;1:75–80. doi: 10.1002/jhm.82. [DOI] [PubMed] [Google Scholar]
- 12.Manthous CA. Leapfrog and critical care: evidence- and reality-based intensive care for the 21st century. Am J Med. 2004;116:188–93. doi: 10.1016/j.amjmed.2003.08.032. [DOI] [PubMed] [Google Scholar]
- 13.Pham HH, Devers KJ, Kuo S, Berenson R. Health care market trends and the evolution of hospitalist use and roles. J Gen Intern Med. 2005;20:101–7. doi: 10.1111/j.1525-1497.2005.40184.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pham HH, Devers KJ, May JH, Berenson R. Financial pressures spur physician entrepreneurialism. Health Aff. 2004;23:70–81. doi: 10.1377/hlthaff.23.2.70. [DOI] [PubMed] [Google Scholar]
- 15.Auerbach AD, Nelson EA, Lindenauer PK, Pantilat SZ, Katz PP, Wachter RM. Physician attitudes toward and prevalence of the hospitalist model of care: results of a national survey. Am J Med. 2000;109:648–53. doi: 10.1016/s0002-9343(00)00597-0. [DOI] [PubMed] [Google Scholar]
- 16.Pham HH, Grossman JM, Cohen G, Bodenheimer T. Hospitalists and care transitions: the divorce of inpatient and outpatient care. Health Aff. 2008;27:1315–27. doi: 10.1377/hlthaff.27.5.1315. [DOI] [PubMed] [Google Scholar]
- 17.2005-2006 SHM Survey: State of the Hospital Medicine Movement. 2009 Available at: http://dev.hospitalmedicine.org/AM/Template.cfm?Section=Survey&Template=/CM/ContentDisplay.cfm&ContentID=14352 . Accessed March 13.
- 18.Wachter RM. What will board certification be-and mean-for hospitalists? J Hosp Med. 2007;2:102–4. doi: 10.1002/jhm.202. [DOI] [PubMed] [Google Scholar]
- 19.Plauth WH, III, Pantilat SZ, Wachter RM, Fenton CL. Hospitalists' perceptions of their residency training needs: results of a national survey. Am J Med. 2001;111:247–54. doi: 10.1016/s0002-9343(01)00837-3. [DOI] [PubMed] [Google Scholar]
- 20.Glasheen JJ, Epstein KR, Siegal E, Kutner JS, Prochazka AV. The spectrum of community-based hospitalist practice: A call to tailor internal medicine residency training. Arch Intern Med. 2007;167:727–8. doi: 10.1001/archinte.167.7.727. [DOI] [PubMed] [Google Scholar]
- 21.Glasheen J, Siegal E, Epstein K, Kutner J, Prochazka A. Fulfilling the promise of hospital medicine: tailoring internal medicine training to address hospitalists' needs. J Gen Intern Med. 2008;23:1110–5. doi: 10.1007/s11606-008-0646-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lindenauer PK, Pantilat SZ, Katz PP, Wachter RM. Hospitalists and the practice of inpatient medicine: results of a survey of the national association of inpatient physicians. Ann Intern Med. 1999;130:343–9. doi: 10.7326/0003-4819-130-4-199902161-00003. [DOI] [PubMed] [Google Scholar]
- 23.Office of Statewide Health Planning and Development Healthcare Information Division - Data Products. 2009 Mar 13; Available at: http://www.oshpd.ca.gov/HID/DataFlow/HospMain.html.
- 24.Vittinghoff E, McCulloch CE. Relaxing the rule of ten events per variable in logistic and Cox regression. Am J Epidemiol. 2007;165:710–8. doi: 10.1093/aje/kwk052. [DOI] [PubMed] [Google Scholar]
- 25.Berenson RA, Ginsburg PB, May JH. Hospital-physician relations: cooperation, competition, or separation? Health Aff. 2007;26:w31–w43. doi: 10.1377/hlthaff.26.1.w31. [DOI] [PubMed] [Google Scholar]
- 26.Lindenauer PK, Rothberg MB, Pekow PS, Kenwood C, Benjamin EM, Auerbach AD. Outcomes of care by hospitalists, general internists, and family physicians. N Engl J Med. 2007;357:2589–600. doi: 10.1056/NEJMsa067735. [DOI] [PubMed] [Google Scholar]
- 27.Vasilevskis EE, Meltzer D, Schnipper J, et al. Quality of care for decompensated heart failure: comparable performance between academic hospitalists and non-hospitalists. J Gen Intern Med. 2008;23:1399–406. doi: 10.1007/s11606-008-0680-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pham HH, Coughlan J, O'Malley AS. The impact of quality-reporting programs on hospital operations. Health Aff. 2006;25:1412–22. doi: 10.1377/hlthaff.25.5.1412. [DOI] [PubMed] [Google Scholar]
- 29.Huddleston JM, Long KH, Naessens JM, et al. Medical and surgical comanagement after elective hip and knee arthroplasty: a randomized, controlled trial. Ann Intern Med. 2004;141:28–38. doi: 10.7326/0003-4819-141-1-200407060-00012. [DOI] [PubMed] [Google Scholar]
- 30.Roy A, Heckman MG, Roy V. Associations between the hospitalist model of care and quality-of-care-related outcomes in patients undergoing hip fracture surgery. Mayo Clin Proc. 2006;81:28–31. doi: 10.4065/81.1.28. [DOI] [PubMed] [Google Scholar]
- 31.Kelley MA, Angus D, Chalfin DB, et al. The critical care crisis in the United States: a report from the profession. Chest. 2004;125:1514–7. doi: 10.1378/chest.125.4.1514. [DOI] [PubMed] [Google Scholar]
- 32.Hauer KE, Durning SJ, Kernan WN, et al. Factors associated with medical students' career choices regarding internal medicine. JAMA. 2008;300:1154–64. doi: 10.1001/jama.300.10.1154. [DOI] [PubMed] [Google Scholar]