Figure 1.
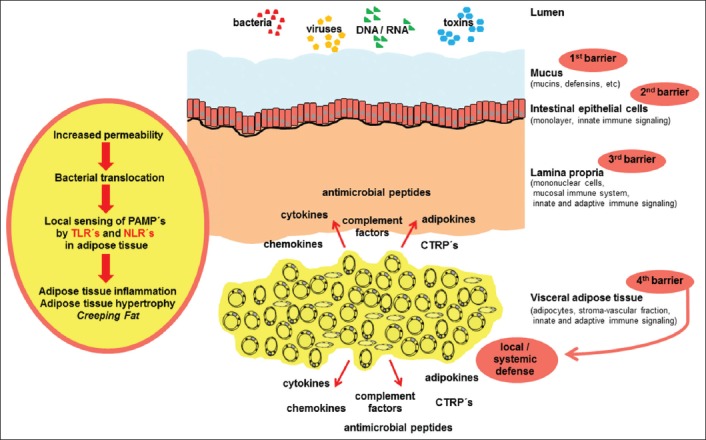
Current hypothetical view of the role of visceral adipose tissue in inflammatory bowel disease
The intestinal mucus provides a first barrier against luminal toxins and invading pathogens. In the context of intestinal inflammation and increased permeability of the mucus and epithelium, microbes and toxins are able to cross the epithelial and mucus barriers. Subsequently, lamina propria mononuclear cells interact with these compounds. When invasion cannot be contained by the mucosal compartment, pathogen associated molecular patterns (PAMPs) are recognized by Toll-like receptors (TLRs) and nucleotide-binding oligomerization domain-like receptors (NLRs) in adipose tissue. Activation of TLRs and NLRs causes adipose tissue inflammation, hypertrophy and the formation of creeping fat. This altered adipose tissue releases cytokines, adipokines, chemokines, complement factors, antimicrobial peptides and C1q/tumor necrosis factor-related proteins (CTRPs), thus providing a “fourth barrier” of local defense. This mechanism might protect against local gut perforation, local peritonitis, systemic inflammation, and sepsis
