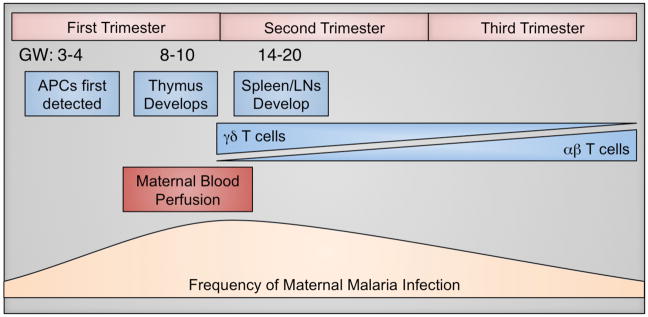
Figure 1. Gestational Timeline of Fetal Immune Development and Maternal Factors Influencing Placental Malaria.
Fetal immune development (blue) begins as early as gestational week (GW) 3–4, with the emergence of antigen-presenting cells (APCs). Thymic development occurs between GW 8–10, followed by the appearance of secondary lymphoid structures, such as the spleen and lymph nodes (LNs). Naïve T cells can first be detected in the periphery around GW 12 and initially the T cell pool is predominated by γδ T cells. The proportion of γδ T cells declines with gestational age, concurrent with expansion of the αβ T cell population, which constitutes the majority at birth. The placenta is also growing rapidly during early gestation. A key turning point in placental growth is the perfusion of the placenta with maternal blood, which occurs between GW 6–12, and theoretically represents the first opportunity for malaria parasites to access the placenta for sequestration (maroon). Pregnant women are more susceptible than non-pregnant adults to malaria infection; however, the highest rates of infection and highest parasite densities seem to occur between 9–20 weeks (tan) in primigravidas. Collectively, these overlapping factors suggest that the first window of vulnerability for placental malaria infection and fetal immune exposure may occur late in the first trimester or early in the second trimester (~GW 10–16).