Abstract
Objectives
To identify which clinical specialties are most central for care of people with dementia in the community and long term care (LTC) settings.
Design
Cross-sectional analysis
Participants
Fee-for-service Medicare beneficiaries aged ≥65 years with dementia
Measurements
Specialty, categorized into primary care (internal or family medicine, geriatrics, or nurse practitioners (NPs)) versus other specialties, of the predominant provider of care (PPC) for each patient, defined by providing the most ambulatory visits.
Results
Among 2,598,719 beneficiaries with dementia, 74% lived in the community and 80% had a PPC in primary care. In LTC, 91% had primary care as their PPC compared to 77% in community (p<.001). Cardiology and neurology were most frequent specialists. NPs were PPCs for 19% of dementia patients in LTC versus 7% in the community (p<.001).
Conclusion
It is unknown whether specialists are aware of their central role for many dementia patients’ care needs. In LTC, NPs play a lead role as PPCs.
Keywords: predominant provider, dementia, primary care, specialist, long-term care, Medicare
INTRODUCTION
An estimated 72 million older adults in the US will be age 65 and older by 2030, representing 20% of the total population (up from 13% in 2010) [1]. The risk of dementia increases with age; as people live longer, more people will be at risk for dementia. By 2050, an estimated 13.8% of the U.S. population will have dementia such as Alzheimer’s disease, with the largest increase in the age group 85+[1].
Outside of the U.S., IMPACT (Important Perspectives on Alzheimer's Care and Treatment) survey characterized the roles of primary care and specialists who treat Alzheimer’s disease (AD) from five European countries [2]. While IMPACT provides an international perspective, we do not have a similar understanding of which specialties are providing care for dementia patients in the US. In the United States, geriatrics, neurology, and geriatric psychiatry are the physician specialties most associated with providing either primary or consultative care for dementia patients [3]. Nurse practitioners (NPs) are also important providers for people with dementia, with changes in their training that consolidate adult care and gerontology to assure more will be available to the growing elderly population [3]. But the role of these providers has not been described nationally for community-dwelling and long term care (LTC) residents with dementia.
There is concern, however, about potential shortages of providers trained in the care of dementia, including nurse practitioners, geriatricians, geriatric psychiatrists, and neurologists. The Bureau of Labor Statistics for the U.S. predicts a 34% increase in demand for NPs from 2012 to 2022 [3] and a need for 36,000 geriatricians by 2030, which is a 5-fold increase from current 7,147 certified geriatricians in the US [3]. There are even fewer geriatric psychiatrists, 1,554 in the US in 2012 [3], and the demand for neurologists already exceed the supply of 14,338 in practice in 2012 [3]. Due to projected short falls of providers relative to the large population with dementia, we need a better understanding of who provides a substantive amount of care to dementia patients in the US to target educational or other resources that will assure access to high quality dementia care in the future.
In this study, we identify the predominant provider of care (PPC) as the provider with the greatest proportion of ambulatory visits for each Medicare beneficiary with a dementia diagnosis. The goals of the study are three fold: to determine 1) which specialties are currently the PPC for older adults with dementia, 2) how LTC and community differ in the specialties of PPCs, and 3) how NPs as the PPC differ based on geography of the United States.
METHODS
Design
This study is a cross-sectional analysis of 100% of national fee-for-service Medicare beneficiaries (2012) with a dementia diagnosis. The 2012 Medicare Beneficiary Summery file was used to identify beneficiaries who resided in the 50 States and DC, were age 65 and older on January 1, not enrolled in HMO, and had both Parts A and B coverage during the entire year or until death. We then searched their 2012 inpatient and outpatient claims to determine if they had a dementia diagnosis based on the ICD-9 codes used in RX Hierarchical Condition Categories 54 and 55 (see appendix A). The Minimum Data Set was used to identify LTC residents by having at least 100 days in a nursing home.
Measures
The main variable of interest is the specialty of the predominant provider of ambulatory care (PPC) who provided the greatest proportion of outpatient visits. Providers were assigned the CMS specialty code under which they billed most. We categorized family practice, internal medicine, general practice, geriatric medicine, and NP as primary care providers and all others as specialists. Patient characteristics included age, sex, race, and severity of illness measured as the number of short-stay acute care hospitalizations, Charlson comorbidity index [4], and mortality. Age, sex, race, and data of death were obtained from the Medicare Beneficiary Summary File. Medicare Provider Analysis and Review (MEDPAR) and Carrier (Physician/Supplier Part B claims) files were used to obtain diagnoses for the Charlson index, hospitalizations, visit counts, and the number of unique providers seen using the providers’ unique NPI numbers.
Statistical analysis
We examined patient characteristics by specialty of the PPC and by community vs LTC settings using t-test or Chi-squared tests, as appropriate. We present maps to show geographic variation at the state level for NPs as the PPC of care. This study was approved by the Dartmouth College Institutional Review Board.
RESULTS
Cohort description
There were more than 2.5 million Medicare beneficiaries with a dementia diagnosis in 2012. Three quarters of the cohort lived in the community and most were women and Caucasian. Mean age for these beneficiaries with dementia was 82.4 (SD 7.8). On average, each beneficiary with dementia had one hospitalization, 13.1 ambulatory visits and saw on average 4 unique providers per year. 77% of LTC beneficiaries are dually eligible for Medicare and Medicaid, compared to only 21% in the community. LTC beneficiaries are sicker, with higher mean Charlson count (2.8 vs 2.2) and higher annual mortality for all causes (25.6% vs 15.4%) than those in the community. The average number of visits per beneficiary to the assigned PPC was 9.8 (57% of total visits) for LTC residents and 5.6 (48% of total visits) in the community (p<0.001). There were fewer visits to any specialists in LTC than in community (mean 3.1 vs4.6, p<.0001).
Specialties serving as PPC
Overall, 80% of beneficiaries had a primary care provider as their PPC. Over 90% of beneficiaries had primary care providers as their PPC in LTC compared to 77.3% of beneficiaries in community (p<0.001). Among primary care providers, internists were the most frequent PPC at 36.3%, followed by family practitioners (29.8%), and NPs (10.1%) (p<0.001). Among the primary care providers, NP’s as PPCs had the greatest difference between community (6.9%) and LTC (19.2%) (p<0.001).
Table 2 lists the most common 15 specialties as PPC for beneficiaries with dementia. The specialists were not specific to treatment of dementia, simply those who were seeing beneficiaries with dementia the most. The top specialists collectively were the PPCs for 8.4% of beneficiaries overall: cardiology, neurology, hematology/oncology, and urology. All four specialties were more likely to be the PPC in the community compared to in LTC (11.1% vs1.3%). Although it was not among the top four specialties, psychiatry served as the PPC in greater proportion in LTC compared to community (2.0% vs. 0.6%, p <0.001).
Table 2.
Most Common Specialties of Predominant Providers of Care for Fee-for-service Older Medicare Beneficiaries with a Dementia Diagnosis (2012)
| Provider Type | Overall N | LTC | Community |
|---|---|---|---|
| N beneficiaries (%) | 2,598,719 (100) | 677,048 (100) | 1,921,671 (100) |
| Primary Care as Predominant Providers (%) | 2,100,308 (80.8) | 615,788 (91.0) | 1,484,520 (77.3) |
| 1 Internal Medicine (%) | 942,384 (36.3) | 230,918 (34.1) | 711,466 (37.0) |
| 2 Family Practice (%) | 774,534 (29.8) | 213,768 (31.6) | 560,766 (29.2) |
| 3 Nurse Practitioner (%) | 262,625 (10.1) | 129,622 (19.2) | 133,003 (6.9) |
| 4 Geriatric Medicine (%) | 67,923 (2.6) | 24,636 (3.6) | 43,287 (2.3) |
| 5 General Practice (%) | 52,842 (2.0) | 16,844 (2.5) | 35,998 (1.9) |
| Specialist as Predominant Providers (%) | 498,411 (19.2) | 61,260 (9.1) | 437,151 (22.8) |
| 1 Cardiology (%) | 88,302 (3.4) | 3,303 (0.5) | 84,999 (4.4) |
| 2 Neurology (%) | 73,799 (2.8) | 1,744 (0.3) | 72,055 (3.8) |
| 3 Hematology/Oncology (%) | 31,580 (1.2) | 1,697 (0.3) | 29,883 (1.6) |
| 4 Urology (%) | 27,025 (1.0) | 1,396 (0.2) | 25,629 (1.3) |
| 5 Psychiatry (%) | 26,071 (1.0) | 13,737 (2.0) | 12,334 (0.6) |
| 6 Physical Medicine/Rehab (%) | 24,455 (0.9) | 6,792 (1.0) | 17,663 (0.9) |
| 7 Emergency Medicine (%) | 23,127 (0.9) | 7,137 (1.1) | 15,990 (0.8) |
| 8 Dermatology (%) | 21,486 (0.8) | 1,038 (0.2) | 20,448 (1.1) |
| 9 Pulmonary Disease (%) | 19,531 (0.8) | 2,591 (0.4) | 16,940 (0.9) |
| 10 Orthopedic Surgery (%) | 19,015 (0.7) | 1,257 (0.2) | 17,758 (0.9) |
| 11 General Surgery (%) | 16,719 (0.6) | 5,304 (0.8) | 11,415 (0.6) |
| 12 Ophthalmology (%) | 15,646 (0.6) | 926 (0.1) | 14,720 (0.8) |
| 13 Nephrology (%) | 15,586 (0.6) | 1,682 (0.3) | 13,904 (0.7) |
| 14 Endocrinology (%) | 10,498 (0.4) | 514 (0.1) | 9,984 (0.5) |
| 15 Otolaryngology (%) | 10,165 (0.4) | 722 (0.1) | 9,443 (0.5) |
All comparisons among columns have p values <0.001.
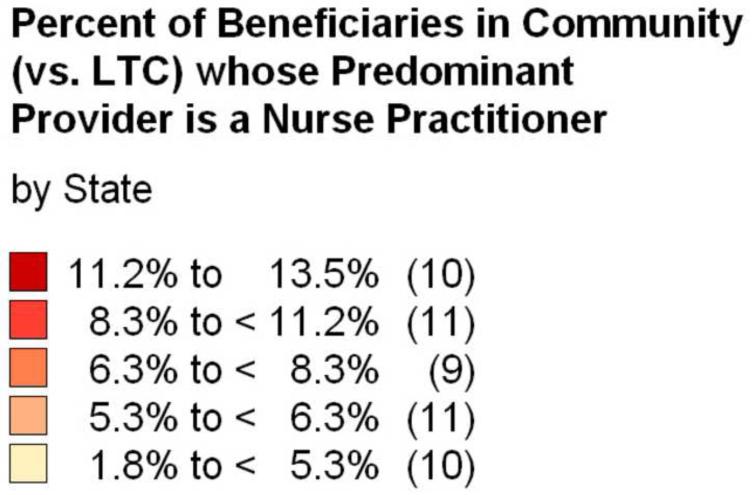
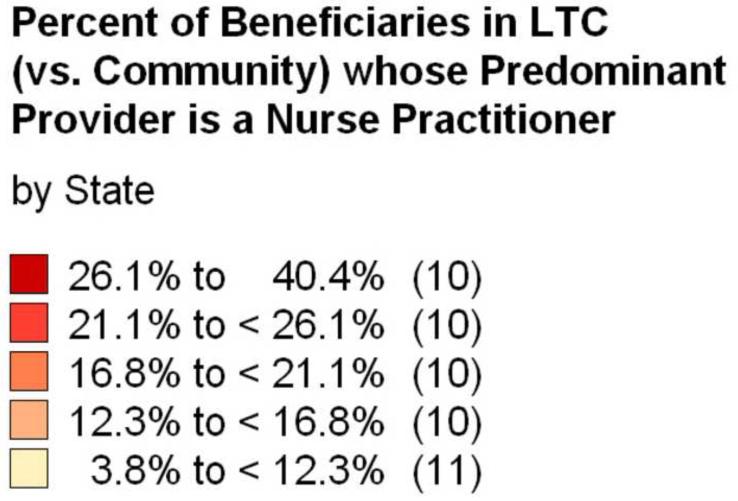
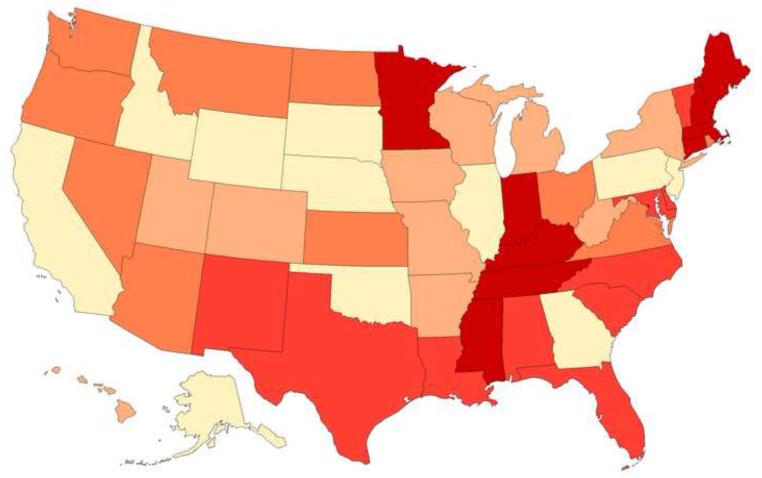
Nurse practitioners in long-term care and in community
Due to known differences in state regulation of NP practice, we examined geographic difference in use of NPs as the PPC. Map 1 and Map 2 show the percent of dementia beneficiaries with whose PPC was a NP in LTC and the community by quintiles of proportion of NPs as PPC, respectively. In LTC, the range across states was 3.8% to 40.4% while in community the range across states was 1.8% to 13.5%. The highest quintile states for those in the community were mostly the same states as those in the highest quintile in long-term care except Alaska (AK) and North Dakota (ND). There are more differences between community and LTC settings in the low quintile states. Only 5 (CA, OK, IL, PA, and GA) of 10 states in the lowest quintile in the community were also in the lowest LTC quintile.
Map 1.
Community
Map 2.
LTC
DISCUSSION
Our data show that the majority of PPCs for beneficiaries with dementia diagnoses were primary care clinicians. The critical role primary care clinician play in the management of people with dementia will only grow as the number of beneficiaries with dementia increases with population aging. Among the specialties we have categorized as primary care, geriatrics is the only one that has substantial training in the diagnosis and treatment of dementia [3]. Studies of primary care providers in the US have shown that a substantial number of primary care providers prefer to refer dementia patients to specialists because of uncertainty in making diagnosis of dementia[5] and managing behavioral and psychological symptoms[6], and to recommend driving evaluation [6]. The potential groups to refer dementia beneficiaries to: geriatric psychiatry, neurology or geriatrics, are all small specialties and may not be easily accessible for the volume of patients [3]. These studies demonstrate that additional educational efforts are need to be directed toward primary care providers who are often the PPCs of individuals with dementia.
Another important insight from this study is that overall 20% of beneficiaries with dementia see specialists for most of their care. From these data alone, we cannot determine if the prominence of these specialists is related to an acute issue which could lead to these specialists being most frequently seen as opposed to providing longitudinal management over long periods of time. The critical issue in either scenario is whether the provider, who might have little training in dementia, recognize the dementia and incorporate it in determining capacity to consent, goals of care, and ability for self-management. Many of these providers may be working in tandem with a primary care provider to meet the broad needs of these patients. Both specialists and primary care providers report difficulty accessing community resources and both want to have bi-directional communication between specialists and primary care [6], which may be areas for collaborative efforts at improvement.
Beneficiaries with dementia in LTC were infrequently managed by specialists. In fact, neurologists were 14 times more likely to serve as PPCs for dementia beneficiaries in the community than in LTC. The lower likelihood of specialties as PPCs in LTC facilities is likely due to delivery of primary care on site in most nursing homes. Further study would be needed to know whether specialists continue to follow people, although not as PPC, as they transition into long term care.
A final insight from this study is the important role that NPs play as PPCs in LTC and how that role differs across states. In LTC, 40 states had NPs serving as PPCs for 12% to 40% of dementia beneficiaries living in long-term care facilities. In the community setting, the inverse was true -- 41 states had NPs serving as PPC for 11% or less of dementia beneficiaries living in the community. Highest use of NPs was in the South Central and New England regions.
It is possible that different state restrictions on NP’s scope of practice may influence the percentage of NP serving as PPC for beneficiaries with dementia. There are three levels of NP practice: full, reduced, and restricted [7]. States with restricted NP practice requires supervision, delegation, or team-management by an “outside health discipline”, usually a physician, in order for the NP to provide patient care (such as CA, OK, and GA with the lowest percentage of NP serving as PPC), while full practice states do not require an “outside health discipline” in order for NP to provide patient care (such as MN, ME, NH, and CT with the highest percentage of NP serving as PPC) [7]. However, TN has restricted practice for NP, but is in the group of states with the highest percentage of NP serving as PPC [7]. KY and MS both have reduced practice for NP [7], but both states were in the highest group of NP serving as PPC. Thus, states’ policies on NP’s scope of practice do not fully explain whether NPs are more likely to serve as PPCs.
Another possible explanation for differences in where NPs serve as PPCs is that those states with the most shortage of primary care providers may have more NPs serving as PPCs. Federal regulation stipulates that for an area to be considered primary care health professional shortage area (HPSA), the area must have a population-to-physician ratio of at least 3,500 to 1[8]. HPSA does not take into account primary care provided by nurse practitioners or physician assistants [8]. The states in the highest quintile and the lowest quintile of NPs as PPCs all have about the same shortage of primary care health professionals [8]. Thus, the degree of primary care shortage in each state does not seem to entirely explain the proportion of NPs serving as PPCs. The factors that either facilitate or act as barriers to greater NP participation in care of people with dementia in the context of the growing population warrants further attention.
The limitations of our study rest mainly in the constraints of administrative data. First the diagnosis of dementia is determined by whether a clinician bills for the diagnosis using ICD-9 codes. Claims have good specificity for dementia but lack sensitivity, under-ascertaining early disease [9, 10]. The provider with the most visits for each beneficiary was identified as the PPC in our study, but may not be the one in most frequent contact if there is high inter-visit care and communication not captured by billing data. There may also be some misclassification of clinicians as primary care versus specialist. For the physicians, we defined specialty as the one they most often billed under, which may differ from their self-designated specialty. For NPs, administrative data do not distinguish those NPs who practice in a specialty setting versus primary care and we opted to categorize them as primary care. According to AANP National Nurse Practitioner Practice Site Census, 86.5% of NPs have primary care focus [11]. Thus, grouping NPs into primary care seems most appropriate. Finally, we were also limited in our ability to study patient factors, such as their educational level and socioeconomic status, which may influence whether a person seeks primary care or specialty providers.
Conclusion
With the growing number of adults with dementia in the US and the potentially limited number of health care providers, our study identified the key specialties on which to focus for dementia education and for practice improvement and innovation. Among primary care providers, internists, family medicine, and nurse practitioners (especially in the LTC setting) were the PPCs. Among specialists, cardiologists, neurologists, hematologist/oncologists, and urologists were most often PPCs. Future research should investigate whether having primary care or specialists as the PPC translates to different health outcomes for beneficiaries with dementia.
Table 1.
Patient Characteristics and Patters of Service Use for Fee-for-service Older Medicare Beneficiaries with a Dementia Diagnosis (2012)
| Total | Long-term care | Community | |
|---|---|---|---|
| Number of beneficiaries, n (%) | 2,598,719 (100) | 677,048 (26) | 1,921,671 (74) |
| Female (%) | 1,701,995 (65.5) | 489,515 (72.3) | 1,212,480 (63.1) |
| Age in years, mean (SD) | 82.4 (7.8) | 84.24 (8.0) | 81.71 (7.7) |
| 65-75, n (%) | 534,280 (20.6) | 104,061 (15.4) | 430,219 (22.4) |
| 76-84, n (%) | 959,722 (36.9) | 214,741 (31.7) | 744,981 (38.8) |
| ≥85, n (%) | 1,104,717 (42.5) | 358,246 (52.9) | 746,471 (38.8) |
| Race | |||
| White, n (%) | 2,144,316 (82.5) | 550,486 (81.3) | 1,593,830 (82.9) |
| Black, n (%) | 246,130 (9.5) | 79,357 (11.7) | 166,773 (8.7) |
| Hispanic, n (%) | 133,800 (5.2) | 32,017 (4.7) | 101,783 (5.3) |
| Other, n (%) | 74,473 (2.9) | 15,188 (2.2) | 59,285 (3.1) |
| Dual Eligible * , n (%) | 924,035 (35.6) | 524,089 (77.4) | 399,946 (20.8) |
| Charlson count †, mean (SD) | 2.38 (1.9) | 2.8 (1.9) | 2.24 (1.9) |
| Annual mortality, n (%) | 469,516 (18.1) | 173,348 (25.6) | 296,168 (15.4) |
| Hospitalizations, mean per person (SD) | 0.9 (1.3) | 0.89 (1.4) | 0.91 (1.3) |
| Unique Providers of Visits, mean per person (SD) | 4.08 (2.8) | 3.67 (2.5) | 4.23 (2.9) |
| Ambulatory Visits | |||
| To any provider, mean (SD) | 13.1 (11.0) | 17.06 (14) | 11.71 (9.3) |
| To predominant provider, mean (SD) | 6.7 (6.0) | 9.8 (8.2) | 5.6 (4.5) |
| To any primary care provider, mean (SD) | 8.39 (8.2) | 13.17(11.2) | 6.7 (6.0) |
| To any specialist, mean (SD) | 4.18 (5.8) | 3.1 (5.7) | 4.56 (5.8) |
Dual eligible = eligible for both Medicare & Medicaid,
Charlson count = Charlson Comorbidity Index score. All comparisons among columns have p values <0.001.
ACKNOWLEDGEMENTS
This study was funded by a grant from the John A. Hartford Foundation and NIA P01 AG19783. Dr. Yang was supported by Geriatric Training Grant by Donald W. Reynolds Foundation. Dr. Oh was supported by 1K23AG043504-01 (NIA/NIH), P50 AG005146, and the Roberts Gift Fund. We would also like to thank Kristen K. Bronner for her assistance with creating maps.
Appendix. A. Definition of dementia
RxHCC54: ICD-9 diagnosis code 331.0
RxHCC55: ICD-9 diagnosis codes 046.0, 046.11, 046.19, 046.2, 046.3, 046.71, 046.72, 046.79, 046.8, 046.9, 290.0, 290.10, 290.11, 290.12, 290.13, 290.20, 290.21, 290.3, 290.40, 290.41, 290.42, 290.43, 290.8, 290.9, 294.0, 294.10, 294.11, 294.20, 294.21, 294.8, 294.9, 330.0, 330.1, 330.2, 330.3, 330.8, 330.9, 331.11, 331.19, 331.2, 331.6, 331.7, 331.81, 331.82, 331.89, 331.9
References
- [1]. [Accessed October 26, 2015]; http://www.alz.org/facts/downloads/facts_figures_2015.pdf.
- [2].Robinson L, Vellas B, Knox S, et al. Clinical Practice Patterns of Generalists and Specialists in Alzheimer’s Disease: What Are the Differences, and What Difference Do They Make? The Journal of Nutrition, Health & Aging. 2010;14:545–552. doi: 10.1007/s12603-010-0266-8. [DOI] [PubMed] [Google Scholar]
- [3].Warshaw GA, Bragg EJ. Preparing the Health Care Workforce To Care For Adults With Alzheimer’s Disease And Related Dementias. Health Affairs. 2014;33:633–641. doi: 10.1377/hlthaff.2013.1232. [DOI] [PubMed] [Google Scholar]
- [4].Charlson M, Szatrowski TP, Peterson J, et al. Validation of a Combined Comorbidity Index. J Clin Epidemiol. 1994;11:1245–1251. doi: 10.1016/0895-4356(94)90129-5. [DOI] [PubMed] [Google Scholar]
- [5].Pimlott NJ, Persaud M, Drummond N, et al. Family physicians and dementia in Canada. Part2. Understanding the challenges of dementia care. Can Fam Physician. 2009;55:508–509. [PMC free article] [PubMed] [Google Scholar]
- [6].Hum S, Cohen C, Persaud M, et al. Role Expectations in Dementia Care Among Family Physicians and Specialists. Canadian Geriatrics Journal. 2014;17:95–102. doi: 10.5770/cgj.17.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7]. [Accessed October 26, 2015]; http://www.aanp.org/images/documents/state-leg-reg/stateregulatorymap.pdf.
- [8]. [Accessed October 27, 2015]; http://kff.org/other/state-indicator/primary-care-health-professional-shortage-areas-hpsas/#map.
- [9].Newcomer R, Clay T, Luxenberg JS, et al. Misclassification and selection bias when identifying Alzheimer’s disease solely from Medicare claims records. J Am Geriatr Soc. 1999;47(2):215–9. doi: 10.1111/j.1532-5415.1999.tb04580.x. [DOI] [PubMed] [Google Scholar]
- [10].Taylor DH, Fillenbaum GG, Ezell ME. The accuracy of medicare claims data in identifying Alzheimer’s disease. J Clin Epidemiol. 2002;55(9):929–37. doi: 10.1016/s0895-4356(02)00452-3. [DOI] [PubMed] [Google Scholar]
- [11]. [Accessed October 26, 2015]; http://www.aanp.org/all-about-nps/np-fact-sheet.