Abstract
Sheikh Khalifa Medical City (SKMC) in Abu Dhabi is the main tertiary care referral hospital in the United Arab Emirates (UAE) with 560 bed capacity that is fully occupied most of the time.
SKMC senior management has made a commitment to make quality and patient safety a top priority. Our governing body Abu Dhabi Health Services Company has identified medication reconciliation as a critical patient safety measure and key performance indicator (KPI). The medication reconciliation electronic form a computerized decision support tool was introduced to improve medication reconciliation compliance on transition of care at admission, transfer and discharge of patients both in the inpatient and outpatient settings. In order to improve medication reconciliation compliance a multidisciplinary task force team was formed and led this quality improvement project. The purpose of this publication is to indicate the quality improvement interventions implemented to enhance compliance with admission medication reconciliation and the outcomes of those interventions.
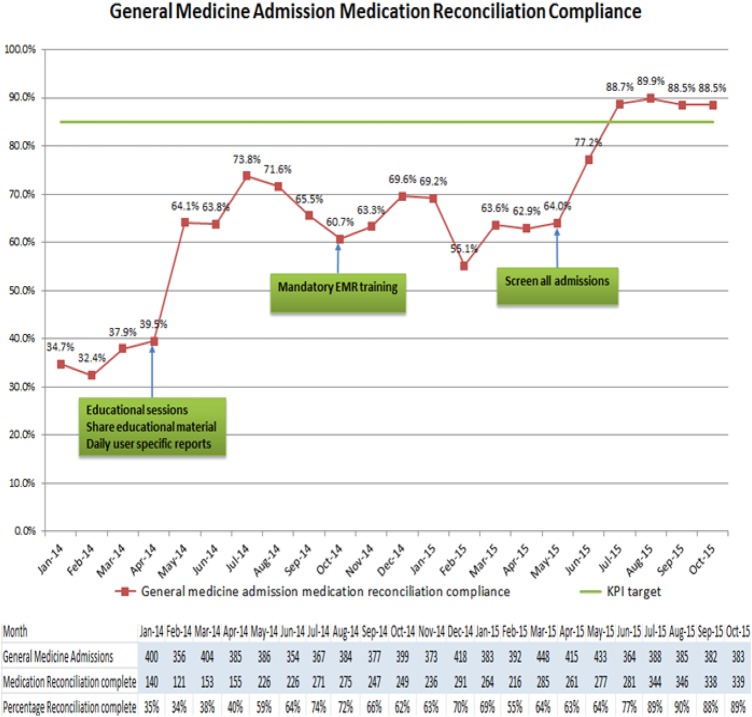
We chose to conduct the pilot study in general medicine as it is the busiest department in the hospital, with an average of 390 patients admitted per month during the study period. The study period was from April 2014 till October 2015 and a total of 8576 patients were evaluated. The lessons learned were disseminated throughout the hospital. Our aim was to improve admission medication reconciliation compliance using the electronic form in order to ensure patient safety and reduce preventable harm in terms of medication errors. Admission medication reconciliation compliance improved in general medicine from 40% to above 85%, and this improvement was sustained for the last four months of the study period.
Key interventions implemented:
Sharing daily user specific admission medication reconciliation compliance data with general medicine physicians
Conducting educational sessions to increase awareness and address concerns
Creating and communicating medication reconciliation education material
Incorporating medication reconciliation education in the mandatory electronic medical record (EMR) training for all newly hired physicians
Screening all general medicine admissions daily for admission medication reconciliation completion and providing timely feedback to the physicians to complete the reconciliation.
Problem
Sheikh Khalifa Medical City (SKMC) in Abu Dhabi is the main tertiary care referral hospital in the United Arab Emirates (UAE) with 560 bed capacity that is fully occupied most of the time. Medication reconciliation is a key safety measure and a major key performance indicator (KPI) identified by leadership and front line care givers as a high priority area. SKMC policy states that all admitted patients should receive medication reconciliation within 24 hours of admission. The electronic medication reconciliation form was introduced at SKMC in 2013 and monthly compliance data was shared with the respective departments.
However, the compliance was a challenge that required many performance improvement interventions to get front line staff engaged with completing the admission medication reconciliation. The overall baseline general medicine compliance was 40%. As a result, a multidisciplinary task force team was formed by senior management with representation from physicians, pharmacy, and the quality department. The focus of this team was to target physician ownership and accountability as a means to improve compliance.
Background
Medication errors are common since medications have to be procured, prescribed, dispensed, and administered. However, they occur most frequently during the prescribing and administering actions. The impact is significant and medication errors has been identified as a leading cause of patient harm and increased medical expenses in health care facilities worldwide.1–3
Medication reconciliation is the process of comparing a patient's medication orders to all of the medications that the patient has been taking. This reconciliation is done to avoid medication errors such as omissions, duplications, dosing errors, or drug interactions. It is a formal process of creating the most complete and accurate list possible of a patient's current medications and comparing the list against the admission, transfer, and discharge medication orders. Accurate and complete medication reconciliation can prevent numerous prescribing and administration errors. Feedback from pharmacy indicates that most prescribing errors are directly related to lack of proper medication reconciliation.
Medication reconciliation systems and processes have successfully reduced medication errors in many health care organizations.4–6 The electronic medication reconciliation tool is a standardized medication form used for documenting home medications and reconciling medications at transitions of care on admission, transfer, and discharge that provides an accurate medication list which is both accessible and visible. It is an important patient safety and quality measure, and it can have a major impact on improving medication reconciliation compliance and clinical outcomes by reducing prescribing medication errors.
Baseline measurement
Admission medication reconciliation compliance KPI target set by our governing body is above 85% based on international benchmarks. All general medicine admissions were on the second day of admission for completed admission medication reconciliation. Medication reconciliation compliance data was extracted by pharmacy from the electronic medical record monthly and shared with the general medicine team. The general medicine baseline performance compliance pre-implementation in April 2014 was 40%; admission medication reconciliation was performed in 155 out of 385 admitted patients (refer to attachment general medicine admission medication reconciliation compliance for monthly number of patients).
Design
Methodology used was prospective study of admission medication reconciliation in admitted medical patients by using a specific segmented electronic report that contained all required information including the medical service, time of admission, time of admission medication reconciliation completion, and responsible physician. The information was extracted from the electronic medication reconciliation screening tool.
The general medicine baseline performance compliance pre-implementation in April 2014 was low at 40%. We identified the problem and a multidisciplinary taskforce team was formed with representation from physicians, pharmacy and the quality department. Brain storming session was conducted; we came up with some ideas and tested those interventions through a series of plan, do, study, act (PDSA) cycles.
Strategy
Admission medication reconciliation improvement efforts were initiated across SKMC. We chose to conduct this pilot study in general medicine as it is the busiest department in the hospital. The key interventions tested and their impacts on improving the admission mediation reconciliation were as below.
PDSA cycle 1 (April 2014 till August 2014)
We started sharing daily user specific admission medication reconciliation compliance data with general medicine physicians using the division of general medicine email system. We conducted a number of educational sessions for general medicine physicians to increase awareness and address concerns and we also shared education material with the general medicine physicians on how to complete the medication reconciliation electronic form. This improved the compliance from 40% in April 2014 to 66% in September 2014.
PDSA cycle 2 (October 2014 till April 2015)
We incorporated medication reconciliation education in the mandatory electronic medical record training for all newly hired physicians. This resulted in improved compliance from 61% in October 2014 to 63% in April 2015.
PDSA cycle 3 (May 2015 till October 2015)
We started screening all general medicine admissions the following morning for admission medication reconciliation. Reminder emails were sent to the admitting physicians in a timely manner to complete the medication reconciliation within 24 hours from the time of admission. With this intervention we were able to achieve our KPI target of above 85% compliance in July 2015 and sustain this improvement for four consecutive months.
General medicine admission medication reconciliation
Results
With the implemented performance improvement interventions we were able to improve general medicine admission medication reconciliation from 40% in April 2014 to above 85% in July 2015, and we then sustained this improvement for four consecutive months (see attachment general medicine admission medication reconciliation compliance for monthly number of patients).
Lessons and limitations
Senior management support and empowerment was one of the critical success factors. However, it took time to get buy in and engagement from frontline staff due to different background education and training. In addition, we used education sessions to address the misconception that there was duplication of work. The role of information technology and automation in this process was critical.
The implementation of the electronic medication reconciliation tool had a significant impact on improving compliance. The lessons learned were disseminated throughout the hospital and the medication reconciliation improvement project will be implemented in other departments throughout the organization. The sustainability of this project will need to be enforced by engaging the front liners and maintaining leadership support.
Conclusion
The multidisciplinary taskforce team managed to implement quality improvement interventions and change management strategies that resulted in significant sustained improvement in admission medication reconciliation compliance for admitted general medicine patients. Admission medication reconciliation compliance improved from 40% to above 85% meeting the key performance indicator KPI target set by our governing body based on international benchmarks.
The lessons learned were disseminated throughout the organization. Implemented interventions are generalizable and can be replicated in other wards and organizations.
This improvement will enhance patient safety and reduce preventable harm in terms of medication errors. Support and commitment from senior leadership was critical to the success of this project.
This performance improvement project shows that quality improvement teams using information technology must understand the clinical context. They should engage the frontline staff in order to overcome resistance to change and implement sustainable systems.
Acknowledgments
Many thanks to SKMC pharmacy Rafik Youssif, Mazhar Abbasi and Mohammed Saifuddin for their significant contributions to this project. Thanks to all SKMC general medicine team members for their engagement and dedication. Special thanks to SKMC senior management for all their support and empowerment.
Footnotes
Declaration of interests: None of the authors have any declared conflict of interest.
Ethical approval: This was a performance improvement project hence it is exempt from ethical approval requirement.
References
- 1.The Joint Commission, National Patient Safety Goals Effective January 1, 2014 http://www.jointcommission.org/assets/1/6/HAP_NPSG_Chapter_2014.pdf Accessed: 15 September 2014 [Google Scholar]
- 2.Institute of Medicine (2006). Preventing Medication Errors: Quality Chasm Series. Washington, D.C.: National Academies Press. [Google Scholar]
- 3.Institute of Medicine (1999). To Err Is Human: Building a Safer Health System. Washington, DC: National Academy Press. [Google Scholar]
- 4.Institute for Healthcare Improvement (2014). Reconcile Medications at All Transition Points [Online] http://www.ihi.org/resources/Pages/Changes/ReconcileMedicationsatAllTransitionPoints.aspx Accessed: 15 September 2014 [Google Scholar]
- 5.Institute for Safe Medication Practices (2005). Building a case for medication reconciliation, ISMP Medication Safety Alert, Acute Care, [Online] https://www.ismp.org/newsletters/acutecare/articles/20050421.asp Accessed: 15 September 2014 [Google Scholar]
- 6.American Pharmacist Association, American Society of Health-System Pharmacists (2012). Improving Care Transitions: Optimizing Medication Reconciliation [Online] http://www.pharmacist.com/sites/default/files/files/2012_improving_care_transitions.pdf Accessed: 15 September 2014 [Google Scholar]