Abstract
Tonsillar metastatic small cell lung cancer (SCLC) is rare, while anti-Hu antibodies are frequently found in SCLC.
A 66-year-old man was admitted to our hospital with painful dysesthesia and muscle weakness in the distal extremities for over 1 year, progressive dysphagia for over 1 month, and severe cough and dyspnea for over 1 week. He was diagnosed with SCLC accompanied by tonsillar metastasis and anti-Hu antibody-associated paraneoplastic sensory neuropathy (PSN). The patient tolerated 6 cycles of sequential chemoradiotherapy and gradually recovered. The patient's disease remained in remission 2 years after the diagnosis with a remarkable reduction of tumor burden and a persisting high titer of anti-Hu antibodies. To our knowledge, this is the first case of tonsillar metastatic SCLC accompanied by anti-Hu antibody-associated PSN, whereby the anticancer immune response was presumed to play a vital role in disease control.
Unilateral tonsillar metastasis of SCLC accompanied by anti-Hu antibody-associated PSN can occur and in certain circumstances, may have a favorable prognosis.
INTRODUCTION
The tonsil is a rare site in which to find a metastasis, the latter accounting for only 0.8% of all tonsillar tumors, and there is only 1 case of unilateral tonsillar metastasis of small cell lung cancer (SCLC), from left lung to right tonsil, in the scientific literature.1–3 Anti-Hu antibodies are frequently detected in multiple cancers, especially in SCLC, and cause a spectrum of neurological paraneoplastic syndromes, including cerebellar ataxia, limbic encephalitis, Lambert–Eaton syndrome, polyradiculopathy, opsoclonus-myoclonus syndrome, and most commonly, paraneoplastic sensory neuropathy (PSN).4
Here, we present an unusual case of long-term survival in a patient with SCLC accompanied by unilateral tonsillar metastasis and anti-Hu antibody-associated PSN. To our knowledge, this is the first case of a metastatic small cell carcinoma to the tonsil with anti-Hu antibody-associated PSN.
CASE PRESENTATION
In March 2013, a 66-year-old man who was a heavy smoker, presented with painful dysesthesia and muscle weakness in his hands and feet for over 1 year, progressive dysphagia for over 1 month, and severe cough and dyspnea for over 1 week. Physical examination showed a large mass arising from the right tonsil (Figure 1) and several enlarged firm lymph nodes in the right cervical region. Deep tendon reflexes and sensation of the distal extremities were significantly weakened. Lab tests found an increase of neuron-specific enolase (NSE) level (65.2 U/L). Chest computed tomography (CT) demonstrated a mass at the hilum of the left lung, along with severe atelectasis and pleural effusion (Figure 2).
FIGURE 1.

Laryngoscopic findings of the tumor in March 2013. A large mass arising from the right tonsil was covered with fibrin and extended across the midline of the oropharynx, adjoining the epiglottic vallecula.
FIGURE 2.
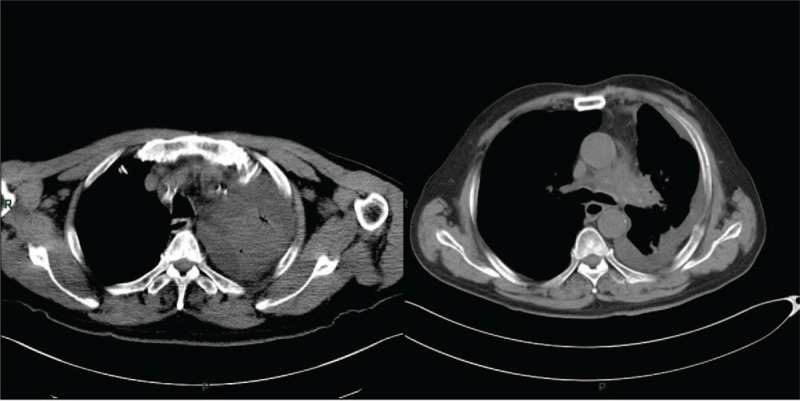
Chest CT scan before chemoradiotherapy performed in March 2013. On admission, chest CT scan revealed a near total consolidation of the left upper lobe, severe pleural effusion and a mass at the hilum of the left lung. CT = computed tomography.
The patient's general condition deteriorated rapidly, and high fever, apnea, and occasional loss of consciousness developed subsequently. Biopsy of the right tonsil revealed a high-grade small cell carcinoma positive for thyroid transcription factor 1. A high titer of anti-Hu antibodies was also detected and subsequent electromyography confirmed the existence of sensory axonal polyneuropathy of the distal extremities. Consequently, tonsillar metastasis of a SCLC with anti-Hu antibody-associated PSN was suspected.
In April 2013, local radiotherapy of the left lung as well as antibiotics was administered to control the symptoms. Later on, systemic chemotherapy with cisplatin and etoposide was introduced. After 2 cycles of sequential chemoradiotherapy, the patient's situation gradually improved, and a fiberoptic bronchoscopy was then successfully carried out. The ensuing histological examination supported the diagnosis of SCLC. At the same time, positron emission tomography-computed tomography (PET-CT) was performed, and a nodule in the left lung was detected, in addition to the right tonsillar mass, which exhibited elevated FDG activity. Meanwhile, brain magnetic resonance imaging found no metastatic deposits in the patient's central nervous system. Therefore, unilateral tonsillar metastasis of SCLC with anti-Hu antibody-associated PSN was diagnosed.
Afterward, the patient received another 4 cycles of chemotherapy by August 2013 and NSE levels dropped into the normal range (∼9.2–10.6 U/L), with a considerable alleviation of his major symptoms. The patient was then discharged and followed up in the clinics every 3 months. Prophylactic cranial irradiation was carried out in January 2014 when the patient was in good condition, and a follow-up CT scan detected recurrent disease neither in the primary site nor in the tonsil. The patient's disease remained in remission and the progression-free survival exceeded 2 years. The CT scan, performed at the latest follow-up in May 2015, revealed a complete regression of the tonsillar mass and a significant shrinkage of the left pulmonary nodule (Figure 3). Despite a significant reduction of tumor burden and a remarkable improvement in his general condition, the titer of anti-Hu antibodies remained high and the patient still complained of numbness and weakness in his distal extremities.
FIGURE 3.
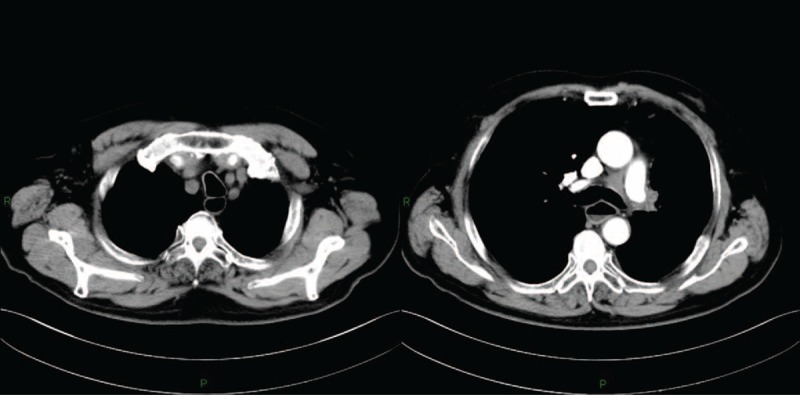
Contrast-enhanced computed tomography scan at follow-up performed in May 2015. Two years after the diagnosis, the pulmonary atelectasis and pleural effusion were completely resolved. The remaining mass close to the left pulmonary artery showed mild enhancement.
DISCUSSION
SCLC accounts for 13% of all newly diagnosed lung cancer cases worldwide and is one of the leading causes of cancer-related death. A majority of patients with SCLC will be diagnosed when there is extensive disease, with metastatic lesions spreading to multiple organs. Distant metastases usually involve the liver, bones, brain, abdominal lymph nodes, adrenal gland, skin, kidneys, and the pancreas.5 Tonsillar metastasis of SCLC is quite rare, with only a few cases reported.1–3,6–8
In various cancers, tumor cells can ectopically express one of the Hu antigens, which are normally expressed throughout the nervous system, and trigger a vigorous immune response, leading to a spectrum of neuropathological lesions.9 Furthermore, anti-Hu antibodies have been shown to indicate an underlying neoplasm in 88% of cases, most of which are SCLC10 and in more than 80% of the cases, unexplainable neurological manifestations accompanied by high circulating titers of anti-Hu antibodies precede the cancer diagnosisr.11
The prognosis of patients with extensive stage SCLC is dismal and the median progression-free survival is about 6 months.12 Similarly, the average life expectancy of patients with tonsillar metastases was reported to be less than 9 months, unrelated with the histology of the primary tumor.1,3 However, our patient was still alive, with no signs of disease progression 2 years after the diagnosis. It is interesting to note that patients with SCLC and positive anti-Hu antibodies generally have a better prognosis, especially for those who did not manifest an anti-Hu antibody-associated syndrome but harbored low titers of anti-Hu antibodies, as they tend to respond better to therapy and live longer than cancer patients not producing anti-Hu antibodies.13 In addition, extraordinary long-term survival of patients with SCLC accompanied by anti-Hu antibody-associated PSN has been reported.14
Accumulating evidences suggests that an anti-Hu antibody-triggered anticancer immune response may play an important role in tumor rejection and disease control,9,11 and immunotherapies based on this hypothesis are under development.15 The symptoms of PSN occurred 1 year prior to the diagnosis of SCLC in our patient and a high titer of anti-Hu antibodies persisted during the disease remission, suggesting an active role for the immune response in this case.
The symptoms of PSN still bothered our patient and it has been reported that anti-Hu antibody-associated paraneoplastic neuropathy can continue to progress even after tumor remission.14 The currently proposed immunosuppressive therapies such as plasma exchange, intravenous immunoglobulin G, and cyclophosphamide are generally unsatisfactory,4 and sometimes in SCLC patients with anti-Hu antibody-associated paraneoplastic neuropathy, the prognosis may depend on the outcome of the neurological disorders rather than on tumor progression.10 However, it is widely perceived that potent immunosuppressive modulation may favor tumor growth and disease flare. Consequently, novel treatment approaches are highly needed and an intensive investigation of the biology of Hu antigen-specific cytotoxic T-lymphocytes should be carried out.
Our study has limitations and we could not rule out a differential diagnosis. Although extremely rare, primary small cell carcinoma of the tonsil has been reported and it can metastasize to the lung.16 Without cutting-edge technologies such as transcriptome and proteomic analyses, it is quite difficult to discern the origin of the primary tumor site, in case of synchronous tumor masses. However, the treatment modalities for these 2 diagnoses are almost the same and the patient is doing well under current management.
CONCLUSIONS
Unilateral tonsillar metastasis of SCLC is rare, but it does occur. To the best of our knowledge, this is the first case of tonsillar metastatic SCLC accompanied by anti-Hu antibody-associated PSN. An anticancer immune response may have played an important role in the disease control.
Acknowledgment
The authors would like to thank the patient and his family for participating in this study. They would also like to thank The Young Investigator Award from Peking Union Medical College Hospital (grant number 33320140115, PI: NJ) for providing funding.
Footnotes
Abbreviations: CT = computed tomography, NSE = neuron-specific enolase, PET-CT = positron emission tomography-computed tomography, PSN = paraneoplastic sensory neuropathy, SCLC = small cell lung cancer.
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
WY designed this study. WY, NJ, and WL were principal physicians. LM was responsible for the diagnosis and management of the paraneoplastic neuropathy. YH was responsible for the treatment and interpretation of the tonsillar mass. NJ wrote the first version of the manuscript, and all authors read and approved the final version of the manuscript.
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Hisa Y, Yasuda N, Murakami M. Small cell carcinoma of the lung metastatic to the palatine tonsil. Otolaryngol Head Neck Surg 1997; 116:563–564. [DOI] [PubMed] [Google Scholar]
- 2.Unsal M, Kutlar G, Sullu Y, Yurtlu S, et al. Tonsillar metastasis of small cell lung carcinoma. Clin Respir J 2015; doi: 10.1111/crj.12275. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 3.Kim EJ, Kim SR, Jin Gang S, et al. Tonsillar metastasis of small cell lung cancer in a patient with idiopathic pulmonary fibrosis: a case report. Medicine (Baltimore) 2015; 94:e565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Koike H, Tanaka F, Sobue G. Paraneoplastic neuropathy: wide-ranging clinicopathological manifestations. Curr Opin Neurol 2011; 24:504–510. [DOI] [PubMed] [Google Scholar]
- 5.van Meerbeeck JP, Fennell DA, De Ruysscher DK. Small-cell lung cancer. Lancet 2011; 378:1741–1755. [DOI] [PubMed] [Google Scholar]
- 6.Seddon DJ. Tonsillar metastasis at presentation of small cell carcinoma of the lung. J R Soc Med 1989; 82:688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arroyo HH, Takehara J, Ogawa AI, et al. Small cell lung carcinoma metastasis to palatine tonsils. Braz J Otorhinolaryngol 2013; 79:645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen XH, Bao YY, Zhou SH, et al. Palatine tonsillar metastasis of small-cell neuroendocrine carcinoma from the lung detected by FDG-PET/CT after tonsillectomy: a case report. Iran J Radiol 2013; 10:148–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pignolet BS, Gebauer CM, Liblau RS. Immunopathogenesis of paraneoplastic neurological syndromes associated with anti-Hu antibodies: a beneficial antitumor immune response going awry. Oncoimmunology 2013; 2:e27384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Graus F, Keime-Guibert F, Reñe R, et al. Anti-Hu-associated paraneoplastic encephalomyelitis: analysis of 200 patients. Brain 2001; 124:1138–1148. [DOI] [PubMed] [Google Scholar]
- 11.Darnell RB, DeAngelis LM. Regression of small-cell lung carcinoma in patients with paraneoplastic neuronal antibodies. Lancet 1993; 341:21–22. [DOI] [PubMed] [Google Scholar]
- 12.Slotman BJ, van Tinteren H, Praag JO, et al. Use of thoracic radiotherapy for extensive stage small-cell lung cancer: a phase 3 randomised controlled trial. Lancet 2015; 385:36–42. [DOI] [PubMed] [Google Scholar]
- 13.Graus F, Dalmou J, Reñé R, et al. Anti-Hu antibodies in patients with small-cell lung cancer: association with complete response to therapy and improved survival. J Clin Oncol 1997; 15:2866–2872. [DOI] [PubMed] [Google Scholar]
- 14.Poepel A, Jarius S, Heukamp LC, et al. Neurological course of long-term surviving patients with SCLC and anti-Hu syndrome. J Neurol Sci 2007; 263:145–148. [DOI] [PubMed] [Google Scholar]
- 15.Ehrlich D, Wang B, Lu W, et al. Intratumoral anti-HuD immunotoxin therapy for small cell lung cancer and neuroblastoma. J Hematol Oncol 2014; 7:91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sehdev A, Zhao Y, Singh AK, et al. Primary small cell carcinoma of the tonsil: a case report and review of the literature. Case Rep Oncol 2012; 5:537–541. [DOI] [PMC free article] [PubMed] [Google Scholar]


