Abstract
Aim
To provide comprehensive real‐world evidence on societal diabetes‐attributable costs in Denmark.
Methods
National register data are linked on an individual level through unique central personal registration numbers in Denmark. All patients in the Danish National Diabetes Register in 2011 (N = 318 729) were included in this study. Complication status was defined according to data from the Danish National Hospital Register. Diabetes‐attributable costs were calculated as the difference between costs of patients with diabetes and the expected costs given the annual resource consumption of the diabetes‐free population.
Results
Societal costs attributable to diabetes were estimated to be at least 4.27 billion EUR in 2011, corresponding to 14,349 EUR per patient‐year. A twofold higher healthcare resource usage was found for patients with diabetes as compared with the diabetes‐free population. Attributable costs, grouped according to different components, were 732 million EUR for primary and secondary care services, 153 million EUR for pharmaceutical drugs, 851 million EUR for nursing services, 1.77 billion EUR in lost productivity and 761 million EUR for additional costs. A steep increase in diabetes‐attributable costs was found for patients with major complications compared with patients without complications across all cost components. For attributable healthcare costs this increase was estimated to be 6,992 EUR per person‐year after controlling for potential confounders.
Conclusions
Nearly half of the total costs of patients with diabetes can be attributed directly to their diabetes. The majority of costs are incurred among patients with major complications pointing to the importance of secondary preventive efforts among patients with diabetes.
What's new?
Real‐world evidence on the attributable costs of diabetes is calculated from individual register data and categorized according to complication progression.
The study shows evidence of twofold higher healthcare resource usage in patients with diabetes compared with the diabetes‐free population.
The societal diabetes‐attributable costs of diabetes in Denmark 2011 were estimated to be ˜ 4.27 billion EUR, corresponding to 14,349 EUR per patient year.
Nearly 60% of diabetes‐attributable costs were ascribed to the 25% of patients with major complications.
Steep gradients of increasing costs with increasing complications were evidenced across all cost components.
What's new?
Real‐world evidence on the attributable costs of diabetes is calculated from individual register data and categorized according to complication progression.
The study shows evidence of twofold higher healthcare resource usage in patients with diabetes compared with the diabetes‐free population.
The societal diabetes‐attributable costs of diabetes in Denmark 2011 were estimated to be ˜ 4.27 billion EUR, corresponding to 14,349 EUR per patient year.
Nearly 60% of diabetes‐attributable costs were ascribed to the 25% of patients with major complications.
Steep gradients of increasing costs with increasing complications were evidenced across all cost components.
Introduction
Globally, healthcare systems are facing the challenge of an exponential increase in the prevalence of chronic diseases 1. This puts a heavy economic burden on society as new successful but costly treatments lead to an increase in care for more people as life expectancy increases.
With ~ 371 million people diagnosed globally 2 and evidence of rapidly increasing prevalence 3, 4, 5, 6, diabetes mellitus is one of the most burdensome chronic diseases. Diabetes is associated with shorter lifetime, reduced quality of life and economic burdens on the patient and society as a result of healthcare, pharmaceutical drugs, nursing, reduced labour market participation and premature mortality 1, 7, 8, 9, 10.
We aimed to present new evidence of the relationship between costs of patients with diabetes, with and without complications, compared with the diabetes‐free population based on data from all relevant national registers in Denmark 11. Categorizing patients according to their complication progression into no complications, minor complications and major complications, is a novel method intended to inform decision‐makers of a complex problem in an intuitive and easily interpretable way. Our results provide an economic rationale for secondary prevention, which is important to recognize with increasing numbers of patients with the chronic condition of diabetes. Furthermore, the results may contribute to an awareness among decision‐makers regarding the allocation of budgets which can impede shifts of resources between sectors.
Subjects and methods
Study population
Denmark offers unique opportunities for register‐based research in epidemiology and healthcare 11. The present study is part of a large‐scale register‐based observational investigation, the Diabetes Impact Study 2013, investigating the epidemiological, health economic and socio‐economic aspects of diabetes in Denmark.
The study population was identified from the Danish National Diabetes Register, adjusted for shortcomings 12, resulting in a period prevalence of n = 318,729. Person‐time was quantified as number of person‐years, defined as 365 person‐days (n = 297,378). Patient data were combined with data from the Danish National Patient Register 13, the Danish National Prescription Registry 14, the Danish National Health Service Register 15, the Danish Civil Registration System 16 and registers at Statistics Denmark. Municipal statements were used where register data were not available. Data were linked between registers using the unique Danish Personal Identification Number, assigned to each Danish citizen 16.
Analysis
Person‐time was stratified by gender and current age (in 5‐year age intervals) into three complication status groups: no complications, minor complications and major complications. Documentation on diagnoses and procedural codes across complication status groups can be found in Table S1.
The cost of illness framework was applied with a societal cost perspective, including both direct and indirect costs, but excluding intangible costs such as psychosocial effects 10, 17. The analytical time window was the calendar year, 2011. Costs (market values excluding value added tax) 17) were defined as opportunity costs valued as alternative forgone use. The following cost components were evaluated on an individual person level from national register data: 1) healthcare services in primary and secondary care including ambulant treatment and emergency room visits; 2) nursing services in own home/assisted facilities and nurse home visits; 3) pharmaceutical drug consumption; and 4) lost productivity including lower annual income, absenteeism and premature mortality, calculated using the human capital approach 17. Additional cost components (prevention, education, psychological assistance, use of self‐monitoring of blood glucose appliances, insulin pumps, medical appliances, patients’ (and informal care givers’) own time and depreciation of capital) were conservatively estimated from Statistics Denmark data and the literature. The measurement of cost components is shown in Table S2.
Attributable costs measure the excess costs of patients with diabetes’ total healthcare consumption compared with the annual resource consumption of the diabetes‐free population, stratified according to gender and age. This approach means that our attributable cost estimates reflect the cost of care of patients with diabetes including issues not directly associated with diabetes, and not solely the cost of diabetes care. This was applied because earlier studies document that adding up diabetes‐specific diagnoses/services underestimates the attributable costs compared with a case–control method 18, 19.
For healthcare services, patients with diabetes were compared with the diabetes‐free population (n = 5,261,714 in 2011) stratified by gender and 5‐year age groups. For pharmaceutical drugs, nursing and the labour market, comparisons were made between patients with diabetes and a matched cohort of the diabetes‐free population, consisting of five control subjects per patient with diabetes, matched by age, gender and residence at date of diagnosis (n = 1,462,872). As a result of data limitations from source registers, some cost components were calculated per person (pharmaceutical drugs, nursing, productivity loss) and some per person‐years (healthcare costs). In calculations across the different sectors, person‐years were applied.
Direct associations between cost components and complication status groups were explored in a multivariate linear regression analysis, controlling for potential confounders (gender, age, highest attained education level, ethnicity, year of death and region of residence). The dependent variables were: total and attributable healthcare cost (EUR per person‐years) in primary and secondary care; total net pharmaceutical drug costs; and total costs for home nursing (EUR per year) in 2011, defined per group according to the independent variables. The definitions of these variables are given in Table S3. T‐tests were performed and the significance valued at the 1% level.
Costs were further analysed according to first ascertainment source in the Danish National Diabetes Register as we have previously seen that up to 20% of registrants in the Danish National Diabetes Register are included only as a result of frequent blood glucose measurements and may not have diabetes 12.
Results
Estimates for total and attributable costs and costs per person‐year across cost components, gender and complication status groups are shown in Tables 1, 2, 3. Estimates excluding possible ‘false‐positive’ patients are shown in Tables S4 and S5. All cost estimates are presented in Euro (EUR).
Table 1.
Total diabetes resource use (total costs) and costs per person‐year for the entire diabetes population according to complication status and gender
| Cost item | Total costs (EUR) | Total cost per person‐years (EUR) | ||||||
|---|---|---|---|---|---|---|---|---|
| ALL | C0 | C1 | C2 | ALL | C0 | C1 | C2 | |
| Healthcare costs | 1,638,237,935 | 553,933,413 | 319,439,149 | 764,865,373 | 5,509 | 3,361 | 5,508 | 10,257 |
| Women | 741,592,485 | 302,682,783 | 139,460,753 | 299,448,949 | 5,140 | 3,445 | 5,670 | 9,409 |
| Men | 896,645,450 | 251,250,630 | 179,978,396 | 465,416,424 | 5,857 | 3,265 | 5,388 | 10,889 |
| Primary care | 221,176,905 | 110,599,788 | 42,068,988 | 68,508,128 | 744 | 671 | 725 | 919 |
| Women | 113,618,643 | 63,234,638 | 19,779,391 | 30,604,615 | 787 | 720 | 804 | 962 |
| Men | 107,558,262 | 47,365,151 | 22,289,598 | 37,903,514 | 703 | 616 | 667 | 887 |
| Secondary care | 1,417,061,030 | 443,333,624 | 277,370,161 | 696,357,244 | 4,765 | 2,690 | 4,782 | 9,339 |
| Women | 627,973,841 | 239,448,145 | 119,681,362 | 268,844,335 | 4,352 | 2,725 | 4,866 | 8,447 |
| Men | 789,087,188 | 203,885,480 | 157,688,799 | 427,512,910 | 5,154 | 2,650 | 4,721 | 10,002 |
| Pharmaceutical drug costs | 255,799,680 | 102,638,292 | 62,354,493 | 90,806,895 | 860 | 623 | 1,075 | 1,218 |
| Women | 124,231,968 | 56,257,489 | 28,124,315 | 39,850,163 | 861 | 640 | 1,143 | 1,252 |
| Men | 131,567,712 | 46,380,803 | 34,230,178 | 50,956,732 | 859 | 603 | 1,025 | 1,192 |
| Nursing costs | 1,913,057,725 | 486,635,500 | 319,986,457 | 1,106,435,768 | 6,433 | 2,953 | 5,517 | 14,838 |
| Women | 1,181,279,919 | 347,648,931 | 197,983,759 | 635,647,229 | 8,187 | 3,957 | 8,050 | 19,973 |
| Men | 731,777,784 | 138,986,589 | 122,002,705 | 470,788,491 | 4,780 | 1,806 | 3,652 | 11,015 |
| Nursing home | 850,952,193 | 211,354,084 | 128,233,596 | 511,364,513 | 2,862 | 1,282 | 2,211 | 6,858 |
| Women | 537,556,556 | 151,368,523 | 82,046,366 | 304,141,667 | 3,726 | 1,723 | 3,336 | 9,556 |
| Men | 313,395,637 | 59,985,561 | 46,187,229 | 207,222,847 | 2,047 | 780 | 1,383 | 4,848 |
| Nursing in own home | 682,300,980 | 207,788,535 | 123,110,097 | 351,402,347 | 2,294 | 1,261 | 2,123 | 4,713 |
| Women | 421,328,648 | 149,028,783 | 75,136,381 | 197,163,484 | 2,920 | 1,696 | 3,055 | 6,195 |
| Men | 260,972,332 | 58,759,753 | 47,973,716 | 154,238,863 | 1,705 | 764 | 1,436 | 3,609 |
| Home nurse in own home | 379,804,552 | 67,492,881 | 68,642,764 | 243,668,907 | 1,277 | 410 | 1,183 | 3,268 |
| Women | 222,394,715 | 47,251,626 | 40,801,011 | 134,342,079 | 1,541 | 538 | 1,659 | 4,221 |
| Men | 157,409,815 | 20,241,275 | 27,841,759 | 109,326,781 | 1,028 | 263 | 833 | 2,558 |
| Productivity loss | 1,770,021,767 | 584,202,697 | 360,442,062 | 825,377,008 | 5,952 | 3,545 | 6,214 | 11,069 |
| Women | 550,569,259 | 245,373,990 | 101,862,861 | 203,332,408 | 3,816 | 2,793 | 4,142 | 6,389 |
| Men | 1,219,452,507 | 338,828,707 | 258,579,201 | 622,044,600 | 7,965 | 4,403 | 7,741 | 14,553 |
| Lost income | 912,272,022 | 413,992,645 | 184,680,345 | 313,599,033 | 3,068 | 2,512 | 3,184 | 4,206 |
| Women | 317,068,466 | 190,042,378 | 47,083,003 | 79,943,085 | 2,198 | 2,163 | 1,914 | 2,512 |
| Men | 595,203,557 | 223,950,267 | 137,597,342 | 233,655,947 | 3,888 | 2,910 | 4,119 | 5,467 |
| Lost productivity in 2011 as a result of premature mortality | 32,477,477 | 3,584,403 | 5,659,401 | 23,233,674 | 109 | 22 | 98 | 312 |
| Women | 8,209,904 | 884,182 | 1,901,945 | 5,423,777 | 57 | 10 | 77 | 170 |
| Men | 24,267,574 | 2,700,221 | 3,757,456 | 17,809,896 | 159 | 35 | 112 | 417 |
| Lost productivity in 2011 as a result of premature deaths before 2011 | 723,048,722 | 122,775,598 | 144,419,340 | 455,853,784 | 2,431 | 745 | 2,490 | 6,113 |
| Women | 187,784,170 | 35,195,124 | 44,329,134 | 108,259,911 | 1,302 | 401 | 1,802 | 3,402 |
| Men | 535,264,552 | 87,580,474 | 100,090,205 | 347,593,872 | 3,496 | 1,138 | 2,996 | 8,132 |
| Absence | 102,223,545 | 43,850,051 | 25,682,976 | 32,690,518 | 344 | 266 | 443 | 438 |
| Women | 37,506,720 | 19,252,307 | 8,548,779 | 9,705,634 | 260 | 219 | 348 | 305 |
| Men | 64,716,826 | 24,597,745 | 17,134,197 | 22,984,884 | 423 | 320 | 513 | 538 |
| Total additional costs | 1,096,979,996 | 285,846,918 | 193,084,112 | 618,048,966 | 3,689 | 1,734 | 3,329 | 8,288 |
| Women | 499,242,465 | 152,580,215 | 81,802,942 | 264,859,308 | 3,460 | 1,737 | 3,326 | 8,322 |
| Men | 597,737,531 | 133,266,704 | 111,281,170 | 353,189,657 | 3,904 | 1,732 | 3,331 | 8,263 |
| Education, prevention, psychological assistance etc. | 23,510,431 | 13,124,212 | 4,710,462 | 5,675,757 | 79 | 80 | 81 | 76 |
| Women | 11,433,432 | 7,005,481 | 1,995,657 | 2,432,294 | 79 | 80 | 81 | 76 |
| Men | 12,076,999 | 6,118,731 | 2,714,805 | 3,243,462 | 79 | 80 | 81 | 76 |
| SMBG and pumps | 66,392,321 | 38,767,809 | 13,283,599 | 14,340,912 | 223 | 235 | 229 | 192 |
| Women | 32,467,058 | 20,693,596 | 5,627,794 | 6,145,668 | 225 | 236 | 229 | 193 |
| Men | 33,925,263 | 18,074,213 | 7,655,806 | 8,195,243 | 222 | 235 | 229 | 192 |
| Medical appliances | 57,486,656 | 0 | 0 | 57,486,656 | 193 | 0 | 0 | 771 |
| Women | 24,635,388 | 0 | 0 | 24,635,388 | 171 | 0 | 0 | 774 |
| Men | 32,851,268 | 0 | 0 | 32,851,268 | 215 | 0 | 0 | 769 |
| Patients’ and informal care givers’ time | 345,542,010 | 183,886,084 | 66,482,029 | 95,173,897 | 1,162 | 1,116 | 1,146 | 1,276 |
| Women | 167,107,269 | 98,155,258 | 28,166,096 | 40,785,915 | 1,158 | 1,117 | 1,145 | 1,282 |
| Men | 178,434,741 | 85,730,825 | 38,315,933 | 54,387,982 | 1,166 | 1,114 | 1,147 | 1,272 |
| Depreciation | 604,048,579 | 50,068,814 | 108,608,022 | 445,371,743 | 2,031 | 304 | 1,873 | 5,973 |
| Women | 263,599,318 | 26,725,880 | 46,013,396 | 190,860,043 | 1,827 | 304 | 1,871 | ½5,997 |
| Men | 340,449,260 | 23,342,934 | 62,594,626 | 254,511,701 | 2,224 | 303 | 1,874 | 5,955 |
| Total for all cost items | 6,674,097,103 | 2,013,256,821 | 1,255,306,273 | 3,405,534,010 | 22,443 | 12,216 | 21,643 | 45,670 |
| Women | 3,096,916,097 | 1,104,543,408 | 549,234,630 | 1,443,138,059 | 21,465 | 12,572 | 22,331 | 45,345 |
| Men | 3,577,180,985 | 908,713,433 | 706,071,649 | 1,962,395,903 | 23,365 | 11,809 | 21,137 | 45,912 |
C0, no complications; C1, minor complications; C2, major complications; SMBG, self‐monitoring of blood glucose.
Table 2.
Diabetes attributable costs and attributable costs per person‐year for the diabetes population according to complication status and gender
| Cost item | Total attributable cost (EUR) | Total attributable cost per person‐year (EUR) | ||||||
|---|---|---|---|---|---|---|---|---|
| ALL | C0 | C1 | C2 | ALL | C0 | C1 | C2 | |
| Healthcare costs | 731,520,509 | 93,151,921 | 146,557,644 | 491,810,944 | 2,460 | 565 | 2,527 | 6,595 |
| Women | 307,076,026 | 56,324,754 | 65,757,805 | 184,993,467 | 2,128 | 641 | 2,674 | 5,813 |
| Men | 424,444,483 | 36,827,167 | 80,799,839 | 306,817,477 | 2,772 | 479 | 2,419 | 7,178 |
| Primary care | 23,775,938 | 8,071,606 | 4,630,869 | 11,073,463 | 80 | 49 | 80 | 149 |
| Women | 9,466,709 | 3,358,214 | 2,032,360 | 4,076,136 | 66 | 38 | 83 | 128 |
| Men | 14,309,229 | 4,713,392 | 2,598,509 | 6,997,327 | 93 | 61 | 78 | 164 |
| Secondary care | 707,744,571 | 85,080,316 | 141,926,775 | 480,737,481 | 2,380 | 516 | 2,447 | 6,447 |
| Women | 297,609,317 | 52,966,541 | 63,725,445 | 180,917,331 | 2,063 | 603 | 2,591 | 5,685 |
| Men | 410,135,255 | 32,113,775 | 78,201,329 | 299,820,150 | 2,679 | 417 | 2,341 | 7,015 |
| Pharmaceutical drug costs | 153,372,738 | 51,151,437 | 43,493,499 | 58,727,802 | 516 | 310 | 750 | 788 |
| Women | 68,729,716 | 25,830,792 | 18,958,706 | 23,940,218 | 476 | 294 | 771 | 752 |
| Men | 84,643,022 | 25,320,645 | 24,534,793 | 34,787,584 | 553 | 329 | 734 | 814 |
| Nursing costs | 851,426,972 | 44,157,419 | 138,412,494 | 668,857,059 | 2,863 | 268 | 2,386 | 8,970 |
| Women | 530,191,480 | 55,119,865 | 94,574,667 | 380,496,948 | 3,675 | 627 | 3,845 | 11,956 |
| Men | 321,235,491 | ‐10,962,446 | 43,837,827 | 288,360,111 | 2,098 | ‐142 | 1,312 | 6,746 |
| Nursing home | 271,179,210 | ‐22,733,872 | 29,375,665 | 264,537,417 | 912 | ‐138 | 506 | 3,548 |
| Women | 214,979,658 | 8,249,313 | 31,006,921 | 175,723,425 | 1,490 | 94 | 1,261 | 5,521 |
| Men | 56,199,552 | ‐30,983,185 | ‐1,631,255 | 88,813,992 | 367 | ‐403 | ‐49 | 2,078 |
| Nursing in own home | 307,899,167 | 47,914,035 | 59,025,923 | 200,959,210 | 1,035 | 291 | 1,018 | 2,695 |
| Women | 180,996,612 | 39,487,891 | 36,882,579 | 104,626,142 | 1,254 | 449 | 1,500 | 3,287 |
| Men | 126,902,555 | 8,426,144 | 22,143,344 | 96,333,067 | 829 | 110 | 663 | 2,254 |
| Home nurse in own home | 272,348,594 | 18,977,256 | 50,010,906 | 203,360,433 | 916 | 115 | 862 | 2,727 |
| Women | 134,215,210 | 7,382,661 | 26,685,167 | 100,147,381 | 930 | 84 | 1,085 | 3,147 |
| Men | 138,133,384 | 11,594,594 | 23,325,738 | 103,213,051 | 902 | 151 | 698 | 2,415 |
| Productivity loss | 1,770,021,767 | 584,202,697 | 360,442,062 | 825,377,008 | 5,952 | 3,545 | 6,214 | 11,069 |
| Women | 550,569,259 | 245,373,990 | 101,862,861 | 203,332,408 | 3,816 | 2,793 | 4,142 | 6,389 |
| Men | 1,219,452,507 | 338,828,707 | 258,579,201 | 622,044,600 | 7,965 | 4,403 | 7,741 | 14,553 |
| Lost income | 912,272,022 | 413,992,645 | 184,680,345 | 313,599,033 | 3,068 | 2,512 | 3,184 | 4,206 |
| Women | 317,068,466 | 190,042,378 | 47,083,003 | 79,943,085 | 2,198 | 2,163 | 1,914 | 2,512 |
| Men | 595,203,557 | 223,950,267 | 137,597,342 | 233,655,947 | 3,888 | 2,910 | 4,119 | 5,467 |
| Lost productivity in 2011 due to premature mortality | 32,477,477 | 3,584,403 | 5,659,401 | 23,233,674 | 109 | 22 | 98 | 312 |
| Women | 8,209,904 | 884,182 | 1,901,945 | 5,423,777 | 57 | 10 | 77 | 170 |
| Men | 24,267,574 | 2,700,221 | 3,757,456 | 17,809,896 | 159 | 35 | 112 | 417 |
| Lost productivity in 2011 due to premature deaths before 2011 | 723,048,722 | 122,775,598 | 144,419,340 | 455,853,784 | 2,431 | 745 | 2,490 | 6,113 |
| Women | 187,784,170 | 35,195,124 | 44,329,134 | 108,259,911 | 1,302 | 401 | 1,802 | 3,402 |
| Men | 535,264,552 | 87,580,474 | 100,090,205 | 347,593,872 | 3,496 | 1,138 | 2,996 | 8,132 |
| Absence | 102,223,545 | 43,850,051 | 25,682,976 | 32,690,518 | 344 | 266 | 443 | 438 |
| Women | 37,506,720 | 19,252,307 | 8,548,779 | 9,705,634 | 260 | 219 | 348 | 305 |
| Men | 64,716,826 | 24,597,745 | 17,134,197 | 22,984,884 | 423 | 320 | 513 | 538 |
| Total additional costs | 760,778,770 | 257,979,629 | 132,635,083 | 370,164,058 | 2,558 | 1,565 | 2,287 | 4,964 |
| Women | 352,528,414 | 137,705,130 | 56,192,816 | 158,630,468 | 2,443 | 1,567 | 2,285 | 4,984 |
| Men | 408,250,356 | 120,274,499 | 76,442,267 | 211,533,590 | 2,667 | 1,563 | 2,288 | 4,949 |
| Education, prevention, psychological assistance etc. | 23,510,431 | 13,124,212 | 4,710,462 | 5,675,757 | 79 | 80 | 81 | 76 |
| Women | 11,433,432 | 7,005,481 | 1,995,657 | 2,432,294 | 79 | 80 | 81 | 76 |
| Men | 12,076,999 | 6,118,731 | 2,714,805 | 3,243,462 | 79 | 80 | 81 | 76 |
| SMBG and pumps | 66,392,321 | 38,767,809 | 13,283,599 | 14,340,912 | 223 | 235 | 229 | 192 |
| Women | 32,467,058 | 20,693,596 | 5,627,794 | 6,145,668 | 225 | 236 | 229 | 193 |
| Men | 33,925,263 | 18,074,213 | 7,655,806 | 8,195,243 | 222 | 235 | 229 | 192 |
| Medical appliances | 57,486,656 | 0 | 0 | 57,486,656 | 193 | 0 | 0 | 771 |
| Women | 24,635,388 | 0 | 0 | 24,635,388 | 171 | 0 | 0 | 774 |
| Men | 32,851,268 | 0 | 0 | 32,851,268 | 215 | 0 | 0 | 769 |
| Patients’ and informal care givers’ time | 345,542,010 | 183,886,084 | 66,482,029 | 95,173,897 | 1,162 | 1,116 | 1,146 | 1,276 |
| Women | 167,107,269 | 98,155,258 | 28,166,096 | 40,785,915 | 1,158 | 1,117 | 1,145 | 1,282 |
| Men | 178,434,741 | 85,730,825 | 38,315,933 | 54,387,982 | 1,166 | 1,114 | 1,147 | 1,272 |
| Depreciation | 267,847,352 | 22,201,524 | 48,158,993 | 197,486,835 | 901 | 135 | 830 | 2,648 |
| Women | 116,885,267 | 11,850,795 | 20,403,270 | 84,631,202 | 810 | 135 | 830 | 2,659 |
| Men | 150,962,085 | 10,350,729 | 27,755,723 | 112,855,634 | 986 | 135 | 831 | 2,640 |
| Total for all cost items | 4,267,120,755 | 1,030,643,103 | 821,540,781 | 2,414,936,871 | 14,349 | 6,254 | 14,164 | 32,386 |
| Women | 1,809,094,895 | 520,354,532 | 337,346,855 | 951,393,509 | 12,539 | 5,923 | 13,716 | 29,894 |
| Men | 2,458,025,860 | 510,288,571 | 484,193,927 | 1,463,543,362 | 16,055 | 6,631 | 14,495 | 34,241 |
C0, no complications; C1, minor complications; C2, major complications; SMBG, self‐monitoring of blood glucose.
Table 3.
Total person‐years for the entire diabetes population according to complication status and gender
| Person years | All | No complications | Minor complications | Major complications |
|---|---|---|---|---|
| Total | 297,378 | 164,809 | 58,000 | 74,568 |
| Women | 144,281 | 87,860 | 24,595 | 31,826 |
| Men | 153,097 | 76,950 | 33,405 | 42,742 |
Healthcare
Total healthcare costs were estimated to be 1.64 billion Euro, corresponding to 5509 EUR per person‐year. On average, a patient with diabetes consumed approximately twice the healthcare resources compared with a diabetes‐free person (1.2, 1.8 and 2.8 times the healthcare resource use of a diabetes‐free person for patients with no, minor or major complications, respectively) with higher gradients found among younger patients as compared with the elderly, among male patients as compared with female patients, and for secondary care as compared with primary care. A patient going from no complications to minor or major complications incurred increased healthcare costs of 1782 and 7534 EUR per person‐year, respectively, even after controlling for potential confounders (Table S6).
The total attributable healthcare costs of diabetes were estimated to be 732 million EUR, divided between the no complication, minor complication and major complication groups as follows: 93, 147 and 492 million EUR, respectively. The greatest absolute cost burden was observed in the age group of 60–74 years, mainly because of the sheer volume of patients in these age groups.
Average attributable costs per person‐year for healthcare were 2460 EUR (2,128 EUR for women and 2,772 EUR for men). The costs for patients with minor complications were 4.5 times higher and for patients with major complications 12 times higher than for patients without complications. Patients with major complications, representing 25% of all patients, consumed almost 50% of total healthcare resources. Differences in attributable healthcare costs between a patient with no complications and a patient with minor or major complications of 1617 and 7388 EUR per person‐year, respectively, were found, after controlling for potential confounders (Table S7).
Observed patterns in healthcare resource consumption are shown in Fig. 1 and may be summarized as follows: 1) gradients between complication status groups were especially marked for secondary care, where the largest costs also lay; 2) men consumed more resources in all secondary care services than women, whereas the opposite was true for primary care; and 3) attributable cost per person‐year decreased with age, mainly as a result of the diabetes‐free population experiencing an increase in cost with age.
Figure 1.
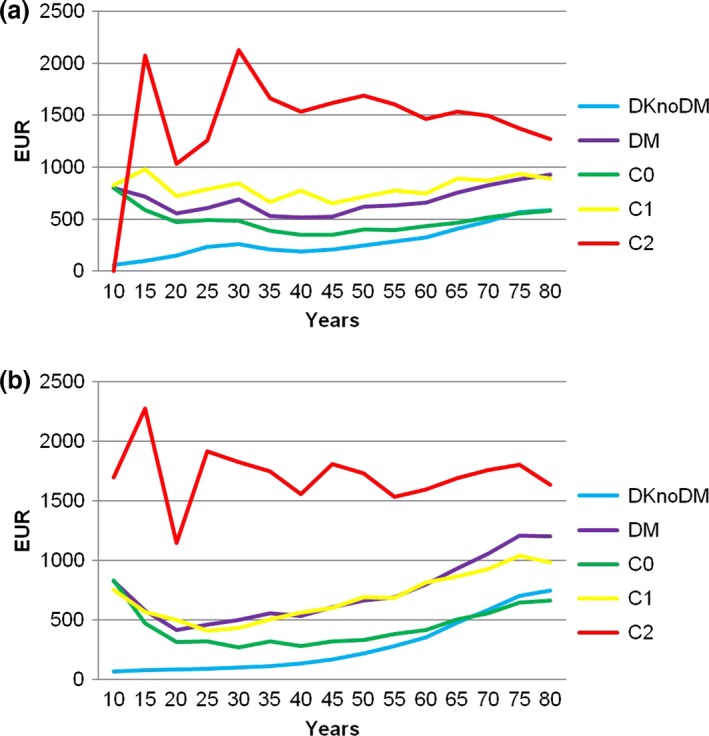
Total cost of secondary care for the diabetes‐free population (DKnoDM) and patients with diabetes (DM) by complication state (C0: no, C1: minor and C2: major) for (a) women and (b) men.
Pharmaceutical drugs
Pharmaceutical drug consumption amounted to 256 million EUR in 2011, corresponding to 860 EUR per person. Differences in the costs between no complications and minor and major complications, respectively, were 257 and 329 EUR per year, after controlling for potential confounders (Table S8). The pharmaceutical drug consumption of patients with diabetes was 2.5 times higher than that of the diabetes‐free population: 153 million Euro were found to be attributable to diabetes. Attributable costs per person‐year were 516 EUR (476 EUR for women and 553 EUR for men), and were 310, 750 and 788 EUR per person‐year for the no complication, minor complication and major complication groups, respectively. This shows a significant increase in pharmaceutical drug costs when patients progressed from uncomplicated diabetes to minor complications, whereas later progression to major complications did not impose a marked increase. For women, the increase from minor to major complications was 2% and for men 10%. The higher attributable costs among men were the result of differences in pharmaceutical drug consumption between genders in the control group, whereas consumption was approximately equal for each gender among patients with diabetes.
Attributable costs were highest among the young, and declined with age (Fig. 2). This pattern is mainly the result of patients with diabetes having more or less the same pharmaceutical drug consumption across age groups, whereas there was increasing consumption with age among the control subjects.
Figure 2.
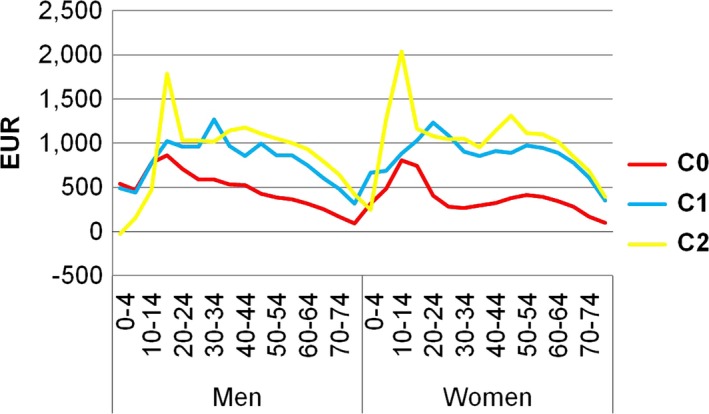
Diabetes‐attributable cost for pharmaceuticals by age, gender and complication status (C0: no, C1: minor and C2: major).
Nursing
Costs for nursing for patients with diabetes in 2011 amounted to 1.91 billion EUR, corresponding to 6,433 EUR per person. Total attributable nursing costs amounted to 851 million corresponding to 2,863 EUR per person‐year (3,675 EUR for women and 2,098 EUR for men). When the attributable costs were divided between the no complication, minor complication and major complication groups, the costs were 268, 2,386 and 8,970 EUR, respectively, per patient. Attributable costs per patient hence increased 33‐fold when patients progressed from uncomplicated diabetes to diabetes with major complications.
The probability of living in a nursing home for patients with diabetes was 45% greater compared with the matched diabetes‐free population. For men (in particular those aged ≥ 75 years) negative attributable costs were evidenced, reflecting that men in these older age groups, who have no complications, use fewer nursing resources than aged‐matched men in the diabetes‐free population. Patients with diabetes received on average 50% more home nursing visits than the matched diabetes‐free population. The difference in total costs for home nursing between patients with no complications and those with minor and major complications were estimated to be 299 and 722 EUR per year, respectively, after controlling for potential confounders (Table S9).
Productivity
In total, the productivity loss amounted to 1.77 billion EUR, assuming patients with diabetes of working age earned the same income as the diabetes‐free population of the same age, gender and education level, died at the same age and had not experienced any excess days of absence attributable to disease.
Patients with diabetes on average received a lower annual gross income than matched control subjects after controlling for education level. This reflected that a higher percentage of control subjects had jobs requiring high‐level skills, e.g. almost twice as many control subjects held jobs in managerial positions, whereas patients with diabetes had a 22% higher unemployment rate and more than twice as many had retired early (12% compared with 5.4%). Differences in income level increased with education level and complication status group, with a maximum annual difference among patients with major complications belonging to the highest education level group of 25,229 EUR for men and 24,104 EUR for women in the age group 55–59 years. The annual difference in mean gross income according to age in four education level groups is shown for the no complications group, with men and women separately in Fig. 3.
Figure 3.
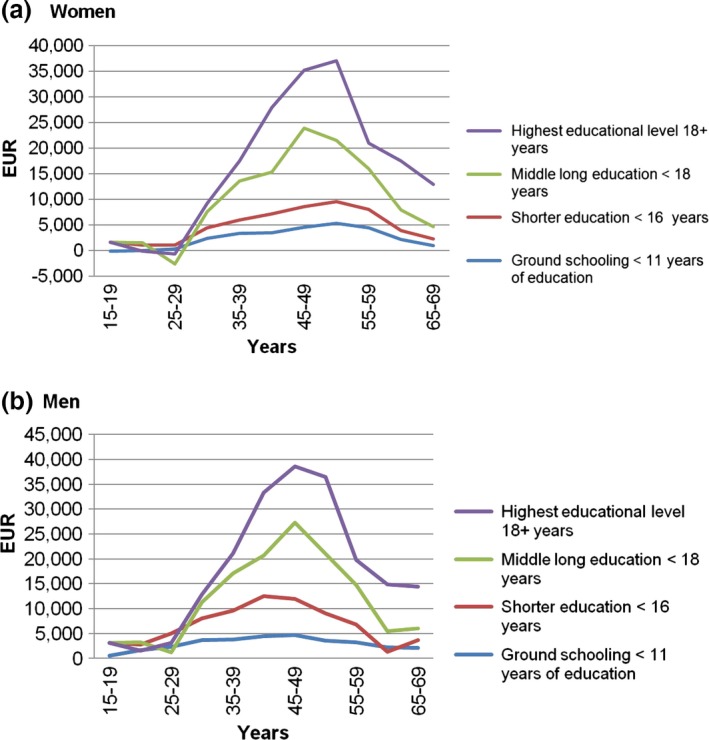
Annual difference in mean gross income according to age and education level for (a) women and (b) men with no diabetes complications.
The total attributable difference in annual gross income was 912 million EUR. The main share (46%) of the total productivity loss was attributable to productivity losses among patients with no complications, because of the volume of people of working age. Lost productivity in 2011 as a result of premature death from diabetes was 32.4 million EUR calculated from 1,567 premature deaths corresponding to 52% of the total number of deaths among patients with diabetes of working age and to 1% of the total diabetes population in the working age group. Production foregone in 2011 as a result of premature deaths from diabetes encountered before 2011 (with production foregone as a result of the diabetes‐attributable deaths until the age of 69 years used as proxy estimate) was estimated to be 723 million EUR, and excess days of absence from work were estimated to be 102 million EUR in 2011.
Additional costs
Additional costs attributable to diabetes were estimated to be 761 million EUR corresponding to 2,558 EUR per person‐year.
Total attributable costs
The total costs of diabetes in Denmark in 2011 were estimated to be 6.67 billion EUR (22,443 EUR per person‐year), of which 4.27 billion EUR (14,349 EUR per person‐year) were attributable to diabetes. The relative distribution between cost components is shown in Fig. 4, and the absolute distribution is shown in the Figure S1.
Figure 4.
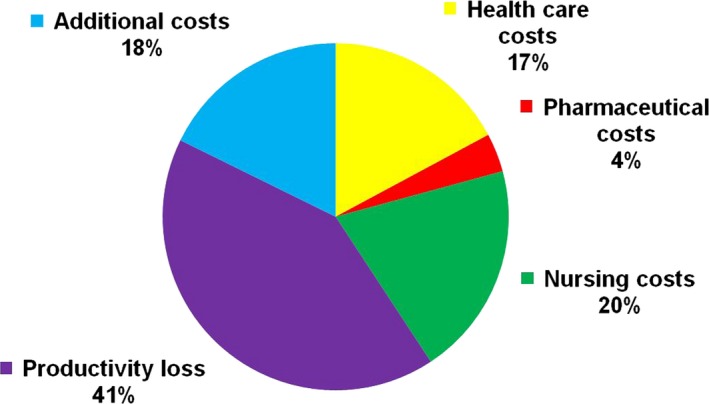
Relative distribution of the components of diabetes‐attributable costs.
The total diabetes‐attributable costs were divided between the no complication, minor complication and major complication groups as follows: 6,254, 14,164 and 32,386 EUR per person‐year, respectively (Fig. 5).
Figure 5.
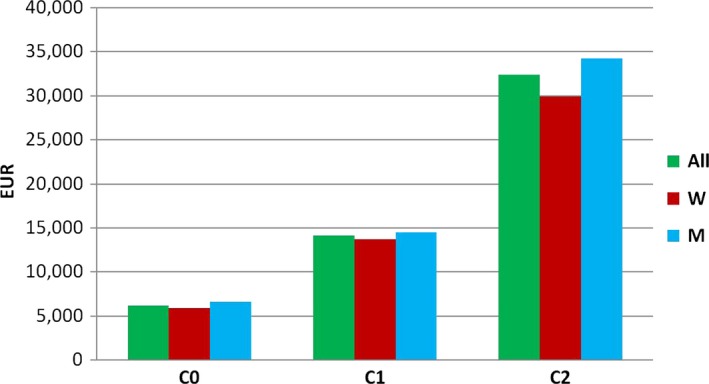
Diabetes attributable costs according to complication status (C0: no complications; C1: minor complications; C2: major complications) and gender.
The relative distribution of total attributable costs according to complication status and number of person‐years showed that 25% of patients with diabetes consumed nearly 60% of attributable costs (Fig. 6).
Figure 6.
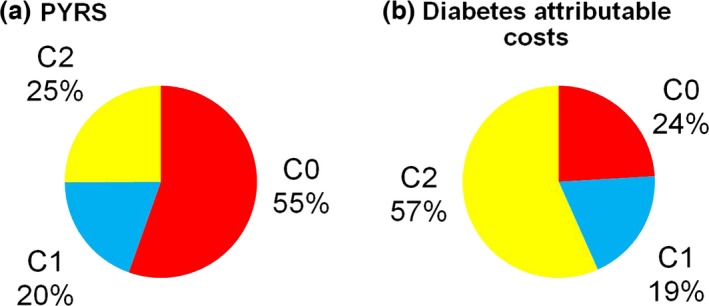
Relative distribution of person years (a) and diabetes attributable costs (b) according to complication status (C0: no complications; C1: minor complications; C2: major complications).
Discussion
We found that patients with diabetes consumed approximately twice the healthcare resources consumed by people without diabetes. This is less than that documented in earlier studies 20, indicating that the population with diabetes is becoming less resource‐demanding in the healthcare sector per person‐year, probably as a result of improvements in prognosis 21, 22. Compared with the diabetes‐free population, patients with diabetes incurred their resource use earlier in life, while later in life they required more specialized care. When patients with diabetes developed complications, the healthcare and nursing costs increased markedly. Men in particular used fewer healthcare services before complications, whereas later they were more likely than women to progress to major complications with a need for specialized care. We show a marked increase in healthcare costs with increasing complications, even after controlling for relevant confounders. These findings correspond to those of other studies, which document major costs related to diabetes complications 23, 24. This highlights the cost‐saving potential of preventing complications among patients with diabetes and hence the importance of secondary prevention. Acknowledging that more people are living for longer with diabetes because of prognosis improvements, and that these epidemiological trends cannot be turned around in the short or medium term 21, 22, the importance of prevention of expensive complications is highlighted. We found that patients’ morbidity characteristics were the most important predictors of diabetes‐attributable costs. Interestingly, however, the multivariate analysis, showed significant cost differences according to region of residence, education level and year of death. This latter finding indicates that the high attributable costs for younger patients with diabetes might, to some degree, be attributable to death per se, irrespective of the cause of death. This methodological issue should be further investigated. Likewise, underlying associations between patients’ characteristics and their morbidity patterns are important to investigate further in order to target prevention and treatment efforts. These issues will be dealt with in future work.
Regarding pharmaceutical drug consumption, the greatest increase in costs was found to be between patients with no complications and those with minor complications. Clinically, this might be explained by patients with minor complications being heavily medicated to prevent progression to major complications. Gender differences point to women being more proactive in receiving pharmaceutical drugs earlier in their diabetes (with fewer complications) than men. Nursing costs were found to be concentrated among patients with major complications, corresponding to recent structural changes in Denmark with respect to nursing services being offered. Patients with diabetes were more costly than the diabetes‐free population, in particular with respect to visits by a home nurse. Results clearly show evidence for different labour market patterns among patients with diabetes compared with the control subjects, and increasing loss in productivity among patients with diabetes was seen with an increase in complication levels. When controlling for education level, it was evident that the main extent of the income disparities could not be accounted for by the fact that the diabetes incidence was higher among people with lower income. We therefore expect the difference to be attributable to the influence of the ability of the person with diabetes to work, thus resulting in a lower annual income. Even though diabetes mainly affects older people in society, looking at patient volume, we show major costs to society as well as to the individual in relation to productivity.
The exclusion of patients registered in the Danish National Diabetes Register solely because of frequent blood glucose measurements (63,647 person‐years) 12 resulted in a reduction in patients with no complications. Total attributable costs were decreased by 9% (to 3.9 billion EUR), but attributable cost per person‐year increased. We conclude therefore that estimates for patients with no complications might be underestimated.
The chosen approach with a 1‐year time window has its limitations, but it allowed a descriptive analysis of the population in this year 25. It would be advantageous to include more years to facilitate analysis of trends over time. Our data did not allow a distinction between Type 1 and Type 2 diabetes, which would be advantageous taking the different aetiology into consideration. Our findings across age groups indicate high attributable costs among children and teenagers, reflecting that the diabetes‐free population in these age groups consumes markedly less healthcare, nursing services and pharmaceutical drugs.
Categorizing patients according to their development of complications; i.e. no complications, minor complications and major complications, is a novel method within this field. We aimed to contribute to this field with an easily understandable outline of the cost pattern for a very complex disease, providing decision‐makers with the necessary guidance for future investments in diabetes.
The presented cost distributions by component and by complication status are presumably not only valid in a Danish setting but could be transferred to other countries and chronic diseases.
Based on all available data in Danish national health registers for all patients with diabetes in 2011, the costs attributable to diabetes were estimated to be at least 4.27 billion EUR, corresponding to 14,349 EUR per person‐year. We show a steep increase in attributable costs for patients with major complications compared with patients without complications across all cost components, also when potential confounders are controlled for. Our results underline the universal message of cost increases with increased complications, providing an economic rationale for secondary prevention.
Evidence of cost distributions within diabetes can guide future efforts in specific sectors, or targeted patient groups, based on expected cost savings.
Funding sources
This study was conducted by the Institute of Applied Economics and Health Research in cooperation with the Danish Diabetes Association and supported by a PhD programme from Centre of Health Economics Research, funded by The Danish Centre for Strategic Research in Type 2 Diabetes, DD2. A consortium of sponsors, from the pharmaceutical industry comprising Astra Zeneca/BMS, Novo Nordisk, Merck, Sanofi Aventis and Bayer, provided an unrestricted grant to the Institute of Applied Economics and Health Research for the conduct of this research. Neither the Danish Diabetes Association nor the consortium of sponsors from the pharmaceutical industry had any influence on the execution of the study
Competing interests
None declared.
Supporting information
Table S1. Grouping of diagnoses and interventions used for classifying hospital activities by complication status of relevance for diabetes, and with respect to diagnostic specificity for diabetes.
Table S2. Cost units and methods of calculation for cost components.
Table S3. Definition of variables included in the multivariate analysis
Table S4. Total diabetes‐attributable costs and attributable costs per person‐year for all diabetes patients, excluding patients included in the National Diabetes Register as a result of frequent blood glucose measurements.
Table S5. Distribution of person‐years by complication status and gender for all diabetes patients, excluding patients included in the National Diabetes Register as a result of frequent blood glucose measurements.
Table S6. Multivariate analysis of total healthcare costs (EUR per person‐year).
Table S7. Multivariate analysis of total attributable healthcare costs (EUR per person‐year).
Table S8. Multivariate analysis of total net pharmaceutical costs (EUR per year).
Table S9. Multivariate analysis of total costs for nursing in own home (EUR per year).
Figure S1 Absolute distribution of diabetes‐attributable costs by cost components.
Supplementary references.
Acknowledgements
This study was conducted on behalf of the Danish Diabetes Association and supported by a PhD program at Centre of Health Economics Research supported by the Danish Centre for Strategic Research in Type 2 Diabetes, DD2. We thank Mrs Sabrina I. Imeroski for editorial assistance.
Diabet. Med. 33, 877–885 (2016)
[The copyright line for this article was changed on 15 February 2016 after original online publication.]
References
- 1. World Health Organisation . Global status report on noncommunicable diseases 2010. Description of the global burden of NCDs, their risk factors and determinants. Geneva: WHO, 2011. [Google Scholar]
- 2. International Diabetes Federation . IDF Diabetes Atlas Update 2012. IDF, 2012. [Google Scholar]
- 3. Jansson SPO, Andersson DKG, Svärdsudd K. Prevalence and incidence rate of diabetes melitus in a Swedish community during 30 years of follow‐up. Diabetologia 2007; 50: 703–710. [DOI] [PubMed] [Google Scholar]
- 4. Satman I, Omer B, Tutuncu Y, Kalaca S, Gedik S, Dinccag N et al Twelve‐year trends in the prevalence and risk factors of diabetes and prediabetes in Turkish adults. Eur J Epidemiol 2013; 28: 169–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Li R, Lu W, Jiang QW, Li YY, Zhao GM, Shi L et al Increasing prevalence of type 2 diabetes in Chinese adults in Shanghai. Diabetes Care 2012; 35: 1028–1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kengne AP, Echouffo‐Tcheugui JB, Sobngwi E, Mbanya JC. New insights on diabetes mellitus and obesity in Africa‐part 1: prevalence, pathogenesis and comorbidities. Heart 2013; 99: 979–983. [DOI] [PubMed] [Google Scholar]
- 7. World Health Organisation . Diabetes Fact sheet. Geneva: WHO, 2012. [Google Scholar]
- 8. OECD European Diabetes Leadership Forum . The diabetes epidemic and its impact on Europe, 2012. Available at http://www.oecd.org/els/health-systems/europeandiabetesleadershipforumedlfcopenhagen25-26april2012.htm Last accessed 2 October 2015.
- 9. American Diabetes Association . Economic Costs of Diabetes in the U.S. in 2012. Diabetes Care 2013; 36: 1033–1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ettaro L, Songer TJ, Zhang P, Engelgau MM. Cost of illness studies in Diabetes Mellitus. Pharmacoeconomics 2004; 22: 149–64. [DOI] [PubMed] [Google Scholar]
- 11. Thygesen LC, Daasnes C, Thaulow I, Hansen HB. Introduction to Danish (nationwide) registers on health and social issues: structure, access, legislation and archiving. Scand J Pub Health 2011; 39 (7 Suppl): 12–6. [DOI] [PubMed] [Google Scholar]
- 12. Green A, Sortsø C, Jensen PB, Emneus M. Validation of the Danish National Diabetes Register. J Clin Epidemiol 2015; 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lynge E, Sandegaard JL, Rebolj M. The Danish National Patient Register. Scand J Pub Health 2011; 39. [DOI] [PubMed] [Google Scholar]
- 14. Kildemoes H, Sørensen H, Hallas J. The Danish National Prescription Registry. Scand J Public Health 2011; 39: 38–41. [DOI] [PubMed] [Google Scholar]
- 15. Andersen JS, Olivarius NDF, Krasnik A. The Danish National Health Service Register. Scand J Public Health 2011; 39. [DOI] [PubMed] [Google Scholar]
- 16. Pedersen C. The Danish Civil Registration System. Scand J Public Health 2011; 39. [DOI] [PubMed] [Google Scholar]
- 17. Drummond M, Sculper M, Torrance G, O'Brien B, Stoddart G. Methods for the Economic Evaluation of Health Care Programme. New York: Oxford University Press, 2005. [Google Scholar]
- 18. Tunceli O, Wade R, Gu T, Bouchard JR, Aagren M, Luo W. Cost of diabetes: comparison of disease‐attributable and matched cohort cost estimation methods. Curr Med Res Opin 2010; 26: 1827–1834. [DOI] [PubMed] [Google Scholar]
- 19. Kristensen T, Olsen KR, Sortsø C, Ejersted C, Thomsen JL, Halling A. Resources allocation and health care needs in diabetescare in Danish GP clinics. Health Policy 2013; 113: 206–215. [DOI] [PubMed] [Google Scholar]
- 20. Rubin R, Altman W, Mendelson D. Health care expenditures for people with diabetes mellitus, 1992. J Clin Endocinol Metab 1994; 78: 809A–809F. [DOI] [PubMed] [Google Scholar]
- 21. Green A, Sortsø C, Jensen PB, Emneus M. The changing epidemiology of diabetes in Denmark: Results from the Diabetes Impact Study 2013 In: Group European Diabetes Epidemiology (EDE) , ed. 50th annual meeting of the European Diabetes Epidemiology Group Les Fontaines, Gouvieux‐Chantilly 2015. [Google Scholar]
- 22. Green A, Sortsø C, Jensen PB, Emneus M. The changing epidemiology of Renal Replacement Therapy in Diabetes. Results from the Diabetes Impact Study 2013, Denmark In: Niculescu E, ed. INTERDIAB ‐ International Conference on Interdisciplinary Management of Diabetes Mellitus and its Complications. Bucharest: Association for Renal Metabolic and Nutrition Studies, 2015. [Google Scholar]
- 23. Alva ML, Gray A, Mihaylova B, Leal J, Holman RR. The impact of diabetes‐related complications on healthcare costs: new results from the UKPDS (UKPDS 84). Diabet Med 2015; 32: 459–466. [DOI] [PubMed] [Google Scholar]
- 24. Massi‐Benedetti M. The cost of diabetes type II in Europe the Code‐2 study. Diabetologia 2002; 45: 1–4. [DOI] [PubMed] [Google Scholar]
- 25. Juul S. Epidemiologi og evidens. Copenhagen: Munksgaard Danmark, 2004. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Grouping of diagnoses and interventions used for classifying hospital activities by complication status of relevance for diabetes, and with respect to diagnostic specificity for diabetes.
Table S2. Cost units and methods of calculation for cost components.
Table S3. Definition of variables included in the multivariate analysis
Table S4. Total diabetes‐attributable costs and attributable costs per person‐year for all diabetes patients, excluding patients included in the National Diabetes Register as a result of frequent blood glucose measurements.
Table S5. Distribution of person‐years by complication status and gender for all diabetes patients, excluding patients included in the National Diabetes Register as a result of frequent blood glucose measurements.
Table S6. Multivariate analysis of total healthcare costs (EUR per person‐year).
Table S7. Multivariate analysis of total attributable healthcare costs (EUR per person‐year).
Table S8. Multivariate analysis of total net pharmaceutical costs (EUR per year).
Table S9. Multivariate analysis of total costs for nursing in own home (EUR per year).
Figure S1 Absolute distribution of diabetes‐attributable costs by cost components.
Supplementary references.


