Abstract
Background
There is increased recognition that patients suffer adverse events (AEs) or harm caused by treatments in dentistry, and little is known about how dental providers describe these events. Understanding how providers view AEs is essential to building a safer environment in dental practice.
Methods
Dental providers and domain experts were interviewed through focus groups and in-depth interviews and asked to identify the types of AEs that may occur in dental settings.
Results
The first order listing of the interview and focus group findings yielded 1,514 items that included both causes and AEs. 632 causes were coded into one of the eight categories of the Eindhoven classification. 882 AEs were coded into 12 categories of a newly developed dental AE classification. Inter-rater reliability was moderate among coders. The list was reanalyzed and duplicate items were removed leaving a total of 747 unique AEs and 540 causes. The most frequently identified AE types were “Aspiration/ingestion” at 14% (n=142), “Wrong-site, wrong-procedure, wrong-patient errors” at 13%, “Hard tissue damage” at 13%, and “Soft tissue damage” at 12%.
Conclusions
Dental providers identified a large and diverse list of AEs. These events ranged from “death due to cardiac arrest” to “jaw fatigue from lengthy procedures”.
Practical Implications
Identifying threats to patient safety is a key element of improving dental patient safety. An inventory of dental AEs underpins efforts to track, prevent, and mitigate these events.
Keywords: Adverse event, Dentistry, Never event, Cause, Classification
INTRODUCTION
Medical adverse events are one of the leading causes of death in the US, and those that originate in the hospital setting have enjoyed significant attention.1 There are multiple definitions of adverse events (AE) in medicine.2, 3 In this study, we define AEs as “harm caused to the patient by dental care, regardless of whether it is associated with an error or is considered preventable.” Dentists perform highly technical procedures in complex environments, work in teams, and use a multitude of devices and tools.4–9 However, less is known about the safety of dental care and this gap is troubling because a large proportion (65.5%)7 of the U.S. population goes to the dentist at least once a year. Evidence from case reports in the literature6 as well as a recent analysis of data from the FDA MAUDE database5, which tracks device related issues, confirmed that AEs do happen in the dental office. Examples of reported dental AEs include aspirated crowns8 and lacerations due to the use of high speed handpieces.4
The formal study of patient safety in medicine emerged in the 1990s propelled by the Institute of Medicine (IOM) report “To Err is Human”. The report challenged the US to build a safer healthcare system for the 21st century and great progress has been made in medicine, especially in hospital settings.10 The IOM suggested that safety improvements should encompass three activities: preventing AEs, making AEs visible, and mitigating the effects of AEs.10 However, the dental patient safety literature has mainly focused on managing risk,11 exploring different approaches to improving specific surgical procedures,12 or selection of dental products/materials.13 In our previous work14–16 we have proposed the adoption of The Agency for Healthcare Research and Quality Patient Safety Initiative which incorporates four major elements to address patient safety: (1) Identifying threats to patient safety; (2) Identifying and evaluating effective patient safety practices; (3) Educate, disseminate, implement, and raise awareness; and (4) Monitor threats to patient safety to ensure that a positive safety culture is maintained and a safe environment continues. In order to benchmark the safety culture in dentistry, we previously adapted the extensively validated Medical Office Survey on Patient Safety Culture17, 18 and surveyed providers at 3 academic dental institutions.15 The results showed that the patient safety culture in these settings was sub-optimal across many measures compared with results from outpatient medical offices.
Building on previous research in dental patient safety,19–27 our goal for this study was to contribute to Element 1 of the patient safety initiative by developing an inventory of AEs generated by interviewing dental team members.
METHODS
The research was reviewed and approved by the Human Subject Committees of both participating institutions. We used individual domain expert (DE) and focus groups (FG) interviews to develop a list of adverse events (AE) that may occur in practice. One single investigator conducted all ten of the DE interviews, and a different single investigator conducted each of the six FGs. Calibration occurred during weekly team meetings during the 6-month period leading to the actual interviews.
Individual telephone interviews with domain experts
Individual interviews are effective means of collecting data to describe providers’ perceptions of complex phenomena in health care research.28 Based upon established and emerging specializations in dentistry, we identified ten practice domains: orthodontics, periodontics, endodontics, implant dentistry, oral surgery, prosthodontics, general restorative, radiology, oral pathology and oral medicine. A purposive sample of one DE from each of these domains (total n = 10) was interviewed by telephone for one hour to ensure the inclusion of domain-specific AEs. DEs were identified as associate or full professors who have practiced for more than 10 years in the specific field and published extensively. We employed a qualitative descriptive approach29 used in medical research aimed at describing phenomena.30 Interviews were designed to encourage specialists to reach deep into their personal or vicarious clinical experiences. A standardized interview (Appendix 1) ensured the fidelity of the interview questions posed to each expert (See table 1). Deliberative methods31 were used in both the DE and FG interviews by providing the participants with both the definition of AEs: “harm caused to the patient by dental care, regardless of whether it is associated with an error or is considered preventable”, and a handout of exemplar AEs in dentistry such as “extraction of the wrong tooth”.
Table 1.
Focus Group and Domain Expert Core Interview Questions
Following personal introductions, a review of the purpose of the study, and the ground rules for the focus group, the facilitator reviewed the working definition of adverse events adopted from the literature. At that point, the facilitator asked the five questions listed below. The co-facilitators took notes on the phone calls with Domain experts, and wrote responses on flip charts that were hung in sight of the participants. The questions focused exclusively on listing adverse events. The facilitators were trained keep the focus on naming adverse events.
|
Focus Groups
Focus group methods are an established and efficacious means of observing the experience, opinions and perspectives of a large number of study participants during a relatively brief amount of time. Focus group interviews are widely used in health research to gain insights into people’s perspectives32 and are increasingly used in dental studies seeking a depth of understanding not captured in quantitative approaches with forced choice responses.33–37 The rationale for using a broad spectrum of academic dental providers in the academic setting was that they would be more likely to have direct or vicarious experience with a broad range of AEs than the majority of dental providers such as those in community or private practices. Three mutually exclusive dental constituencies were stratified for the study sample: 1. faculty dentists, 2. dental students and residents, and 3. dental staff who were not dentists. Purposive sampling was used to recruit participants at each of two university-based dental clinics. We used a free listing method25 based upon previous studies aimed at developing inventories of medical issues.26, 27 The FG interview guide (Appendix 1) ensured the fidelity of the interview structure between the six groups. The literature indicates that free Listing methods are designed to capture a saturated list of responses to a single question.38, 39
Data classification approach
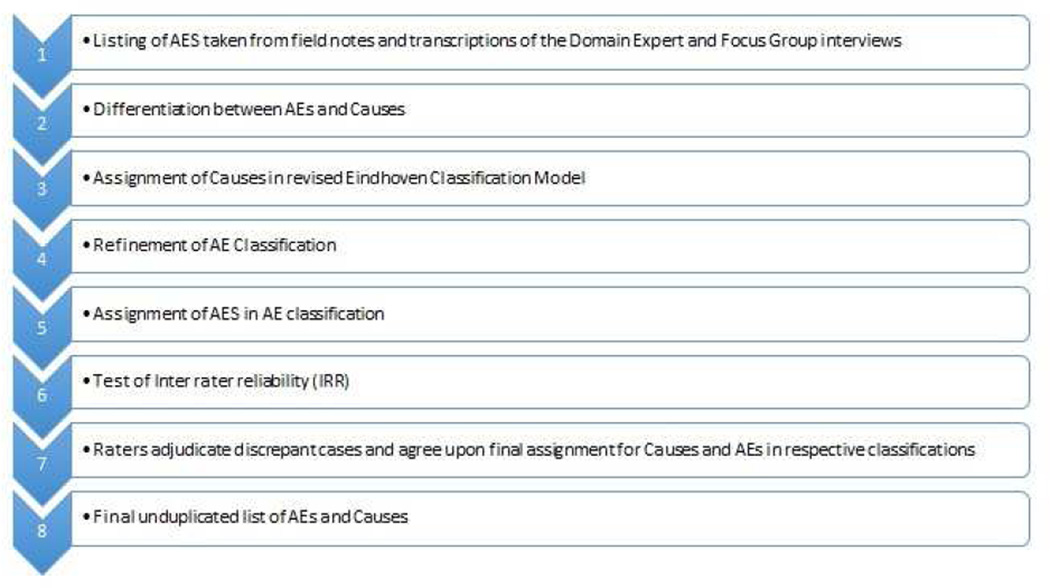
Figure 1 shows the eight steps of the analysis starting with analysis of the verbatim transcriptions and field notes from each interview. Telephone interviews with DE were recorded using a password protected WebEx platform; FGs were recorded using a digital audio recorder. Two research assistants took notes while the facilitator conducted the DE interview. Two research assistants also attended the FGs, one took notes, the other wrote the name of each AE on a flipchart. A research assistant transcribed each of the DE interview and FG recordings. A co-investigator checked every third transcription for accuracy by listening the audio recording while reading the transcription. All notes and flipcharts were transcribed; a qualitative descriptive approach30 allowed only literal documentation of what participants identified as AEs.
Figure 1.
Eight Phases of Analysis for domain expert and focus group findings
To organize the data, each item listed as an AE from the FGs and DE interviews was classified. We discovered that many of the items reported as AEs were actually causes (defined as factors that may lead to harm and not the harm itself)40–42 and not AEs (instances of actual harm that reach the patient). For example: “surgical site infection post operatively” was classified as an AE as it involves harm (infection) to the patient. While, “jumping from chair to chair with the same gloves” was classified as a cause. Two reviewers independently separated AEs from causes.
Items labeled as causes were then further classified. Semantic relationships among items emerged, which led a review of the literature on classifications, and the eventual development of eight categories of causes that we based upon the medical version of the Eindhoven Classification Model.43, 44,45,46 See Table 2.
Table 2.
Classifications of Causes Based on Eindhoven Classification Model: Medical Version (Battles et al. 1998)1 of Adverse Events in Dentistry with Exemplars
| Classification | Responses from respondents (unweighted) |
|---|---|
| Latent Technical |
|
| Latent Organization |
|
| External-based active error | None reported |
| Knowledge-based active error |
|
| Rule-based active error |
|
| Skill-based active error |
|
| Patient-related other |
|
| Unclassifiable other |
|
We next classified AEs. As no AE classification exists for dentistry, we used a retrospective literature review of case reports on dental patient safety and analysis of dental device related AEs of the FDA MAUDE database to develop an initial classification of AEs. Initially, 23 AE categories were identified, which were further collapsed into 12 categories (Table 3). We included quality of care to capture items that were not causes, yet could not be considered an AE. E.g. loss of a temporary crown or bridge once or twice during treatment of a permanent crown or bridge; patient’s lips getting dry and cracked during prolonged procedure; or poor aesthetics.
Table 3.
Dental Adverse Event Classifications * based upon AHRQ classifications for medical errors: http://psnet.ahrq.gov/primer.aspx?primerID=18) with Exemplars
| AE Classification | Responses from respondents (unweighted) |
|---|---|
| Allergy/Toxicity/Foreign |
|
| Body Response |
|
| Aspiration/Ingestion of foreign body |
|
| Infection |
|
| WSPEs Procedure on wrong site Procedure on wrong patient Wrong treatment due to misdiagnosis Other wrong treatment |
|
| Bleeding |
|
| Pain |
|
| Hard tissue damage |
|
| Soft tissue injury/ inflammation |
|
| Nerve injury |
|
| Other systemic complications |
|
| Other Harm |
|
| Quality of Care issue |
|
Two members of the research team with complementary expertise, one oral surgeon and one behavioral scientist, acted as independent coders to test the utility of the categories for both the causes and AEs. The first researcher had considerable experience studying dental patient safety related issues. The second researcher conducted the FGs and had substantial expertise in qualitative data synthesis necessary for AE classification. They independently coded every reported cause into one of the eight categories. The same procedure was followed for each of the reported AEs using the 12 AE categories. Tests for inter rater reliability using Kappa statistical tests were conducted to assess the reliability of the classifications.
A consensus process was used to determine the final classification category in cases of disagreement. We follow Katzenbach’s47 principles of high functioning teams. Reaching consensus was by making sure that all perspectives were heard and understood.
We then combined data from FG and DE interviews to generate an inventory of dental AEs and causes.
RESULTS
A total of 76 informants were asked to list AEs in dentistry; DE (n=10), and FG participants (n=66) during three focus groups in each of the university-based dental schools for a total of six groups that included dental faculty (n=16) dental residents and students (n= 26) and non-dentist clinical staff members (n=24).
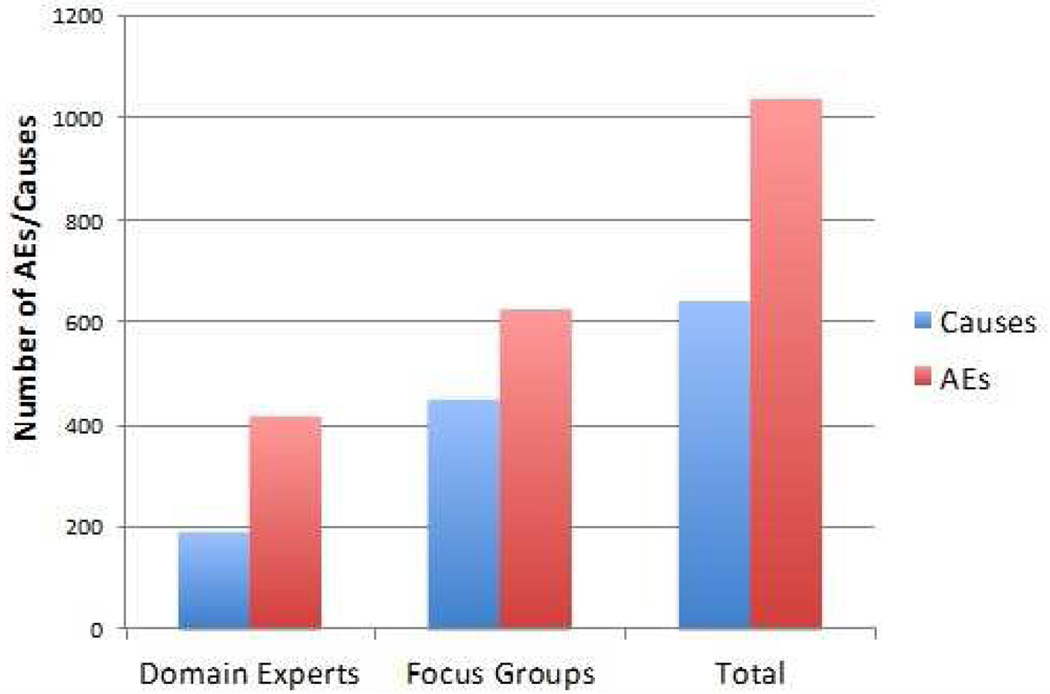
The first order listing of the DE and FG interviews yielded a total 1,514 items reported as AEs. Analysis indicated that respondents confused causes with AEs. The DEs initially identified 524 events as AEs. Of these reported events, we identified that 36% (n=189) were causes rather than AEs. Among the 990 AEs identified by the FGs, 45% (n= 443) were causes. Figure 2 presents the confusion between causes and AEs. In total 747 unique AEs and 540 unique causes were identified (see Appendix 2 and 3).
Figure 2.
Frequency of responses by domain experts and focus groups participants that were classified as Causes and AEs.
An exemplar of the confusion is an item reported as an AE by a FG participant, “Poor home care instructions.” While this might cause an AE, it is not itself an AE. As a cause, however, we coded it as a rule based error (Table 2). Another such example from a DE was, “Failure to have adequate staffing in the room given the level of sedation.” While this cause might lead to disastrous consequences; poor staffing levels by themself are not AEs. This example was coded as a latent organizational error.
Examples of human failures reported by FG and DE participants, include “practicing beyond the scope of training” (rule based error); “obstructing the airway when making an impression” (skill based error); and “failure to recognize decay” or “failure to diagnose” (knowledge based errors). For other examples see Table 2.
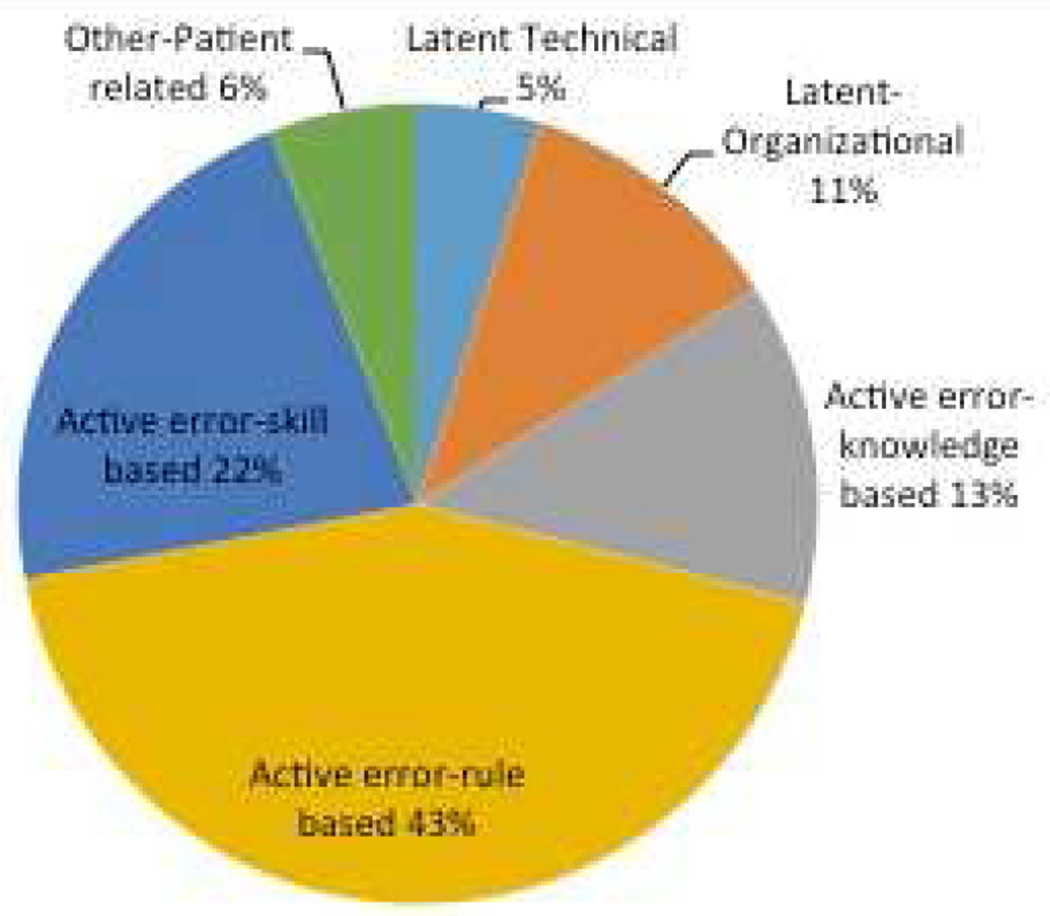
After the adjudication of the discrepant cases, the two independent raters agreed upon the final cause classifications. See Figure 3. Classifications for DE and FG combined show that rule based errors accounted for 43% (n=234) of the reported causes, skill based errors for 22% (n=120), and knowledge based errors for 13% (n=72) of the causes classified as provider related. By contrast, 11% (n=58) of the reported causes were classified as latent-organizational and only 5% (n=24) as latent-technical.
Figure 3.
Based on: TW van der Schaaf, Eindhoven Classification Model for Medical Domain
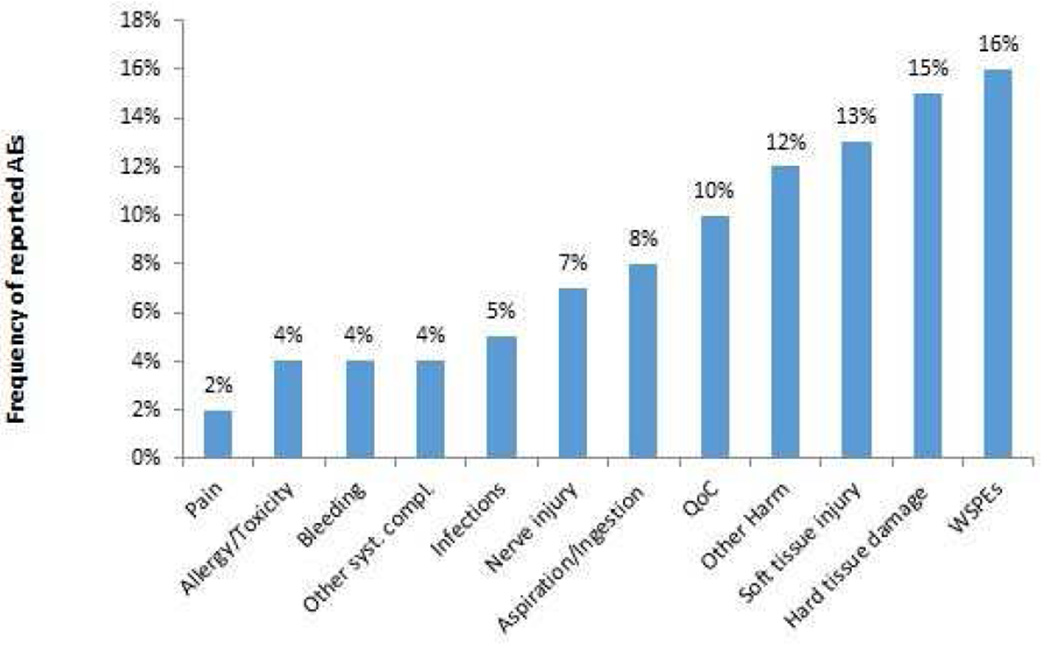
Of the 747 unique AEs included in the final analysis, the most frequently identified AE types in descending order of frequency were “Wrong-site, wrong-procedure, and wrong-patient errors” at 16% (n=116), “Hard tissue damage” at 15% (n=112), “Soft tissue injury” at 13% (n=101), and “Other Harm” at 12% (n=89). And although quality of care issues are not considered AEs, we included those in the analysis as they accounted for 10% (n=75). (Figure 4.)
Figure 4.
Items coded by the Dental AE Classification* (N=747)
*Note that we do not consider Quality of Care (QoC) issues adverse events; those events were included in the analysis as they made up 10% of the overall reported events. WSPEs: Wrong site, wrong patient errors.
Table 4 indicates that the inter-rater reliability between the two independent coders was moderate48 in all instances (DE causes, DE AEs, FG causes, and FG AEs).
Table 4.
Inter-rater reliability (IRR)
| κ | CI | z-score | p-value | |
|---|---|---|---|---|
| DE Causes (n = 189) | 0.41 | 95% (0.32, 0.5) | 11.8 | <0.0001 |
| DE AEs (n=336) | 0.47 | 95% (0.42, 0.53) | 28.1 | <0.0001 |
| FG Causes (n = 443) | 0.41 | 95% (0.35, 0.46) | 16.1 | <0.0001 |
| FG AEs (n=547) | 0.48 | 95% (0.44, 0.53) | 34.5 | <0.0001 |
DISCUSSION
Our results demonstrate that dental team members listed a wide range of harms that might result from dental treatment. After further organizing these events we found that aspiration/ingestion was cited the most, while pain was cited the least. Aspiration or ingestion has been reported to occur infrequently, and of the two, ingestion occurs more often.49 After food, objects of dental origin are second most likely to be aspirated.50 However, these adverse events are difficult to ignore as they require extensive and invasive medical care, are costly and create a potential liability.51 By contrast, providers mentioned mild and manageable pain less frequently, despite the fact that pain follows a range of dental procedures. The quantification of the frequency of pain might increase dental teams’ awareness of a full range of potential AEs in daily practice.
Our study is the first known attempt to interview dental teams and identify an inventory of dental adverse events. We developed a classification system to organize these events in to one category and found that AEs and causes may be classified in multiple categories. As this research is a work in progress we make no claim that the inventory of AEs and causes is complete and their classification is subject to amendment based on additional information and context. The focus groups produced more items than the individual interviews, while the domain experts, identified more direct or vicarious experience with rare, unusual, or never events (i.e. motor loss after TMJ surgery; or unintended displacement of tooth into the infra-temporal fossa). As a result, we collected content rich data that included unlikely, common, and previously overlooked AEs (e.g., extracting the wrong tooth; gingival trauma due to restorative procedure; and sinus perforation). The free listing approach, similar to brainstorming, allowed only for naming AEs, rather than further in depth discussion.
While we did not anticipate the confusion with causes being identified as AEs, these items have provided a rich perspective on how dental providers perceive harm in the dental office and can be used in the future to minimize or prevent AEs from occurring.
An unanticipated finding was the number identified AEs that we classified as quality of care issues. It was based upon the consultation of this project’s Advisory Committee, composed of experts and pioneers in medical adverse events, that we developed the general rule for deciding on what constitutes an AE rather than a quality of care issue; an incident would have to “stand the test of our peers” meaning that our colleagues would most likely agree that the event could indeed be considered an AE. Examples included most often those for which the actual harm was not easily identifiable or “defensible to our peers”, such as esthetic issues after treatment, a failed provisional crown, or under fill of an endodontic treated canal.
There are clear advantages for the implementation of a standardized categorization of dental AEs. It allows for the development of registries, and thus the ability to identify threats to patient safety; raises awareness and monitors threats to patient safety; and allows for future identification and evaluation of patient safety practices.
Some limitations exist in our research. Our study involved two academic dental institutions so we hope to expand the work to a broader range of dental practices in the future. Single DEs in each of the ten practice domains are not a representative sample but this approach allowed us to capture domain specific AEs. For the purpose of clarity, we distributed a working definition of AEs and a short list of AE examples to the DE and FG participants prior to commencing the interviews. Items on the list were not included in the data that we reported unless the participants restated them. While this may have compromised the free listing, it provided a clear message what constituted an AE.
It is possible that a future study population might identify additional items. The purposive sample of ten DEs may reflect only individuals’ perspective of dental AEs. We expect that this type of non-probability sampling does in fact introduce some degree of bias.52,53 While the non-probability sample in the DE interviews and FGs is a potential source of bias, we used the purposive sampling technique in order to reach participants who would be more likely to have greater knowledge of AEs than other dental providers. Further, despite extensive calibration efforts, two reviewers coding AE data into the twelve classifications (See Table 3) were only able to reach moderate agreement, indicating ambiguity inherent to classifying events. In future work we look forward to further applying and expanding this initial list of AEs; determining how frequently these AEs occur in practice and how we can efficiently detect them.
CONCLUSION
Dental providers identified a large and diverse array of dental incidents that were divided into causes of harm, adverse events that produce patient harm and quality of care issues. Our results demonstrate that a classification system such as the one developed in this study may be a viable approach to increase dental providers awareness, and to think proactively, about the full range of harm that patients may experience as a result of dental treatment. This study contributes to an emerging culture of patient safety in dental medicine.
Supplementary Material
Acknowledgments
This research was supported in part by an NIDCR 1R01DE022628-01A1 award. We greatly appreciate the contribution of the Dental Safety Advisory Committee for this project, whose members include: Drs. Lucien Leape, Ana Karina Mascarenhas, Roger Resar, Mike Cohen, Debora Simmons, Eric Thomas, John Valenza, Joan Ash and Ms. Linda Kenney.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
DISCLOSURE
None of the authors reported any disclosures.
None of the authors declare any conflict of interest, financial or other.
Statement of Responsibility
The manuscript has been read and approved by all authors and represents honest work. Below, please find the contribution of each of the authors to this manuscript:
RR conceptualized the project with EK and MW and developed the scientific grant proposal; PM and MW developed the scripts for the domain expert interviews and focus groups; PM facilitated the focus groups; JW conducted the domain expert interviews; PM conducted the analysis of the verbatim transcriptions and field notes from the domain expert interviews and the focus groups: JE and MK assisted with the focus groups and initial data preparation; EK developed the AE classification and the revised Eindhoven classification for causes. PM and EK adjudicated the incidents into causes and adverse events and adjudicated the causes and AEs further into separate classifications. JW, RV, MK, JK, VD, NH, DS and KK further refined the AE classification. AY performed all statistical analyses; EK and PM drafted the manuscript that was reviewed and edited by all authors.
REFERENCES
- 1.Kizer KW, Blum LN. Safe Practices for Better Health Care. In: Henriksen K, Battles JB, Marks ES, Lewin DI, editors. Advances in Patient Safety: From Research to Implementation. Vol. 4. Rockville (MD): 2005. [Google Scholar]
- 2.Brennan TA, Leape LL, Laird NM, et al. Incidence of adverse events and negligence in hospitalized patients. Results of the Harvard Medical Practice Study I. N Engl J Med. 1991;324(6):370–376. doi: 10.1056/NEJM199102073240604. [DOI] [PubMed] [Google Scholar]
- 3.Resar R Outpatient Adverse Event Trigger Tool. Cambridge MA: Institute for Healthcare Improvement (in association with Kaiser Permanente and Baylor Health Care System); 2006. [Accessed 4/11/2016]. " http://www.ihi.org/resources/Pages/Tools/OutpatientAdverseEventTriggerTool.aspx". [Google Scholar]
- 4.Dhanda J, Thomas M, Kheraj A. High speed laceration. Br Dent J. 2008;204(7):352. doi: 10.1038/sj.bdj.2008.256. [DOI] [PubMed] [Google Scholar]
- 5.Hebballi NB, Ramoni R, Kalenderian E, et al. The dangers of dental devices as reported in the Food and Drug Administration Manufacturer and User Facility Device Experience Database. J Am Dent Assoc. 2015;146(2):102–110. doi: 10.1016/j.adaj.2014.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Obadan E, Ramoni RB, Kalenderian E. Lessons Learned from Dental Patient Safety Case Reports. Journal of the American Dental Association. 2015;146(5):318–326. doi: 10.1016/j.adaj.2015.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.The Henry J. Kaiser Family Foundation Percentage of Adults Who Visited the Dentist or Dental Clinic within the Past Year. [Accessed 04/17/2015];2012 " http://kff.org/other/state-indicator/percent-who-visited-the-dentistclinic/". [Google Scholar]
- 8.Weiman MM, Weiman DS, Lingle DM, Brosnan KM, Santora TA. Removal of an aspirated gold crown utilizing the laparoscopic biopsy forceps: a case report. Quintessence Int. 1995;26(3):211–213. [PubMed] [Google Scholar]
- 9.Pinsky HM, Taichman RS, Sarment DP. Adaptation of airline crew resource management principles to dentistry. J Am Dent Assoc. 2010;141(8):1010–1018. doi: 10.14219/jada.archive.2010.0316. [DOI] [PubMed] [Google Scholar]
- 10.Institute of Medicine. To Err is Human: Building a Safer Healthcare System. Washington, D.C.: National Academy Press; 2000. [Google Scholar]
- 11.Chambers DW. Risk management. The Journal of the American College of Dentists. 2010;77(3):35–45. [PubMed] [Google Scholar]
- 12.Lopez-Cedrun JL. Implant rehabilitation of the edentulous posterior atrophic mandible: the sandwich osteotomy revisited. The International journal of oral & maxillofacial implants. 2011;26(1):195–202. [PubMed] [Google Scholar]
- 13.Al-Nawas B, Bragger U, Meijer HJ, et al. A Double-Blind Randomized Controlled Trial (RCT) of Titanium-13Zirconium versus Titanium Grade IV Small-Diameter Bone Level Implants in Edentulous Mandibles - Results from a 1-Year Observation Period. Clinical Implant Dentistry and Related Research. 2012;14(6):896–904. doi: 10.1111/j.1708-8208.2010.00324.x. [DOI] [PubMed] [Google Scholar]
- 14.Ramoni RB, Walji MF, White J, et al. From good to better: toward a patient safety initiative in dentistry. J Am Dent Assoc. 2012;143(9):956–960. doi: 10.14219/jada.archive.2012.0303. [DOI] [PubMed] [Google Scholar]
- 15.Ramoni R, Walji MF, Tavares A, et al. Open wide: looking into the safety culture of dental school clinics. J Dent Educ. 2014;78(5):745–756. [PubMed] [Google Scholar]
- 16.Kalenderian E, Walji MF, Tavares A, Ramoni RB. An adverse event trigger tool in dentistry: a new methodology for measuring harm in the dental office. J Am Dent Assoc. 2013;144(7):808–814. doi: 10.14219/jada.archive.2013.0191. [DOI] [PubMed] [Google Scholar]
- 17.Executive Summary. Rockville, MD: Agency for Healthcare Research and Quality; 2015. [Accessed 12/18/2015]. AHRQ Medical Office Survey on Patient Safety Culture. " http://www.ahrq.gov/professionals/quality-patient-safety/patientsafetyculture/medical-office/2014/mosurv14sum.html". [Google Scholar]
- 18.Rockville, MD: Agency for Healthcare Research and Quality; 2012. [Accessed 12/18/2015]. AHRQ Medical Office Survey on Patient Safety Culture. " http://www.ahrq.gov/professionals/quality-patient-safety/patientsafetyculture/medical-office/2012/index.html". [Google Scholar]
- 19.Thusu S, Panesar S, Bedi R. Patient safety in dentistry - state of play as revealed by a national database of errors. Br Dent J. 2012;213(3):E3. doi: 10.1038/sj.bdj.2012.669. [DOI] [PubMed] [Google Scholar]
- 20.Hiivala N, Mussalo-Rauhamaa H, Murtomaa H. Patient safety incidents reported by Finnish dentists; results from an internet-based survey. Acta Odontol Scand. 2013;71(6):1370–1377. doi: 10.3109/00016357.2013.764005. [DOI] [PubMed] [Google Scholar]
- 21.Milgrom P. Quality control of end results: identifying avoidable adverse events in dentistry. J Am Dent Assoc. 1975;90(6):1282–1290. doi: 10.14219/jada.archive.1975.0279. [DOI] [PubMed] [Google Scholar]
- 22.Perea-Perez B, Labajo-Gonzalez E, Santiago-Saez A, Albarran-Juan E, Villa-Vigil A. Analysis of 415 adverse events in dental practice in Spain from 2000 to 2010. Med Oral Patol Oral Cir Bucal. 2014;19(5):e500–e505. doi: 10.4317/medoral.19601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mettes T, Bruers J, van der Sanden W, Wensing M. Patient safety in dental care: A challenging quality issue? An exploratory cohort study. Acta Odontol Scand. 2013;71(6):1588–1593. doi: 10.3109/00016357.2013.777471. [DOI] [PubMed] [Google Scholar]
- 24.Perea-Perez B, Santiago-Saez A, Garcia-Marin F, Labajo-Gonzalez E, Villa-Vigil A. Patient safety in dentistry: dental care risk management plan. Med Oral Patol Oral Cir Bucal. 2011;16(6):e805–e809. doi: 10.4317/medoral.17085. [DOI] [PubMed] [Google Scholar]
- 25.Ashley MP, Pemberton MN, Saksena A, Shaw A, Dickson S. Improving patient safety in a UK dental hospital: long-term use of clinical audit. Br Dent J. 2014;217(7):369–373. doi: 10.1038/sj.bdj.2014.861. [DOI] [PubMed] [Google Scholar]
- 26.Pemberton MN, Ashley MP, Shaw A, Dickson S, Saksena A. Measuring patient safety in a UK dental hospital: development of a dental clinical effectiveness dashboard. Br Dent J. 2014;217(7):375–378. doi: 10.1038/sj.bdj.2014.859. [DOI] [PubMed] [Google Scholar]
- 27.Saksena A, Pemberton MN, Shaw A, Dickson S, Ashley MP. Preventing wrong tooth extraction: experience in development and implementation of an outpatient safety checklist. Br Dent J. 2014;217(7):357–362. doi: 10.1038/sj.bdj.2014.860. [DOI] [PubMed] [Google Scholar]
- 28.Dicicco-Bloom B, Crabtree BF. The qualitative research interview. Med Educ. 2006;40(4):314–321. doi: 10.1111/j.1365-2929.2006.02418.x. [DOI] [PubMed] [Google Scholar]
- 29.Sandelowski M. Whatever happened to qualitative description? Res Nurs Health. 2000;23(4):334–340. doi: 10.1002/1098-240x(200008)23:4<334::aid-nur9>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 30.Neergaard MA, Olesen F, Andersen RS, Sondergaard J. Qualitative description - the poor cousin of health research? BMC Med Res Methodol. 2009;9:52. doi: 10.1186/1471-2288-9-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bartels LM. Democracy with attitudes. In: MacKuen MB, Rabinowitz G, editors. Electoral democracy. Ann Arbor, MI: University of Michigan Press; 2003. pp. 48–82. [Google Scholar]
- 32.Flick U. An Introduction to Qualitative Research. Thousand Oaks, CA: Sage; 2009. [Google Scholar]
- 33.Gill P, Stewart K, Treasure E, Chadwick B. Conducting qualitative interviews with school children in dental research. Br Dent J. 2008;204(7):371–374. doi: 10.1038/sj.bdj.2008.245. [DOI] [PubMed] [Google Scholar]
- 34.Gill P, Stewart K, Treasure E, Chadwick B. Methods of data collection in qualitative research: interviews and focus groups. Br Dent J. 2008;204(6):291–295. doi: 10.1038/bdj.2008.192. [DOI] [PubMed] [Google Scholar]
- 35.Hannes K, Norre D, Goedhuys J, Naert I, Aertgeerts B. Obstacles to implementing evidence-based dentistry: a focus group-based study. J Dent Educ. 2008;72(6):736–744. [PubMed] [Google Scholar]
- 36.Meadows LM, Verdi AJ, Crabtree BF. Keeping up appearances: using qualitative research to enhance knowledge of dental practice. J Dent Educ. 2003;67(9):981–990. [PubMed] [Google Scholar]
- 37.Gadbury-Amyot CC, Smith DB, Overman PR, Bunce L. Faculty Development at One Midwestern Dental School: A Program Evaluation. J Dent Educ. 2015;79(10):1177–1188. [PubMed] [Google Scholar]
- 38.Ryan GW, Nolan JM, Yoder PS. Successive free listing: Using multiple free lists to generate explanatory models. Field Methods. 2000;12(2):83. [Google Scholar]
- 39.Weiss W, Bolton P. Training in qualitative research methods for PVOs and NGOs. [Accessed 12/18/2015];Sessions 4.1– 4.3 The Johns Hopkins University School of Public Health 2000. " http://www.jhsph.edu/research/centers-and-institutes/center-for-refugee-and-disaster-response/publications_tools/publications/_pdf/TQR/tg_introduction.PDF". [Google Scholar]
- 40.Leape LL. Error in medicine. JAMA. 1994;272(23):1851–1857. [PubMed] [Google Scholar]
- 41.Leape LL, Brennan TA, Laird N, et al. The nature of adverse events in hospitalized patients. Results of the Harvard Medical Practice Study II. N Engl J Med. 1991;324(6):377–384. doi: 10.1056/NEJM199102073240605. [DOI] [PubMed] [Google Scholar]
- 42.Leape LL, Lawthers AG, Brennan TA, Johnson WG. Preventing medical injury. QRB Qual Rev Bull. 1993;19(5):144–149. doi: 10.1016/s0097-5990(16)30608-x. [DOI] [PubMed] [Google Scholar]
- 43.Henneman EA, Blank FS, Gattasso S, Williamson K, Henneman PL. Testing a classification model for emergency department errors. J Adv Nurs. 2006;55(1):90–99. doi: 10.1111/j.1365-2648.2006.03878.x. [DOI] [PubMed] [Google Scholar]
- 44.Battles JB, Kaplan HS, Van der Schaaf TW, Shea CE. The attributes of medical event-reporting systems: experience with a prototype medical event-reporting system for transfusion medicine. Archives of pathology & laboratory medicine. 1998;122(3):231–238. [PubMed] [Google Scholar]
- 45.van Vuuren W, Shea CE, van der Schaaf TW. The development of an incident analysis tool for the medical field. Eindhoven, the Netherlands: Technische Universiteit Eindhoven; 1997. [Google Scholar]
- 46.Mers TM. Medical Event Reporting System for Transfusion Medicine reference manual, version 3.0. New York: 2001. [Accessed 06/10/2015]; "How dental team members describe AEs JADA resubmission 04142016.docx". [Google Scholar]
- 47.Katzenbach JR, Smith DK. The wisdom of teams: creating the high-performance organization. Boston, Mass: Harvard Business School Press; 1993. [Google Scholar]
- 48.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. [PubMed] [Google Scholar]
- 49.Tiwana KK, Morton T, Tiwana PS. Aspiration and ingestion in dental practice: a 10-year institutional review. J Am Dent Assoc. 2004;135(9):1287–1291. doi: 10.14219/jada.archive.2004.0404. [DOI] [PubMed] [Google Scholar]
- 50.Fields RT, Jr, Schow SR. Aspiration and ingestion of foreign bodies in oral and maxillofacial surgery: a review of the literature and report of five cases. J Oral Maxillofac Surg. 1998;56(9):1091–1098. doi: 10.1016/s0278-2391(98)90263-4. [DOI] [PubMed] [Google Scholar]
- 51.Seals ML, Andry JM, Kellar PN. Pulmonary aspiration of a metal casting: report of case. J Am Dent Assoc. 1988;117(5):587–588. doi: 10.14219/jada.archive.1988.0050. [DOI] [PubMed] [Google Scholar]
- 52.Maxwell J. Qualitative Research Design: An Interactive Approach. Thousand Oaks, CA: Sage; 2005. [Google Scholar]
- 53.Light RJ, Singer J, Willett J. By design: Conducting research on higher education. Cambridge, MA: Harvard University Press; 1990. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.