Abstract
Background
Metal-on-Metal (MoM) total hip arthroplasties (THA) are associated with pseudotumor formation and high revision rates. This prospective study analysed the clinical and wear analyses of 9 large Metal-on-Metal (MoM) total hip arthroplasties (THA) to understand the underlying mechanisms of failure. The MoM bearings were revised for multiple reasons; the main reason was pseudotumor formation.
Materials and Methods
From 2006 till 2010 the Reinier de Graaf Hospital implanted 160 large head M2a-Magnum™ (Biomet Inc. Warsaw, Indiana, USA) THAs in 150 patients. The first year, 9 bearings were revised and analysed at the Biomechanics Section, Hamburg University of Technology, Germany. We performed clinical (Harris Hip Score, radiographic analysis, blood cobalt and chromium) and wear analysis (implant, tissue and fluid) of the 9 bearings. Since this study did not fall under the scope of the Medical Research Involving Human Subjects Act in The Netherlands, no ethical approval was necessary. In this prospective study all patient details were anonymized by the corresponding author, all other authors were blinded during the research and wear analyses. Patients with bilateral MoM implants were excluded.
Results
The 9 bearings had a median (IQR) survival of 41.0 (25) months in situ. From these bearings, three showed no noticeable wear. The median (IQR) head wear volume was 3.2 (3.6) mm3 and maximum wear depth 0.02 (0.02) mm. For the cup the median (IQR) wear volume was 0.23 (0.3) mm3 with a maximum wear depth of 0.03 (0.05) mm.
Conclusion
An early identification of parameters related to failure of the MoM THA, such as pain, decreased range of motion, radiographic changes and high levels of blood cobalt and chromium is of great importance for patient’s quality of life. Especially now patients and surgeons face the long term effects of all these bearings still in situ. This study reports the clinical and wear analyses of 9 MoM THA. In the majority of this group the reason for revision was pseudotumor formation. Most bearings showed signs of wear, however with a great diversity in clinical analysis, in inclination angle, serum cobalt and chromium levels as well as wear analysis. For a better understanding of the underlying mechanisms related with failure, more wear analyses of revised MoM bearings are necessary as well as a frequent follow-up of the patients with a MoM bearing.
Introduction
The Dutch Orthopaedic Association (Nederlandse Orthopedische Vereniging) decided in the beginning of 2011 to do a recall of all MoM articulations in The Netherlands. Their advice included active recall of all MoM hip implants as well as an active follow–up. This decision was made after multiple studies had shown high revision rates with the MoM THA by early failures and pseudotumor formation due to metal debris by high wear and edge loading [1–4]. In 2009 almost 35% of the 270.000 hip replacements in the USA were MoM bearings [1, 5]. In England, an estimated number of more than 60.000 patients have received a MoM THA since2003[6].
The metal debris can lead to elevated serum levels of cobalt and chromium and tissue reactions around the prosthesis, described as ‘Aseptic Lymphocyte dominated Vasculitis Associated Lesion’ (ALVAL), also known as pseudotumor [2]. The high wear and edge loading might be the result of suboptimal positioning or poor design of the components [7, 8]. Especially excessive inclination, with an inclination angle greater than 55 degrees as well as a small size of the cup, increases the edge loading. This edge loading might lead to high wear and local debris and is related to increased serum cobalt and chromium levels.[9, 10]. Furthermore, edge loading is proposed to have a relation to wear of modular taper interfaces [11].
The wear rates of the retrieved MoM bearings vary widely. First reports showed a low wear rate of 0.3mm3 per year [12, 13]. However, latest reports of MoM hip resurfacings and total hip prosthesis show high wear rates up to 6mm3 per year [14, 15].
This study describes the clinical and biological analysis of 9 patients with revised MoM THAs. We performed wear analysis of the 9 revised implants to relate the wear rate to our clinical and biological findings to help understanding the underlying mechanisms of failure.
Materials and Methods
Patient Demographics
In the Reinier de Graaf Hospital (Delft, The Netherlands) 160 primary large head MoM articulations were implanted in 150 patients between 2006 till 2010. Data and survival analysis of our cohort are written elsewhere [16]. From the 160 bearings placed in our facility, fifteen were revised of which two patients had bilateral MoM bearings. Thirteen of these implants were revised after the recall and 9 of these bearings were analyzed for this prospective study at the Biomechanics Section, Hamburg University of Technology, Germany. From these 9 bearings, seven were revised due to pseudotumor formation and in two cases progressive pain was the indication. Six of the patients were female and the mean age at primary surgery was 57 years (range 22–72 years). The median (IQR) time in situ was 41.0 (25) months. All components; cup, head and insert were revised, in one case the stem was also revised. The median (IQR) cup size was 52 (2) mm and head size 46 (2) mm. All patient demographic features are shown in Table 1. Patient no 9 had bilateral MoM THA, of which the right hip is revised.
Table 1. Patient demographics of the 9 revised bearings.
| Ptn | Age | Gender | YoO | Indication | Headsize | Stem name | Pain | HHS | Diagnosis | Inclination angle(degrees) | Co levels(nmol/l) | Cr levels(nmol/l) | Histology |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. | 57 | F | 2007 | OA | 46 | Mallory | no | 70>80 | Tumor | 47.69 | 22,9 | 18,4 | Pseudotumor |
| 2. | 58 | F | 2007 | OA | 48 | Taperloc | yes | 60>70 | Tumor/ Loosening | 59.11 | 1431,2 | 510,9 | Not performed |
| 3. | 60 | F | 2007 | OA | 46 | Taperloc | yes | 90>100 | Tumor | 59.44 | 80,9 | 67,4 | Not performed |
| 4. | 65 | F | 2008 | OA | 46 | Mallory | yes | 60>70 | Tumor | 35.81 | 13,6 | 6,5 | Not performed |
| 5. | 57 | F | 2009 | OA | 46 | Taperloc | no | 80>90 | Tumor | 52.07 | 80,8 | 100,1 | Pseudotumor |
| 6* | 59 | M | 2009 | AVN | 56 | Taperloc | yes | 70>80 | Loosening | 32.49 | 22,1 | 35,9 | Pseudotumor |
| 7* | 72 | M | 2009 | OA | 46 | Taperloc | yes | <60 | Pain | 26.62 | 13,6 | 14 | Pseudotumor |
| 8. | 22 | M | 2009 | Pseudoarthrosis | 46 | Mallory | yes | 70>80 | Tumor | 41.59 | 26,8 | 58,6 | No clear diagnose |
| 9** | 67 | F | 2009 | OA | 48 | Taperloc | no | 90>100 | Tumor | 40.14 | 283,9 | 149,6 | Pseudotumor |
Patients
* marked had no pseudotumor.
** Bilateral MoM THA.
Abbreviations: Ptn = Patientnumber, YoO = Year of Operation, HHS = Harris Hip Score, Co = Cobalt, Cr = Chromium, OA = Osteoarthritis
Since this prospective study did not fall under the scope of the Medical Research Involving Human Subjects Act in The Netherlands, no ethical approval was necessary. In this study all patient details were anonymized by the corresponding author, all other authors were blinded during the research and wear analyses. Patients with bilateral MoM implants were excluded in measurements.
Implants and operative technique
All patients received the Biomet Magnum (M2a-Magnum™) prostheses with Recap cup and Taperloc (Taperloc® Hip Stem) or Mallory stem (Mallory®) (Biomet inc. Warsaw Indiana, USA). The implants were implanted by two surgeons (one of the co-authors) and the selection of the type of implant was based on experience of the surgeon. Seven operations were performed through an anterior supine intermuscular approach and two (patient 1 and 8) through a straight lateral approach. During the first twenty four hours postoperatively antibiotic prophylaxis was given and patients received low-molecular-weight heparin for 6 weeks.
Clinical analysis
All patients were examined clinically and asked if they experienced pain in the groin, suffer from deafness, dizziness, fear behavior/depression or experienced neurological problems after surgery. Additionally, the Harris Hip Score (HHS), a score to assess the results of hip replacement, and physical examination, all taken by one doctor, were used to evaluate all patients (S1 Fig). The HHS was divided into 5 categories (90 > 100 excellent, 80 > 90 good, 70 > 80 fair, 60 > 70 poor, <60 really poor) and used as one of our outcome measurements.
Anteroposterior pelvic and lateral hip radiographs were obtained and criticized by a specialized one radiologist. Radiographs were assessed for radiolucency, component migration, osteolysis and/or bone resorption. Lateral cup inclination was measured by two authors (MCK, NM) by using the transischial line and a second line drawn across the rims of the cup. Also, all patients had received an ultrasound exam of the hip by one specialized radiologist and additional MARS-MRI or CT-scan. Fluid components or mass on ultrasound or reactive masses on MARS-MRI /CT-scan were highly suspected for pseudotumor formation.
Metal ion analysis
Blood was sampled from all patients in trace-element free tubes. Whole blood Cobalt (Co) and Chromium (Cr) levels (nmol/l) were measured by mass spectrometry (Atomaire Absorption Spectrometry, Thermo Elemental, Solaar M6, 2001, England). Advised by the Dutch Orthopeadic Association, the cobalt ranges were set as normal <40 nmol/l (< 2 mmg/L), normal high 40–85 nmol/l (2–5 mmg/L), high 85–170 nmol/l (5–10 mmg/L) and extreme high >170 nmol/l (> 10 mmg/L).
Wear Measurement
Analysis of the bearings consisted of digital photographs and wear measurements. The surface geometry of each component was determined with the use of a coordinate measurement machine Mitutoyo BHN 305 (Mitutoyo Deutschland GmbH, Neuss, Germany). By using a 2 mm ruby tip all surfaces were scanned. The original surfaces were estimated by fitting unworn surfaces to regions of the measured surface which is unworn. For assessing bearing wear the geometrical from of a sphere was applied for fitting. Conical surface was calculated the same way, whereby the geometrical form of a cone was applied. Volumetric wear was quantified by comparison with an assumed initial geometry. Mathematical methods used are described in detail elsewhere [17, 18]. The red marked bearing and taper surfaces (Fig 1) were analysed.
Fig 1. The red marked bearing and taper surfaces in the picture bellow were analysed.
Tissue and Fluid analysis
During revision surgery, tissue and liquid samples around the joint of 6 patients were taken to determine cobalt, chromium and titanium concentrations. Samples were freeze-dried and crushed with a scalpel. 100 mg samples were digested by microwaves (ELAN DRC II and Optima7000DV ICP-OES, PerkinElmer, Inc. Waltham, MA, USA). Two samples were taken from the solution, separately analyzed and the results averaged.
Results
Clinical analysis
The mean Harris Hip Score was ‘fair’ (70 > 80). Patients revised because of pain scored a lower HHS (60>70) compared to the other revisions. Seven patients (77.8%) experienced pain in the groin, and 2 (22.2%) patients noted a swelling around the joint. None of the analysed patients showed neurological signs, signs of deafness or dizziness. Only one patient complained of fear during mobilisation which was related to the pain in the groin. Six patients complained of groin pain of which only four had pseudotumor formation. Three patients, all female, with pseudotumor tissue had no groin pain. This despite their serum increased ion level of cobalt and chromium and the wear in both cup and head.
Radiographic analysis
The anteroposterior pelvic and lateral hip radiographs of patient 2 and 6 showed signs of loosening of the cup. All the other anteroposterior pelvic and lateral hip radiographs showed no signs of bone resorption, lysis or fractures. The lateral cup inclination had a median (IQR) angle of 41.2 (21.4) degrees. Patients diagnosed with pseudotumor formation scored a median (IQR) inclination angle of 47.7 (23.3) degrees. In our total cohort of 160 prostheses the mean (SD) inclination angle was 40.9 (7.3) degrees [16].
Ultrasound analysis
Ultrasound was performed in 8 patients from our study group. Signs of pseudotumor were observed in 2 of these patients. Moreover, four patients showed liquid accumulation inside the joint or capsule. In one patient ultrasound was not performed, but CT and MRI was done immediately.
Metal ion analysis
The median level of serum cobalt was 24.9 nmol/l with an interquartile range (IQR) of 65.15 nmol/l. For chromium a median of 47.3 nmol/l (IQR 76.8nmol/l) was found. Patients with a pseudotumor showed a median level of serum cobalt of 53.8 nmol/l (IQR 397.9nmol/l) and chromium of 63.0 nmol/l (IQR 187.4nmol/l).
CT and MARS-MRI
A total of 6 MARS-MRI’s and 3 CT-scans were obtained of which 1 patient had both (patient no 9). In two cases CT-scan showed a possible pseudotumor. MARS-MRI showed in 5 cases a possible pseudotumor (see Table 1). CT-scan of patient number 7 showed no signs of pseudotumor. Patient no 6 had no CT or MRI investigation.
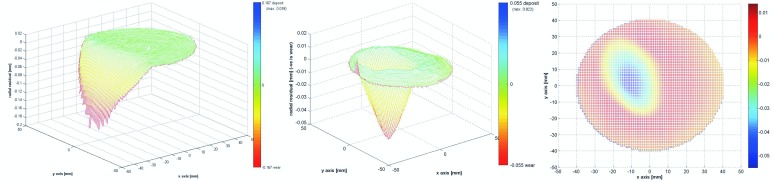
Wear Analysis
Table 2 shows the wear analyses of all nine bearings. In three bearings no noticeable head wear was found. The median (IQR) head wear volume was 3.2 (3.6) mm3 and maximum wear depth 0.02 (0.02) mm. For the cup the median (IQR) wear volume was 0.23 (0.3) mm3 with a maximum wear depth of 0.03 (0.05) mm. Only one bearing, no 2, showed massive bearing wear. Notable cup wear of 28 mm3 and head wear 24.4mm3. Fig 2 shows the wear plots of this bearing. Clear inner sleeve taper wear was only seen in patient 9 (Table 2).
Table 2. Head, cup and taper wear in the revised bearings.
| Ptn | Head wear | Cup wear | Inner Sleeve Taper wear | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Wear Area Ratio [%] | Wear Volume [mm3] | Wear per Year [mm3] | Wear Area Ratio [%] | Wear Volume [mm3] | Wear per Year [mm3] | Deposits [mm3] | Wear Volume [mm3] | Wear per Year [mm3] | |
| 1. | 6.382 | 1.209 | 0.2267 | 2.910 | 0.315 | 0.0591 | 0.078 | 0.000 | 0.000 |
| 2. | 24.561 | 24.424 | 4.8047 | 20.575 | 27.998 | 5.5078 | 0.208 | 0.000 | 0.000 |
| 3. | 13.042 | 4.486 | 0.9444 | 1.884 | 0.302 | 0.0636 | 0.002 | 0.000 | 0.000 |
| 4. | 0.035 | 0.004 | 0.0009 | 0.000 | 0.000 | 0.000 | 0.041 | 0.000 | 0.000 |
| 5. | 11.910 | 3.657 | 1.0703 | 0.000 | 0.000 | 0.000 | 0.118 | 0.000 | 0.000 |
| 6* | 13.701 | 3.281 | 1.1931 | 0.000 | 0.000 | 0.000 | 0.266 | 0.041 | 0.0149 |
| 7* | 0.000 | 0.000 | 0.000 | 1.825 | 0.178 | 0.0548 | 0.078 | 0.000 | 0.000 |
| 8. | 6.484 | 0.930 | 0.310 | 2.302 | 0.260 | 0.0867 | 0.166 | 0.000 | 0.000 |
| 9** | 9.210 | 3.204 | 1.1651 | 1.060 | 0.232 | 0.0844 | 3.074 | 0.172 | 0.0625 |
Patients
* marked had no pseudotumor.
** Bilateral MoM THA.
Abbreviation: Ptn = patientnumber
Fig 2. Wear plot graphs of the cup (most left) and head (middle and right) of patient no 2. 70% points used for estimation of wear.
The green area represents the estimated original surface. The red area represents the wear and is defined as a negative deviation from the original surface.
Tissue and Fluid Analysis
The tissue and fluid analysis shows a great diversity between the bearings (Table 3). The largest difference is seen in the titanium tissue samples. The median (IQR) amount of titanium in the tissue is 168.5 (3327.2) mg/kg. Tissue analysis also showed a large amount of chromium with a great diversity between the samples. The median (IQR) of chromium was 6.9 (744.3)mg/kg. The other results are shown in Table 3.
Table 3. Tissue and fluid analyses of 6 revised bearings.
| Ptn | Type | Co (mg/Kg) | Cr (mg/Kg) | Ti (mg/Kg) |
|---|---|---|---|---|
| 1. | TissueFluid | 44.3 1.11 | 29.8 0.77 | 1347<10 |
| 2. | Tissue Fluid | 204 3.97 | 2945 26.37 | 9468<10 |
| 3. | Tissue Fluid | 7.90 0.52 | 36.35 1.74 | 182 <10 |
| 4. | Tissue Fluid | 5.34 <0.1 | 24.4 0.27 | 155 <10 |
| 5. | Tissue Fluid | 9.6 91.56 | 48.7 4.24 | <50 <10 |
| 7* | Tissue Fluid | 15.6 0.13 | 37.5 0.27 | <50 <10 |
| Median (IQR) | Tissue Fluid | 12.6 (77.0) 0.8 (2.0) | 36.9 (744.3) 1.3 (9.5) | 168.5 (3327.2) 10 (0) |
Patient
* marked had no pseudotumor.
Abbreviations: Ptn = patientnumber, Co = Cobalt, Cr = Chromium, Ti = titanium
Discussion
Survival of large MoM THAs has decreased by early failures and pseudotumor formation. Analysis of revised MoM THA shows a wide variation in wear rates and also pseudotumor formation in the absence of high wear [2, 4, 19]. A better understanding of failure, wear rate and clinical presentation is relevant to predict the outcome of MoM THA’s. We described the clinical and wear analysis of a small group of 9 MoM THA implanted in our clinic from 2007 till 2009. Seven prostheses were revised due to pseudotumor formation, two other prostheses because of pain and loosening.
Pseudotumors seem to be associated with high wear and metal hypersensitivity [20, 21], however a clear association has not been seen yet. According to Edward et al. the histopathological changes in the tissue cannot be explained by high wear alone [19]. There are also several reports of MoM THA failure and adverse local tissue reactions in patients with the absence of high wear [2, 4, 22]. In these patients a hypersensitivity reaction to the metal is more likely and results in aseptic lymphocytic vasculitis-associated lesions [23]. However, reducing the amount of wear might prevent this reaction and possibly reduce the formation of pseudotumors. This is also of importance for all other bearings. The most important predictor of wear rate is edge loading [24]. Edge loading is caused by high cup inclination, cup version, cup and head version, head-neck ratio, cup design and more variables. Some studies show excessive inclination, with an inclination angle greater than 55 degrees and a small size, increases the edge loading and might lead to high wear and local debris. An inclination of the acetabular component of more than 55 degrees is also related to increased serum cobalt and chromium levels [9, 10]. According to Hart et al, high cup inclination can even be a predictor of high wear rate [24]. The effects of metal wear particles and elevated serum metal have been documented but are still not understood [25]. High serum levels of cobalt and chromium were known and evolved during the running-in phase of the prostheses [26].
A clear correlation between the serum ion levels of cobalt and chromium and wear rate was not found in this study. This is in accordance with the findings of de Smet et al and Hart et al. [24, 27]. However, a trend in high inclination and increased metal ion levels could be observed (Table 1).
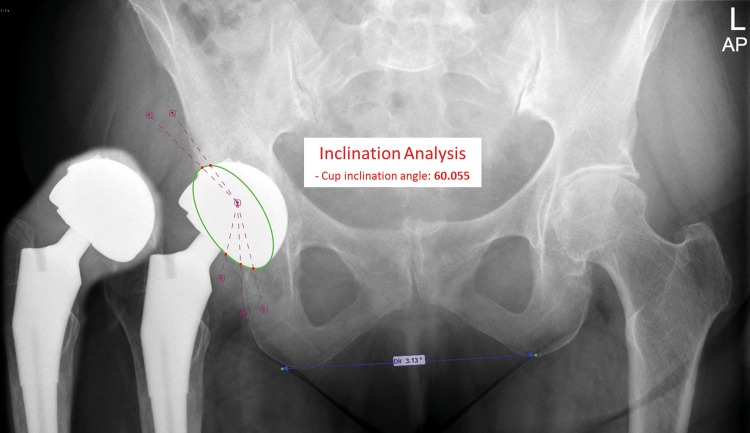
In our small group, two patients (patient no 2 and 3) had a cup inclination angle over the 55 degrees. Both patients also show the highest cup wear area ratio (Table 2). However, high wear was also seen with an inclination angle of 47.7 and 32.5 degrees. The patients with high head wear ratio also showed an increased serum level of cobalt and chromium. Especially patient no 2 with an inclination angle of 60 degrees (Fig 3), a head wear ratio of 24.4 mm3 and a cup wear ratio of 28.0 mm3 showed highly increased cobalt and chromium levels (Table 1). These results show again the importance of a good positioned acetabular component especially to prevent the high edge loading and increase in serum and tissue ion levels as mentioned above.
Fig 3. Anteroposterior radiograph of the pelvic from patient no 2 with the MoM total hip replacement on the right.
The acetabular inclination angle was estimated 60 degrees and the anteversion angle 31 degrees.
The fluid and tissue analysis showed highly increased levels of cobalt and chromium in all patients. Thereby, even more striking is the high titanium level in the tissue of patient 1 and 2. These high levels of titanium indicate “trunniosis” in the taper-stem junction because only these two components consist of titanium alloys. Trunniosis, or cold-welding, is a phenomenon seen in the large head bearings, mostly above the 40mm [28–30]. More stress load on the modular interface at the larger head bearings implies more corrosion and debris, especially titanium. In our cases, no clear wear at the inner sleeve taper was found and stem wear analyses were not performed because the stem stayed in situ during the revision surgery. However, the large amount of titanium in fluid and tissue suggests wear at the taper-stem junction.
As shown above, the exact mechanisms for failure and pseudotumor formation are still not completely understood. Whether the failure is due to high cup inclination, edge loading, trunniosis, due to patient characteristics or a combination of all above, more wear analyses of revised bearings might help finding the answers. This study has several limitations. The clinical analyses as well as the wear analyses differs greatly. Furthermore, the gender ratio, age as well as the surgical technique varies within this small group. We also used two different stem types in our analysis. These sources may all bias the clinical and wear analysis and therefore limit the results of this study.
However, we can state all precautions should be taken for close monitoring and frequent control of MoM THA. Focussing on the clinical presentation can be misleading in decision making. Serum ion levels of cobalt, chromium (and titanium), radiographic control and MARS-MRI are all necessary for close monitoring. An example and flowchart for close monitoring and follow up is described earlier by our research group [16]. A better understanding of the process after implant placement in relation to clinical features, serum ion levels, pseudotumor formation and failure of the implant is necessary. Especially now we are facing the long term effects of the MoM THA’s still in situ.
Supporting Information
(PDF)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Smith AJ, Dieppe P, Vernon K, Porter M, Blom AW. Failure rates of stemmed metal-on-metal hip replacements: analysis of data from the National Joint Registry of England and Wales. Lancet. 2012;379(9822):1199–204. Epub 2012/03/16. 10.1016/S0140-6736(12)60353-5 . [DOI] [PubMed] [Google Scholar]
- 2.Campbell P, Ebramzadeh E, Nelson S, Takamura K, De Smet K, Amstutz HC. Histological features of pseudotumor-like tissues from metal-on-metal hips. Clin Orthop Relat Res. 2010;468(9):2321–7. Epub 2010/05/12. 10.1007/s11999-010-1372-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cohen D. Revision rates for metal on metal hip joints are double that of other materials. BMJ. 2011;343:d5977 Epub 2011/09/23. 10.1136/bmj.d5977 . [DOI] [PubMed] [Google Scholar]
- 4.Pandit H, Glyn-Jones S, McLardy-Smith P, Gundle R, Whitwell D, Gibbons CL, et al. Pseudotumours associated with metal-on-metal hip resurfacings. The Journal of bone and joint surgery British volume. 2008;90(7):847–51. Epub 2008/07/02. 10.1302/0301-620X.90B7.20213 . [DOI] [PubMed] [Google Scholar]
- 5.Bozic KJ, Ong K, Lau E, Kurtz SM, Vail TP, Rubash HE, et al. Risk of complication and revision total hip arthroplasty among Medicare patients with different bearing surfaces. Clin Orthop Relat Res. 2010;468(9):2357–62. Epub 2010/02/19. 10.1007/s11999-010-1262-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cohen D. How safe are metal-on-metal hip implants? BMJ. 2012;344:e1410 Epub 2012/03/01. 10.1136/bmj.e1410 . [DOI] [PubMed] [Google Scholar]
- 7.Daniel J, Holland J, Quigley L, Sprague S, Bhandari M. Pseudotumors associated with total hip arthroplasty. J Bone Joint Surg Am. 2012;94(1):86–93. Epub 2012/01/06. 10.2106/JBJS.J.01612 . [DOI] [PubMed] [Google Scholar]
- 8.Malviya A, Holland JP. Pseudotumours associated with metal-on-metal hip resurfacing: 10-year Newcastle experience. Acta orthopaedica Belgica. 2009;75(4):477–83. Epub 2009/09/25. . [PubMed] [Google Scholar]
- 9.De Haan R, Pattyn C, Gill HS, Murray DW, Campbell PA, De Smet K. Correlation between inclination of the acetabular component and metal ion levels in metal-on-metal hip resurfacing replacement. The Journal of bone and joint surgery British volume. 2008;90(10):1291–7. Epub 2008/10/02. 10.1302/0301-620X.90B10.20533 . [DOI] [PubMed] [Google Scholar]
- 10.Langton DJ, Jameson SS, Joyce TJ, Hallab NJ, Natu S, Nargol AV. Early failure of metal-on-metal bearings in hip resurfacing and large-diameter total hip replacement: A consequence of excess wear. The Journal of bone and joint surgery British volume. 2010;92(1):38–46. Epub 2010/01/02. 10.1302/0301-620X.92B1.22770 . [DOI] [PubMed] [Google Scholar]
- 11.Witt F, Bosker BH, Bishop NE, Ettema HB, Verheyen CC, Morlock MM. The relation between titanium taper corrosion and cobalt-chromium bearing wear in large-head metal-on-metal total hip prostheses: a retrieval study. J Bone Joint Surg Am. 2014;96(18):e157 Epub 2014/09/19. 10.2106/JBJS.M.01199 . [DOI] [PubMed] [Google Scholar]
- 12.Sieber HP, Rieker CB, Kottig P. Analysis of 118 second-generation metal-on-metal retrieved hip implants. The Journal of bone and joint surgery British volume. 1999;81(1):46–50. Epub 1999/03/06. 10.1302/0301-620x.81b1.9047 . [DOI] [PubMed] [Google Scholar]
- 13.Rieker CB, Schon R, Kottig P. Development and validation of a second-generation metal-on-metal bearing: laboratory studies and analysis of retrievals. J Arthroplasty. 2004;19(8 Suppl 3):5–11. Epub 2004/12/04. 10.1016/s0883-5403(04)00516-9 . [DOI] [PubMed] [Google Scholar]
- 14.Campbell P, Beaule PE, Ebramzadeh E, Le Duff MJ, De Smet K, Lu Z, et al. The John Charnley Award: a study of implant failure in metal-on-metal surface arthroplasties. Clin Orthop Relat Res. 2006;453:35–46. Epub 2006/08/15. 10.1097/01.blo.0000238777.34939.82 . [DOI] [PubMed] [Google Scholar]
- 15.Morlock MM, Bishop N, Zustin J, Hahn M, Ruther W, Amling M. Modes of implant failure after hip resurfacing: morphological and wear analysis of 267 retrieval specimens. J Bone Joint Surg Am. 2008;90 Suppl 3:89–95. Epub 2008/08/09. 10.2106/JBJS.H.00621 . [DOI] [PubMed] [Google Scholar]
- 16.Koper MC, Mathijssen NM, Vehmeijer SB. A 5-year survival analysis of 160 Biomet Magnum M2 metal-on-metal total hip prostheses. Hip Int. 2016;26(1):50–6. Epub 2015/11/07. 78601BF0-E929-4FC2-ABA6-EABFDE73AA0B [pii] 10.5301/hipint.5000293 . [DOI] [PubMed] [Google Scholar]
- 17.Morlock MM, Bishop N, Ruther W, Delling G, Hahn M. Biomechanical, morphological, and histological analysis of early failures in hip resurfacing arthroplasty. Proceedings of the Institution of Mechanical Engineers Part H, Journal of engineering in medicine. 2006;220(2):333–44. Epub 2006/05/04. 10.1243/095441105x69015 . [DOI] [PubMed] [Google Scholar]
- 18.Bishop N, Witt F, Pourzal R, Fischer A, Rutschi M, Michel M, et al. Wear patterns of taper connections in retrieved large diameter metal-on-metal bearings. J Orthop Res. 2013;31(7):1116–22. Epub 2013/02/27. 10.1002/jor.22326 . [DOI] [PubMed] [Google Scholar]
- 19.Ebramzadeh E, Campbell P, Tan TL, Nelson SD, Sangiorgio SN. Can wear explain the histological variation around metal-on-metal total hips? Clin Orthop Relat Res. 2015;473(2):487–94. Epub 2014/08/22. 10.1007/s11999-014-3874-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Glyn-Jones S, Roques A, Taylor A, Kwon YM, McLardy-Smith P, Gill HS, et al. The in vivo linear and volumetric wear of hip resurfacing implants revised for pseudotumor. J Bone Joint Surg Am. 2011;93(23):2180–8. Epub 2011/12/14. 10.2106/JBJS.J.01206 . [DOI] [PubMed] [Google Scholar]
- 21.Kwon YM, Glyn-Jones S, Simpson DJ, Kamali A, McLardy-Smith P, Gill HS, et al. Analysis of wear of retrieved metal-on-metal hip resurfacing implants revised due to pseudotumours. The Journal of bone and joint surgery British volume. 2010;92(3):356–61. Epub 2010/03/02. 10.1302/0301-620X.92B3.23281 . [DOI] [PubMed] [Google Scholar]
- 22.Campbell P, Shimmin A, Walter L, Solomon M. Metal sensitivity as a cause of groin pain in metal-on-metal hip resurfacing. J Arthroplasty. 2008;23(7):1080–5. Epub 2008/06/07. 10.1016/j.arth.2007.09.024 . [DOI] [PubMed] [Google Scholar]
- 23.Willert HG, Buchhorn GH, Fayyazi A, Flury R, Windler M, Koster G, et al. Metal-on-metal bearings and hypersensitivity in patients with artificial hip joints. A clinical and histomorphological study. J Bone Joint Surg Am. 2005;87(1):28–36. Epub 2005/01/08. 10.2106/JBJS.A.02039pp . [DOI] [PubMed] [Google Scholar]
- 24.Hart AJ, Muirhead-Allwood S, Porter M, Matthies A, Ilo K, Maggiore P, et al. Which factors determine the wear rate of large-diameter metal-on-metal hip replacements? Multivariate analysis of two hundred and seventy-six components. J Bone Joint Surg Am. 2013;95(8):678–85. Epub 2013/04/19. 10.2106/JBJS.J.01447 . [DOI] [PubMed] [Google Scholar]
- 25.Malviya A, Ramaskandhan J, Holland JP, Lingard EA. Metal-on-metal total hip arthroplasty. J Bone Joint Surg Am. 2010;92(7):1675–83. Epub 2010/07/03. 10.2106/JBJS.I.01426 . [DOI] [PubMed] [Google Scholar]
- 26.van Lingen CP, Ettema HB, Timmer JR, de Jong G, Verheyen CC. Clinical manifestations in ten patients with asymptomatic metal-on-metal hip arthroplasty with very high cobalt levels. Hip international: the journal of clinical and experimental research on hip pathology and therapy. 2013;23(5):441–4. Epub 2013/07/03. 10.5301/hipint.5000054 . [DOI] [PubMed] [Google Scholar]
- 27.De Smet K, De Haan R, Calistri A, Campbell PA, Ebramzadeh E, Pattyn C, et al. Metal ion measurement as a diagnostic tool to identify problems with metal-on-metal hip resurfacing. J Bone Joint Surg Am. 2008;90 Suppl 4:202–8. Epub 2008/11/15. 10.2106/JBJS.H.00672 . [DOI] [PubMed] [Google Scholar]
- 28.Elkins JM, Callaghan JJ, Brown TD. Stability and trunnion wear potential in large-diameter metal-on-metal total hips: a finite element analysis. Clin Orthop Relat Res. 2014;472(2):529–42. Epub 2013/11/13. 10.1007/s11999-013-3244-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lavernia CJ, Iacobelli DA, Villa JM, Jones K, Gonzalez JL, Jones WK. Trunnion-Head Stresses in THA: Are Big Heads Trouble? J Arthroplasty. 2015;30(6):1085–8. Epub 2015/03/01. 10.1016/j.arth.2015.01.021 . [DOI] [PubMed] [Google Scholar]
- 30.Pastides PS, Dodd M, Sarraf KM, Willis-Owen CA. Trunnionosis: A pain in the neck. World J Orthop. 2013;4(4):161–6. Epub 2013/10/23. 10.5312/wjo.v4.i4.161 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.