Abstract
Purpose
This study examined the risk factors of a delayed diagnosis of acute appendicitis in children undergoing an appendectomy.
Methods
This retrospective study involved children aged below 18 years, who underwent an appendectomy. After dividing them into a delayed diagnosis group and nondelayed diagnosis group according to the time interval between the initial hospital visit and final diagnosis, the risk factors of delayed diagnosis were identified using logistic regression analysis.
Results
Among 712 patients, 105 patients (14.7%) were classified in the delayed diagnosis group; 92 patients (12.9%) were diagnosed using ultrasonography (US), and both US and computed tomography were performed in 38 patients (5.3%). More patients in the delayed diagnosis group underwent US (P=0.03). Spring season and prior local clinic visit were significantly associated with a delayed diagnosis. Fever and diarrhea were more common in the delayed diagnosis group (fever: odds ratio [OR], 1.37; 95% confidence interval [CI], 1.05–1.81; diarrhea: OR, 1.94; 95% CI, 1.08–3.46; P<0.05). These patients showed symptoms for a longer duration (OR, 2.59; 95% CI, 1.78–3.78; P<0.05), and the admission course (OR, 1.26; 95% CI, 1.11–1.44; P<0.05) and C-reactive protein (CRP) levels (OR, 1.47; 95% CI, 1.19–1.82; P<0.05) were associated with the delayed diagnosis.
Conclusion
To decrease the rate of delayed diagnoses of acute appendicitis, symptoms such as fever and diarrhea, seasonal variations, admission course, and CRP levels should be considered and children with a longer duration of symptoms should be closely monitored.
Keywords: Appendicitis, Delayed diagnosis, Child, Risk factors
Introduction
Appendicitis is often difficult to diagnosis because of the absence of a pathognomonic signs or symptoms, the poor predictive value of associated laboratory testing, and its varied presentation1). Moreover, diagnosis is more complicated, especially in children for several reasons. The first is the inability to accurately communicate the typical historical features in children, who are less cooperative with physical examination. To increase the diagnostic accuracy, various scoring systems with modern imaging modalities have been applied2). On the other hand, distinguishing between the diagnosis of appendicitis and other common pediatric diseases with overlapping symptoms remains a challenge3). Despite the availability of multiple new diagnostic modalities, the initial misdiagnosis rates range from 28% to 57% for children 12 years old or younger to nearly 100% in those 2 years old or younger4),5). Previous studies have shown that between 5.9% and 27.6% of patients with acute appendicitis had missed the opportunities to make the diagnosis earlier, resulting in an increase in the rate of perforation to 33.3% to 50.0% from a baseline of 20.3% to 28.0%6),7).
A delayed diagnosis of appendicitis can lead to complications and longer hospitalization. Difficulties of history taking and physical examination particularly in infants and younger children often cause 'diagnostic delay' before appendicitis is eventually diagnosed8),9). Diagnostic delay can result in the rupture, abscess formation, wound complication, and a prolonged hospital stay. An early diagnosis of appendicitis in children is important to prevent perforation, abscess formation, and postoperative complications, and decrease the cost by shortening hospital days3).
In previous studies several factors were reported to cause a diagnostic delay in appendicitis. Patients with no insurance present for care later than children who have health insurance10). Intermittent abdominal complaints, parental delay and failure to contact a physician have also been reported to cause diagnostic delays and the influence of diarrhea was also reported11),12),13).
In South Korea, all citizens are covered by the national health insurance system, so the burden of medical expenses on patients is relatively low. Physicians have more freedom in deciding to perform imaging modalities for patients with suspected appendicitis. This can make a difference in the factors associated with a delayed diagnosis of appendicitis.
This study examined the risk factors of a delayed diagnosis, to suggest a newer scoring system for the early detection of acute appendicitis in children.
Materials and methods
A retrospective case review was conducted on children under 18 years of age who underwent an appendectomy in the Gachon University Gil Medical Center from September 2008 to November 2013.
The demographics, preoperative data, and postoperative information were obtained from the electronic medical records. The data collected included the patient's characteristics, symptoms at presentation (e.g., abdominal pain, migrating pain, nausea, vomiting, diarrhea, fever, and anorexia), temperature, history of any recent prior medical visit, admission course, duration of symptoms, physical examinations (tenderness, rebound tenderness), laboratory examinations (e.g., white blood cell, polymorphonuclear leukocyte [PMNL], C-reactive protein [CRP], bilirubin, aspartate aminotransferase/alanine aminotransferase), and radiological findings. In addition, the variables included the type of operation, pathologic finding, hospital day, and the presence of complications. Each patient's body mass index (BMI) and pediatric appendicitis score (PAS) were calculated. The PAS is an efficient diagnostic tool of appendicitis using the symptoms, signs, and laboratory tests results. Samuel14) reported PAS score of ≥6 shows a high probability of appendicitis.
The patients were classified into 2 groups, according the time interval from the initial visit to the hospital to the final diagnosis before the appendectomy: 24 hours or more (delayed group) and less than 24 hours (nondelayed group).
A total of 756 children were underwent appendectomies during the study period. In cases of a symptom started several days, the duration of symptom checked as 3 days. When the data about patient's symptom were not recorded on doctor's chart, we collected data from nursing chart or NEDIS (National Emergency Department information System). Forty-four cases were excluded because of the incidental appendectomy and other appendectomy cases that were not confirmed to be acute appendicitis, such as chronic inflammation, mild lymphoid hyperplasia, and eosinophilia in the proper muscle pathologically. This study was approved by the Institutional Review Board (approval number: 10-001892). Statistical analysis was performed using IBM SPSS Statistics ver. 20.0 (IBM Co., Armonk, NY, USA). A Student t test, Pearson chi-square, linear by linear association analysis was done. The logistic regression was used and P<0.05 was considered significant.
Results
1. Characteristics
Of a total 712 cases, 105 (14.7%) were in the delayed group and 607 (85.3%) were in the nondelayed group.
Table 1 lists the demographics of the 2 groups. Children between 13–18 years and males were most common in both groups. On the other hand, there was no difference in sex (P=0.134), age distribution (P=0.463), and BMI (P=0.419) between the 2 groups.
Table 1. Demographic characteristics of patients with acute appendicitis.
| Characteristic | Total (n=712) | Delayed group (n=105) | Nondelayed group (n=607) | P value |
|---|---|---|---|---|
| Age (yr) | 0.463 | |||
| 0–2 | 6 (0.8) | 2 (1.9) | 4 (0.6) | |
| 3–6 | 52 (7.3) | 9 (8.6) | 43 (7.1) | |
| 7–12 | 308 (43.3) | 44 (41.9) | 264 (43.5) | |
| 13–18 | 346 (48.6) | 50 (47.6) | 296 (48.8) | |
| Male sex | 440 (62) | 58 (55) | 382 (63) | 0.134 |
| Body mass index (kg/m2) | 19.89±0.44 | 19.05±0.35 | 20.03±0.51 | 0.419 |
Values are presented as number (%) or mean±standard deviation.
2. Seasons and admission course
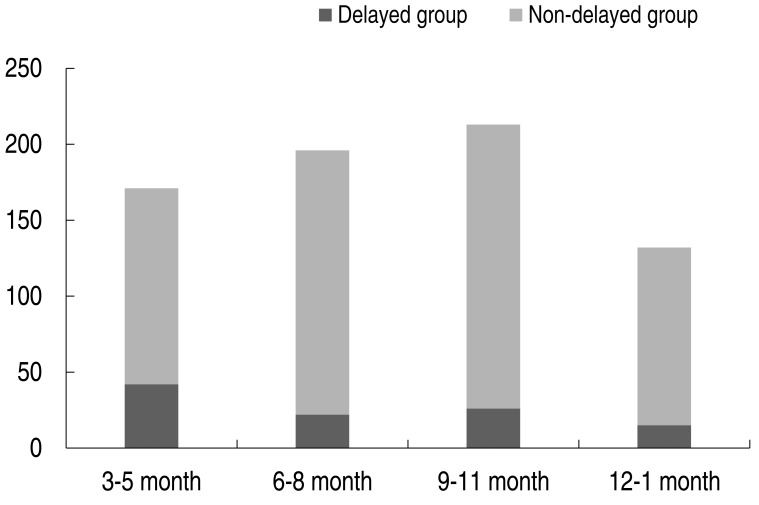
In Table 2, overall children diagnosed with appendicitis visited the most from September to November, in South Korea, which is the fall season. Fig. 1 shows the patients distribution according to season. On the other hand, children in the delayed diagnosed group visited most from March to May, which is the spring season. Overall, 154 children had a prior visit history of local clinics and there were more children in the delayed group. According to the admission course (patient route from admission to the Department of General Surgery), most of the children (81.6%) admitted to the Department of General Surgery were first seen by an Emergency Department (ED) physician. Of all cased, 87 children (12.2 %) were admitted through outpatient Department of General Surgery, 44 children (6.2%) were first seen by a pediatrician in the outpatient department and were next referred to a surgeon. The season (P=0.002), prior local clinic visit history (P<0.001), and admission course (P<0.001) showed significant difference between the 2 groups.
Table 2. Medical history of patients with acute appendicitis.
| Characteristic | Total (n=712) | Delayed group (n=105) | Nondelayed group (n=607) | P value |
|---|---|---|---|---|
| Season (mo) | 0.002 | |||
| Mar-May | 171 (24.0) | 42 (40.0) | 129 (21.3) | |
| June-Aug | 196 (27.5) | 22 (20.9) | 174 (28.7) | |
| Sept-Nov | 213 (29.9) | 26 (24.8) | 187 (30.8) | |
| Dec-Feb | 132 (18.5) | 15 (14.3) | 117 (19.3) | |
| Prior local clinic visit | 154 (21.6) | 44 (41.9) | 110 (18.1) | <0.001 |
| Admission course; | ||||
| Admitted to GS | <0.001 | |||
| From ED | 581 (81.6) | 70 (66.7) | 511 (84.2) | |
| From PD OPD | 44 (6.2) | 16 (15.2) | 28 (4.6) | |
| From GS OPD | 87 (12.2) | 19 (18.1) | 68 (11.2) |
Values are presented as number (%).
GS, general surgery; ED, Emergency Department; PD, pediatrics; OPD, outpatient department.
Fig. 1. Distributions of patients with acute appendicitis, according to the number of months required from first hospital visit to final diagnosis.
3. Symptoms and signs and diagnostic methods
Table 3 lists the common sign and symptoms at presentation for the delayed group and nondelayed group. right lower quadrant (RLQ) tenderness, vomiting, and nausea were frequent symptoms of appendicitis children in both group. Diarrhea at presentation was observed more frequently in the delayed group. Among the signs and symptoms, diarrhea (P=0.012) and rebound tenderness (P=0.032) showed significant differences. Most of the appendicitis children have a 1–3 days symptom duration. The duration of symptoms was significantly longer in the delayed diagnosed group (P<0.001). Either an abdominal computed tomography (CT) scan and/or abdominal ultrasonography (US) imaging was performed in each case. Of 712 patients, 582 (81.7%) were diagnosed with appendicitis by CT, whereas 92 patients (12.9%) were diagnosed by US. In 38 patients (5.3%), a CT scan was performed after US because it was inconclusive. US was performed more in the delayed group (P=0.03).
Table 3. Symptoms and signs of patients with acute appendicitis.
| Characteristic | Total (n=712) | Delayed group (n=105) | Nondelayed group (n=607) | P value |
|---|---|---|---|---|
| Symptom duration (day) | <0.001 | |||
| 1–3 | 642 (90.2) | 75 (71.4) | 567 (93.4) | |
| 4–7 | 53 (7.4) | 24 (22.9) | 29 (4.8) | |
| 8–14 | 12 (1.7) | 5 (4.8) | 7 (1.2) | |
| ≥15 | 5 (0.7) | 1 (0.9) | 4 (0.6) | |
| Migrating pain | 76 (10.7) | 12 (11.4) | 64 (10.5) | 0.090 |
| Fever | 107 (15.0) | 22 (21.0) | 85 (14.0) | 0.071 |
| Nausea | 185 (26.0) | 30 (28.6) | 155 (25.5) | 0.745 |
| Vomiting | 205 (28.8) | 33 (31.4) | 172 (28.3) | 0.277 |
| Diarrhea | 76 (10.7) | 19 (18.1) | 57 (9.4) | 0.012 |
| Anorexia | 40 (5.6) | 8 (7.6) | 32 (5.3) | 0.187 |
| RLQ tenderness | 634 (89.0) | 87 (82.9) | 547 (90.1) | 0.086 |
| RLQ rebound tenderness | 457 (64.1) | 56 (53.3) | 401 (66.1) | 0.032 |
Values are presented as number (%).
RLQ, right lower quadrant.
4. Laboratory values
Table 4 lists the laboratory test results between the 2 groups. The delayed group had a higher mean value in CRP, but there was no significant difference between the 2 groups. In addition, the other laboratory results were insignificant. Table 5 compares the PAS, hospital day, and complications of the 2 groups. The hospital stay was 6.6±0.4 days in the delayed group and 5.0±0.1 days in the nondelayed group. The delayed group's hospital day was significantly longer (P=0.001) than the nondelayed group. The PAS and complication cases showed no differences between the 2 groups.
Table 4. Laboratory data of patients with acute appendicitis.
| Characteristic | Delayed group (n=105) | Nondelayed group (n=607) | P value |
|---|---|---|---|
| WBC (mm3) | 13,780±609 | 14,149±199 | 0.566 |
| PMNL (%) | 73.9±1.6 | 76.4±0.5 | 0.150 |
| CRP (mg/dL) | 6.61±0.73 | 5.93±1.84 | 0.874 |
| Bilirubin (mg/dL) | 0.89±0.05 | 0.88±0.03 | 0.853 |
| AST (U/L) | 22.8±0.8 | 22.2±0.4 | 0.547 |
| ALT (U/L) | 14.1±0.7 | 15.5±0.4 | 0.184 |
Values are presented as mean±standard deviation.
WBC, white blood cell; PMNL, polymorphonuclear leukocyte; CRP, C-reactive protein; AST, aspartate aminotransferase; ALT, alanine aminotransferase.
Table 5. Comparison of the PAS, hospital stay, and complications.
| Characteristic | Delayed group (n=105) | Nondelayed group (n=607) | P value |
|---|---|---|---|
| PAS | 4.8 | 5.2 | 0.054 |
| Hospital day (day) | 6.6±0.4 | 5.0±0.1 | 0.001 |
| Complication | 9 (8.6) | 39 (6.4) | 0.418 |
Values are presented as mean±standard deviation or number (%).
PAS, pediatric appendicitis score.
5. Risk factors associated with delayed diagnosis of acute appendicitis
Table 6 lists the results of logistic regression analysis. When analyzed by winter, the spring season was a predictor of a delayed diagnosis of appendicitis (odds ratio [OR], 2.540; 95% confidence interval [CI], 1.338–4.818; P<0.05). The summer (OR, 0.986; 95% CI, 0.491–1.980; P=0.969) and the fall seasons (OR, 1.084; 95% CI, 0.552–2.132; P=0.814) were not significant. A prior local clinic visit (OR, 3.095; 95% CI, 1.938–4.830; P<0.05) and admission course (OR, 1.263; 95% CI, 1.108–1.440; P<0.05) were significant predictors. The symptom duration (OR, 2.592; 95% CI, 1.780–3.775; P<0.05) was also a significant predictor of delayed diagnosed appendicitis. The migration of pain, nausea, vomiting, anorexia, RLQ tenderness, and RLQ rebound tenderness resulted in an increase in a delayed diagnosis of appendicitis but they had no statistical significance. Only the symptom of fever (OR, 1.374; 95% CI, 1.046–1.805; P<0.05) and diarrhea (OR, 1.935; 95% CI, 1.083–3.458; P<0.05) were found to be significant risk factors for a delayed diagnosis of appendicitis. In the laboratory test, the odds of a delayed diagnosis of appendicitis increased according to increasing CRP (OR, 1.474; 95% CI, 1.194–1.819; P<0.05), but increasing WBC or PMNL counts were not statistically significant.
Table 6. Risk factors of delayed diagnosis of acute appendicitis.
| Variable | P value | OR (95% CI) |
|---|---|---|
| Age | 0.463 | 0.89 (0.66–1.21) |
| Sex | 0.135 | 1.38 (0.91–2.09) |
| Body mass index | 0.125 | 0.78 (0.56–1.07) |
| Season | 0.004 | 2.54 (1.34–4.82) |
| Prior local clinic visit | <0.001 | 3.09 (1.98–4.83) |
| Admission course | <0.001 | 1.26 (1.11–1.44) |
| Symptom duration | <0.001 | 2.59 (1.78–3.78) |
| Migrating pain | 0.350 | 1.39 (0.69–2.79) |
| Fever | 0.022 | 1.37 (1.05–1.81) |
| Nausea | 0.659 | 1.12 (0.69–1.81) |
| Vomiting | 0.873 | 1.04 (0.65–1.66) |
| Diarrhea | 0.026 | 1.94 (1.08–3.46) |
| Anorexia | 0.495 | 1.33 (0.59–2.99) |
| RLQ Tenderness | 0.075 | 0.55 (0.29–1.06) |
| RLQ Rebound tenderness | 0.063 | 0.64 (0.39–1.03) |
| WBC | 0.831 | 0.97 (0.71–1.32) |
| PMNL | 0.612 | 0.85 (0.45–1.60) |
| CRP | <0.001 | 1.47 (1.19–1.82) |
| PAS | 0.882 | 0.98 (0.80–1.21) |
| Hospital day | <0.001 | 1.88 (1.46–2.43) |
OR, odds ratio; CI, confidence interval; RLQ, right lower quadrant; WBC, white blood cell; PMNL, polymorphonuclear leukocyte; CRP, C-reactive protein; PAS, pediatric appendicitis score.
Discussion
In this study, the risk factors of a diagnostic delay for appendicitis were found to be seasonal variations, prior medical visits, admission course, symptom duration, fever, and diarrhea. CRP was associated with a delayed diagnosis of appendicitis.
Despite the numerous publications on the appropriate evaluation and treatment of acute appendicitis, the diagnosis of this condition is often complicated in children. The classic progression of symptoms is well recognized. Unfortunately, this progression does not always occur, physicians find difficulty in recognizing the uncommon presentation. Nonspecific symptoms, intermittent abdominal complaints, and parental delay also have been described to cause diagnostic delays12). Such diagnostic delays can result in rupture, abscess formation, wound complications, and prolonged hospital stay. Early diagnosis and intervention remain the most promising means of reducing the morbidity, mortality, and discomforts for the child, as well as the cost. This study attempted to determine the underlying factors of a delay in the diagnosis of acute appendicitis.
Addiss et al.15) reported a seasonal variation of appendicitis in an epidemiologic analysis with 11% more cases occurring from May to August compared to November through February. On the other hand, little is known regarding the seasonal variations in diagnosing appendicitis. In the present study, seasonal variations are a significant predictor of a delayed diagnosis of appendicitis, particularly from March to May. Generally from March, doctors start to work in their new position and considering the result that most of the children (81.6%) who underwent appendectomies are admitted through ED, a physician with little experience can make a delayed diagnosis. This is because the diagnosis of appendicitis is still primarily a clinical one and is dependent on the physician's skill in eliciting the patient's history and appreciating its significance16).
This study showed that children in the delayed diagnosed group have more history of a prior visit to local clinics. This is one of the risk factors of a diagnostic delay for appendicitis and presents the highest odds ratio among the other associated factors. Von Titte et al.16) reported that approximately one-fourth of patients with perforated appendicitis had a prior medical visit within 48 hours of an appendicitis diagnosis, possibly due to the high potential for symptom miscommunication in the youngest children. Harrison et al.17) reported that primary care physicians referred patients with symptoms for a longer period of time and who ultimately were found to have a more advanced stage of the disease than patients referred from an ED. Both the primary physician and parents must recognize that children's symptoms are abnormal and require further medical evaluations. Nevertheless, a lack of verbal skills necessary to accurately present appendicitis-related symptoms and the nonspecific symptoms at the early stage often misdiagnose appendicitis as gastroenteritis3).
The duration of symptoms is a predictor diagnostic delay. Most children visited the authors' hospital within 3 days after symptoms onset. In diagnostic delay group, however, they had a significant longer duration of symptoms. Bickell et al.18) reported that some of the prolonged times after patients accessed care appeared to be associated with the uncertainty of diagnosis and some with the use of imaging studies. These results were attributed to children in the delayed group being referred after being treating in primary clinics for several days or physicians were concerned about various differential diagnoses when the clinical signs were not explicit, and this make it difficult to determine an acute abdomen in children.
Among the various symptoms, in the present study, fever and diarrhea were risk factors of a delayed diagnosis of appendicitis. Fever and diarrhea are common symptoms that can also be indicative of gastroenteritis or other infectious disease. Patients with gastroenteritis may have abdominal pain accompanied by nausea, vomiting, diarrhea or fever. Physicians must realize that the signs and symptoms of appendicitis change during the physiological course of the disease. Cappendijk and Hazebroek13) reported that diarrhea resulted in a diagnosis of gastroenteritis in almost half of the cases and greatly influenced the diagnostic delay. Gamal and Moore19) presented a table showing that diarrhea is very often a concomitant symptom in appendicitis, but failed to acknowledge this as a significant symptom. Migrating pain, nausea, vomiting and anorexia were not helpful in predicting a diagnostic delay.
Although the WBC count is frequently ordered in children with suspected appendicitis, it is nonspecific and insensitive to this disorder. The WBC are unable to discriminate between patients with and without appendicitis20). In present study, there were no significant differences in the laboratory test results between the delayed group and nondelayed group. In regression analysis, only CRP was associated with a delayed diagnosis of appendicitis. Patient's longer symptom duration, fever, diarrhea were factors associated with increasing in CRP. However, the perception that CRP is another nonspecific inflammatory mediator may be a cause of delayed diagnosis of appendicitis. A combination of CRP and WBC made a positive likelihood ratio up to 23.32 from 4.2421). In cases of an increase in CRP with or without leukocytosis or neutrophilia physicians must consider appendicitis.
This study had some limitations. First, this study was a single hospital based retrospective analysis. Identifying the factors associated with a delayed diagnosis of appendicitis may be impaired by poor documentation regarding the patient's presentation in the electrical medical chart. In addition, the patient's history and review of symptoms were not standardized. Therefore, the data may be incomplete or inaccurate. Specific presenting symptoms such as migrating pain may have been omitted in some patients. This study only included patients who had undergone appendectomies, hence, patients determined to have appendicitis but were treated nonsurgically were missed. Also, the present study did not analyze the effect of a combination of laboratory values to distinguish the delayed group from the nondelayed group.
In conclusion, 14.7% of children who underwent an appendectomy had a delayed diagnosis of appendicitis. The risk factors of a delayed diagnosis of appendicitis were found to be seasonal variations, prior medical visits, admission course, symptom duration, fever, diarrhea and CRP. The postoperative complications and PAS were not an associated factor. Appendicitis patients with nonspecific symptoms are always a concern. These results highlight the need for physicians who start to work in ED recognize the possibility of appendicitis. Repeated history taking and follow-up by physicians will be helpful for avoiding delayed diagnoses.
Footnotes
Conflict of interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Pittman-Waller VA, Myers JG, Stewart RM, Dent DL, Page CP, Gray GA, et al. Appendicitis: why so complicated? Analysis of 5755 consecutive appendectomies. Am Surg. 2000;66:548–554. [PubMed] [Google Scholar]
- 2.Erdem H, Çetinkünar S, Daş K, Reyhan E, Deger C, Aziret M, et al. Alvarado, Eskelinen, Ohhmann and Raja Isteri Pengiran Anak Saleha Appendicitis scores for diagnosis of acute appendicitis. World J Gastroenterol. 2013;19:9057–9062. doi: 10.3748/wjg.v19.i47.9057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rothrock SG, Pagane J. Acute appendicitis in children: emergency department diagnosis and management. Ann Emerg Med. 2000;36:39–51. doi: 10.1067/mem.2000.105658. [DOI] [PubMed] [Google Scholar]
- 4.Rothrock SG, Skeoch G, Rush JJ, Johnson NE. Clinical features of misdiagnosed appendicitis in children. Ann Emerg Med. 1991;20:45–50. doi: 10.1016/s0196-0644(05)81117-5. [DOI] [PubMed] [Google Scholar]
- 5.Curran TJ, Muenchow SK. The treatment of complicated appendicitis in children using peritoneal drainage: results from a public hospital. J Pediatr Surg. 1993;28:204–208. doi: 10.1016/s0022-3468(05)80276-3. [DOI] [PubMed] [Google Scholar]
- 6.Graff L, Russell J, Seashore J, Tate J, Elwell A, Prete M, et al. False-negative and false-positive errors in abdominal pain evaluation: failure to diagnose acute appendicitis and unnecessary surgery. Acad Emerg Med. 2000;7:1244–1255. doi: 10.1111/j.1553-2712.2000.tb00470.x. [DOI] [PubMed] [Google Scholar]
- 7.Reynolds SL. Missed appendicitis in a pediatric emergency department. Pediatr Emerg Care. 1993;9:1–3. doi: 10.1097/00006565-199302000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Barker AP, Davey RB. Appendicitis in the first three years of life. Aust N Z J Surg. 1988;58:491–494. doi: 10.1111/j.1445-2197.1988.tb06241.x. [DOI] [PubMed] [Google Scholar]
- 9.Williams N, Kapila L. Acute appendicitis in the under-5 year old. J R Coll Surg Edinb. 1994;39:168–170. [PubMed] [Google Scholar]
- 10.O'Toole SJ, Karamanoukian HL, Allen JE, Caty MG, O'Toole D, Azizkhan RG, et al. Insurance-related differences in the presentation of pediatric appendicitis. J Pediatr Surg. 1996;31:1032–1034. doi: 10.1016/s0022-3468(96)90079-2. [DOI] [PubMed] [Google Scholar]
- 11.Golladay ES, Sarrett JR. Delayed diagnosis in pediatric appendicitis. South Med J. 1988;81:38–42. doi: 10.1097/00007611-198801000-00008. [DOI] [PubMed] [Google Scholar]
- 12.Buchman TG, Zuidema GD. Reasons for delay of the diagnosis of acute appendicitis. Surg Gynecol Obstet. 1984;158:260–266. [PubMed] [Google Scholar]
- 13.Cappendijk VC, Hazebroek FW. The impact of diagnostic delay on the course of acute appendicitis. Arch Dis Child. 2000;83:64–66. doi: 10.1136/adc.83.1.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Samuel M. Pediatric appendicitis score. J Pediatr Surg. 2002;37:877–881. doi: 10.1053/jpsu.2002.32893. [DOI] [PubMed] [Google Scholar]
- 15.Addiss DG, Shaffer N, Fowler BS, Tauxe RV. The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol. 1990;132:910–925. doi: 10.1093/oxfordjournals.aje.a115734. [DOI] [PubMed] [Google Scholar]
- 16.Von Titte SN, McCabe CJ, Ottinger LW. Delayed appendectomy for appendicitis: causes and consequences. Am J Emerg Med. 1996;14:620–622. doi: 10.1016/S0735-6757(96)90074-1. [DOI] [PubMed] [Google Scholar]
- 17.Harrison MW, Lindner DJ, Campbell JR, Campbell TJ. Acute appendicitis in children: factors affecting morbidity. Am J Surg. 1984;147:605–610. doi: 10.1016/0002-9610(84)90123-5. [DOI] [PubMed] [Google Scholar]
- 18.Bickell NA, Aufses AH, Jr, Rojas M, Bodian C. How time affects the risk of rupture in appendicitis. J Am Coll Surg. 2006;202:401–406. doi: 10.1016/j.jamcollsurg.2005.11.016. [DOI] [PubMed] [Google Scholar]
- 19.Gamal R, Moore TC. Appendicitis in children aged 13 years and younger. Am J Surg. 1990;159:589–592. doi: 10.1016/s0002-9610(06)80073-5. [DOI] [PubMed] [Google Scholar]
- 20.Eriksson S, Granström L, Carlström A. The diagnostic value of repetitive preoperative analyses of C-reactive protein and total leucocyte count in patients with suspected acute appendicitis. Scand J Gastroenterol. 1994;29:1145–1149. doi: 10.3109/00365529409094902. [DOI] [PubMed] [Google Scholar]
- 21.Andersson RE. Meta-analysis of the clinical and laboratory diagnosis of appendicitis. Br J Surg. 2004;91:28–37. doi: 10.1002/bjs.4464. [DOI] [PubMed] [Google Scholar]