Abstract
Purpose: To evaluate the safety and ocular hypotensive efficacy of 4 trabodenoson doses administered twice daily over 14 or 28 days in subjects with ocular hypertension or primary open-angle glaucoma (POAG).
Methods: In this multicenter, randomized, double-masked, placebo-controlled, dose-escalation Phase 2 study, patients received unilateral topical twice-daily trabodenoson (50, 100, or 200 mcg) or placebo for 14 days, or 500 mcg trabodenoson or placebo for 28 days. Ocular and systemic safety and tolerability were assessed by examinations, clinical and laboratory studies. Intraocular pressure (IOP) was assessed using Goldmann tonometry.
Results: Trabodenoson was well tolerated; no clinically meaningful ocular or systemic side effects were identified. Trabodenoson produced a dose-dependent IOP reduction. IOP reductions in the 500 mcg group were significantly greater than placebo at all time points at Day 28. Mean IOP reductions from diurnal baseline ranged from −3.5 to −5.0 mmHg with a mean change of −4.1 mmHg in the 500 mcg group compared −1.0 to −2.5 mmHg with a mean change of −1.6 mmHg for the placebo group, and the Day 28 drop was significantly greater than at Day 14 (P = 0.0163) indicating improvement in IOP lowering with longer treatment time. IOP remained significantly reduced 24 h after the final 500 mcg dose (P = 0.048).
Conclusion: Twice-daily ocular doses of trabodenoson, from 50 to 500 mcg, were well tolerated and showed a dose-related decrease in IOP that was statistically significant and clinically relevant at 500 mcg in patients with ocular hypertension or POAG.
Keywords: : primary open angle glaucoma, ocular hypertension, intraocular pressure, Trabodenoson, adenosine, trabecular meshwork
Introduction
Primary open-angle glaucoma (POAG) is a multifactorial optic neuropathy for which the only established therapeutic intervention is the reduction of intraocular pressure (IOP). Ocular hypertension is a state in which IOP is elevated without evidence of glaucomatous optic neuropathy and is considered a risk factor for POAG. Lowering IOP in eyes with ocular hypertension can prevent the development of glaucoma,1,2 and IOP reduction can reduce the risk of disease progression in eyes with established glaucoma.3,4 In eyes with ocular hypertension or POAG, medical therapy to reduce IOP is the typical first-line treatment. Each year tens of thousands of patients undergo laser and incisional surgeries as a result of inadequate IOP control or disease progression. Thus, there is a clear medical need for new IOP-lowering medications with novel mechanisms that complement the currently available drugs or are effective in place of existing therapies.
Healthcare professionals and their patients have not benefited from a new drug with a novel mechanism of action since the development of latanoprost, a prostaglandin analog targeting the F2α receptor, which was approved for use in the United States in 1996. Like other drugs in the prostaglandin analog class, latanoprost lowers IOP predominantly by increasing the uveoscleral outflow of aqueous humor, the pathway responsible for a minority of aqueous outflow. The most common side effect of prostaglandin analogs is conjunctival hyperemia, which can lead to discontinuation and an increase in associated healthcare costs.5 Other side effects with this class include lash thickening and lengthening, periorbital fat atrophy, lid and iris hyperpigmentation, cystoid macular edema, and anterior chamber inflammation.6,7
Endogenous adenosine plays a role in many human physiologic processes through interactions with 4 known adenosine receptor subtypes (A1, A2A, A2B, and A3). Drugs with mechanisms of action related to the adenosine system (agonists and/or antagonists of the various receptor subtypes) are currently indicated for a variety of health conditions including supraventricular tachyarrhythmias, asthma, and pain management.
Adenosine and its receptors also play a complex role in modulating IOP.8,9 Selective A1 receptor agonism has been demonstrated to lower IOP in animal models10–14 while agonism of non-A1 receptors can elevate IOP.9,11 The lowering of IOP is due to increasing conventional outflow15 by increasing the secretion of matrix metalloproteinase-2 (MMP-2), which digests hydrolyzed collagen type IV, a major component of extracellular matrix (ECM) in the trabecular meshwork (TM).16,17 Levels of MMP-2 increase in response to mechanical stretch secondary to increased pressure in perfused human anterior segment organ cultures.18 This protease production shifts the balance between the deposition of ECM by TM cells, and its metabolism by MMP-2, which digests and removes protein from the outflow path, lowering outflow resistance and IOP, a mechanism contributing to IOP control.19 In humans, adenosine concentrations are elevated in aqueous humor of ocular hypertensive, but not normotensive patients, further supporting a potential role of adenosine in IOP homeostasis.20
Trabodenoson is a highly selective adenosine mimetic targeting the A1 receptor with the potential to lower IOP via a novel mechanism of action: by increasing outflow facility at the TM, which increases the outflow of aqueous humor via the conventional pathway.
Elsewhere in this issue of the Journal, the results of a Phase I safety and tolerability study of trabodenoson in healthy volunteers are reported. In this study, trabodenoson was found to be safe and well-tolerated with no dose-limiting toxicities at doses up to 3,200 mcg per eye. Significantly, it was not associated with adverse events (AEs) of conjunctival hyperemia or anterior chamber inflammation.
In this article we present the results of a Phase I/II clinical trial, the purpose of which was to assess trabodenoson's safety, tolerability, and IOP-lowering efficacy in subjects with ocular hypertension or POAG.
Methods
This was a randomized, double-masked, placebo-controlled, dose-escalation study designed to characterize the systemic and ocular safety and tolerability, IOP-lowering efficacy, and pharmacokinetic (PK) profile of trabodenoson delivered via topical ophthalmic dosing in subjects with ocular hypertension or POAG. The study was registered (ClinicalTrials.gov identifier: NCT01123785), and was conducted in accordance with Good Clinical Practices and the Declaration of Helsinki. The study was conducted at 18 sites throughout the United States, the protocol was approved by a central Institutional Review Board (IRB) or each site's IRB, and all subjects provided written informed consent.
Subjects
The study was conducted in 2 parts comprising 3 stages, with Part 1 consisting of Stages 1 and 2 and Part 2 consisting of Stage 3. Eligibility criteria were identical for all 3 stages. Subjects were 18–77 years old, had the clinical diagnosis of ocular hypertension or POAG, and met all of the following criteria in at least 1 eye during a 4-day pretreatment placebo run-in period (study days −4 to −1): mean IOP on Day −4 of ≥23 and ≤34 mmHg; mean IOP on Day −1 and Day 1 (before randomization or administration of study medication) of ≥24 and ≤34 mmHg; and mean IOP ≥21 mmHg on Day −1 at either 8 or 12 h after morning dosing of placebo. Key exclusion criteria included best-corrected visual acuity worse than 20/60 in either eye; advanced glaucoma (based on visual field and/or optic disc assessment); narrow or closed anterior chamber angles; recent use of topical IOP-lowering medications (miotics or carbonic anhydrase inhibitors within 4 days of Day −1; adrenergic agonists within 14 days of Day −1; beta-blockers within 28 days of Day −1; or prostaglandin analogs within 42 days of Day −1); history of central retinal vein occlusion, uveitis, ocular surgery, or trauma; pregnancy; significant systemic disease (including renal disease, cardiac disease excluding controlled systemic hypertension, asthma, or chronic obstructive pulmonary disease); current or recent use of certain medications (calcium channel blockers, beta-blockers, sympathomimetics, oral carbonic anhydrase inhibitors, dipyridamole, or other adenosine antagonists) or any experimental agents.
Schedule of visits
The study schedule was similar for all 3 stages and included a screening visit, a pretreatment baseline assessment period (ranging from 4 to 56 days during which washout of any currently used topical IOP-lowering medications took place, followed by a placebo run-in period), a 14-day (Stages 1 and 2) or 28-day (Stage 3) treatment period, and a 7-day postdose observation period.
Enrollment, randomization, and treatment
All subjects attended a screening visit during which eligibility was evaluated via a comprehensive review of medical history, complete ophthalmological examination, and systemic and ophthalmologic assessments. In Stage 1, subjects were randomized in a 1:1:1 ratio to receive either trabodenoson 50 or 100 mcg or placebo. In Stage 2, subjects were randomized in a 2:1 ratio to receive either trabodenoson 200 mcg or placebo. In Stage 3, subjects were randomized in a 1:1 ratio to receive either trabodenoson 500 mcg or placebo. Prespecified stopping rules—incorporating clinical, laboratory, and cardiac data—governed the continuation of the study from one stage to the next. In all 3 stages, dosing was applied twice daily in 1 or 2 drops delivered from a multidose bottle to 1 designated study eye only, which was the eye with the higher mean IOP across Day −4, Day −1, and Day 1 predose (or the right eye if pressures were equal). Doses in the active groups were 50 or 100 mcg in Stage 1, 200 mcg in Stage 2, and 500 mcg in Stage 3 and placebo in all stages was a vehicle-matched control. On study days, drug was dosed by study personnel; on nonstudy days, drug was dosed by the subject or a caregiver following observation and approval of the subject/caregiver's dosing technique.
Assessments
The safety and tolerability of trabodenoson were assessed on the basis of clinical evaluations conducted during the pretreatment baseline period and at selected time points during the treatment period, and continuous AE monitoring. AEs were categorized by System Organ Class (SOC) and Preferred Terms using the Medical Dictionary for Regulatory Activities (MedDRA, version 13). All AEs were graded by severity (mild, moderate, or severe) and likely causal relationship to the study drug (possibly, probably, or definitely related).
Systemic safety assessments at baseline, Days 1, 7, and 15 in part 1 and Days 1, 14, and 29 in part 2 included physical examinations, vital signs, and clinical laboratory tests including complete blood counts and blood chemistry assessments along with renal, hepatic, and cardiac biomarkers. Specific cardiovascular safety assessments included 12-lead electrocardiograms and troponin levels.
Ocular safety assessments included best corrected visual acuity (BCVA), IOP, and examination of the external eye (periorbital area, eyelids, eyelashes, conjunctiva, sclera, and pupils), slit lamp examination (eyelids, eyelashes, conjunctiva, cornea, sclera, pupils, iris, and lens) and dilated (and undilated at some time points) fundoscopic examination. BCVA was assessed using the Early Treatment Diabetic Retinopathy Study (ETDRS) protocol. Hyperemia was assessed before randomization and at various time points after dosing using a visual hyperemia scale (0—none/trace, 1—mild, 2—moderate and 3—severe).
IOP was measured at multiple time points throughout the study using Goldmann tonometry in a masked fashion and a 2-person operator/observer technique. IOP values are the mean of 2 readings at each time point; when 2 readings differed by more than 2 mmHg, a third reading was recorded and the 2 closest readings were used to determine the mean IOP at that time point.
PK calculations included area under the concentration–time curve (AUC), maximum concentration (Cmax), time to Cmax (tmax), and plasma half-life (t½). Blood samples were collected at multiple time points for these evaluations.
Statistical Methods
The primary objective of this study was to evaluate the tolerability and safety of topical monocular application of twice-daily trabodenoson 50–500 mcg in subjects with ocular hypertension or POAG. Secondary objectives included evaluation of trabodenoson IOP-lowering efficacy and PK analysis.
The primary efficacy endpoint was mean IOP (mean IOP measured throughout the day at 8 AM, 10 AM, 12 PM, 4 PM, and 8 PM). The mean IOPs of the active doses were statistically compared to those of the placebo group. In addition, analyses adjusting for baseline IOPs were performed. The parameters evaluated included IOP changes at each time of day from the corresponding diurnal baseline (IOP Change), change in daily IOP from diurnal baseline (Daily IOP Change); and the change in IOP from study baseline (Study Baseline IOP Change).
The IOP Change from diurnal baseline was defined as the mean of the differences between each individual time point (e.g., 8 AM, 10 AM, 12 PM, 4 PM, and 8 PM) on Days 7, 14, 28, or 29, and the corresponding IOPs on Day −1 (before randomization). The Daily IOP Change from diurnal baseline for each of the dose groups was the average of these 5 individual IOP changes from diurnal baseline on Days 7, 14, and 28. These 2 diurnal changes in IOP (IOP Change and Daily IOP Change) for each dose group (50, 100, 200, and 500 mcg) were compared statistically to the same changes in the placebo group. As stated above, a further efficacy analysis for Study Baseline IOP Change was conducted; this analysis calculated the reduction in IOP from the patients' 8 AM study baseline IOP (recorded at the 8 AM time point on Day 1 before active drug was administered).
The sample size was determined based on IOP-lowering efficacy outcomes for the primary efficacy endpoint—mean IOP. A sample size of 16 subjects per group in Stages 1 and 2 provides 80% power to detect a difference of 3.6 mmHg in mean IOP between groups using a 2-sided t-test and assuming a 3.5 mmHg standard deviation and a 2-sided alpha of 0.05. Likewise, in Stage 3, a sample size of 27 subjects per group provides 80% power to detect a 2.8 mmHg difference with a standard deviation of 3.5 mmHg between groups using the same approach and assumptions. The calculated sample size was increased by ∼10% to ensure 126 evaluable subjects complete the study.
Statistical analyses were conducted on the intent-to-treat population (defined as subjects randomized who received at least 1 dose of study medication). Nonparametric methodology based on rank statistics using analysis of covariance (ANCOVA) with baseline as a covariate was performed, as the assumption of the parametric ANCOVA did not hold. SAS PROC RANK was used to generate the ranks of the response and covariate variables without regard to treatment group. These ranks were then used in the ANCOVA model to compare the treatment groups. The Kruskal–Wallis test (nonparametric analysis) with preplanned contrasts (placebo versus each active dose) was applied to evaluate the dose-related effect of trabodenoson for all comparisons including IOP and the baseline adjusted data (IOP Change and Daily IOP Change). Presentations of the data include the mean IOP and the medians for baseline adjusted parameters (i.e., IOP Change, Daily IOP Change, and Study Baseline IOP Change).
Because the efficacy endpoints were considered secondary, no corrections for multiplicity were prespecified. However, due to multiple treatment comparisons, the alpha levels for the primary efficacy analysis (mean IOP) were adjusted using the Bonferroni correction to control the overall type I error at 5%. No adjustments were made for other comparisons.
The pooled placebo control group used for comparison of the Part 1 (stages 1 and 2) IOPs included data from all placebo-treated subjects through Day 14. A second contemporaneous placebo control group included only data from placebo-treated subjects treated for 28 days in Part 2 (stage 3), and was only used for comparison of the 28-day Part 2 IOP data. Unless otherwise stated, the analyses discussed include data from all placebo-treated subjects.
Results
Demographics and disposition
Overall, at 18 sites in the United States, 239 subjects were screened in this study, with 144 successfully completing the washout period and meeting all criteria for randomization. Demographic and baseline characteristics were generally similar across the different treatment groups, with the exception of a lower proportion of females in the trabodenoson 200 mcg group (29.4%) compared to all other groups (61.2%–70.6%). Observed differences were not considered to be clinically relevant (Table 1).
Table 1.
Demographic and Baseline Characteristics (ITT Population)
| Placebo | Trabodenoson | ||||
|---|---|---|---|---|---|
| Demographics | Pooled (n = 59) | 50 mcg (n = 17) | 100 mcg (n = 17) | 200 mcg (n = 17) | 500 mcg (n = 34) |
| Mean Age (SD), years | 59.0 (9.2) | 56.6 (12.2) | 55.6 (10.8) | 53.8 (10.1) | 57.6 (10.7) |
| Female (%) | 69.5 | 70.6 | 70.6 | 29.4 | 67.6 |
| Race (%) | |||||
| White | 71.2 | 76.5 | 76.5 | 82.4 | 64.7 |
| Black or African American | 25.4 | 23.5 | 23.5 | 11.8 | 35.3 |
| Other | 3.4 | — | — | 5.9 | |
| Primary ophthalmic diagnosis (%) | |||||
| OHT | 37.3 | 35.3 | 47.1 | 35.3 | 41.2 |
| POAG | 62.7 | 62.7 | 52.9 | 64.7 | 58.8 |
| Mean baseline IOP, mmHg (SD) | |||||
| All subjects | 26.6 (2.6) | 26.1 (2.6) | 25.6 (1.3) | 26.1 (2.8) | 26.2 (2.4) |
| Subjects with OHT | 26.7 (2.8) | 27.2 (3.0) | 25.0 (1.1) | 27.1 (3.6) | 26.3 (2.7) |
| Subjects with POAG | 26.5 (2.5) | 25.5 (2.3) | 26.1 (1.4) | 25.5 (2.3) | 26.1 (2.2) |
IOP, intraocular pressure; OHT, ocular hypertension; POAG, primary open-angle glaucoma; SD, standard deviation; ITT, intent-to-treat.
All 144 randomized subjects received at least 1 dose of study medication and were included in the safety and intent-to-treat analyses. Three subjects (2 treated with trabodenoson and 1 with placebo) were found to have exclusionary ECG findings from baseline evaluations (pretreatment) and were exited after receiving 1–5 doses of study medication. The remaining 141 subjects completed the study.
Safety results
All adverse events
The overall frequency of AEs is given in Table 2. Overall, the proportion of subjects with any AE was higher in the pooled placebo groups (30.5%, 18/59 subjects) than in the pooled trabodenoson groups (25.9%, 22/85 subjects). The only systemic treatment-emergent AEs occurring in 2 or more subjects in either the pooled placebo or trabodenoson groups were urinary tract infection in 3 placebo-treated subjects and oropharyngeal pain in 2 trabodenoson-treated subjects (one each in the 100 and 200 mcg groups). There were no serious AEs, no AE was judged to be severe, and no AE led to treatment discontinuation.
Table 2.
Overall Summary of Adverse Events, n (%)
| Placebo | Trabodenoson | |||||
|---|---|---|---|---|---|---|
| Pooled (n = 59) | 50 mcg (n = 17) | 100 mcg (n = 17) | 200 mcg (n = 17) | 500 mcg (n = 34) | Pooled (n = 85) | |
| Any AE | 18 (30.5) | 2 (11.8) | 4 (23.5) | 8 (47.1) | 8 (23.5) | 22 (25.9) |
| Related AE | 6 (10.2) | 1 (5.9) | 2 (11.8) | 4 (23.5) | 6 (17.6) | 13 (15.3) |
| Serious AE | 0 | 0 | 0 | 0 | 0 | 0 |
| AE resulting in discontinuation | 0 | 0 | 0 | 0 | 0 | 0 |
AE, adverse event.
Treatment-related adverse events
Treatment-related AEs are given in Table 3. The proportion of subjects in the pooled placebo and trabodenoson groups experiencing treatment-related AEs was similar (10.2% vs. 15.3%, respectively). The majority of these were ocular AEs, including conjunctival and ocular hyperemia in the trabodenoson groups (combined 16/85, 18.8%), eye irritation and foreign body sensation in the placebo groups (combined 5/59, 8.5%), and eyelid pruritus (1 case in each group). Of these 16 subjects with hyperemia, 10 were mild and 6 were moderate. Only 2 systemic AEs were judged to be treatment-related: 1 case each of skin pruritus and headache, both in the placebo group. All treatment-related AEs were graded as mild or moderate and none as severe.
Table 3.
Treatment-Related Adverse Events, n (%)
| Placebo | Trabodenoson | |||||
|---|---|---|---|---|---|---|
| Pooled (n = 59) | 50 mcg (n = 17) | 100 mcg (n = 17) | 200 mcg (n = 17) | 500 mcg (n = 34) | Pooled (n = 85) | |
| Eye disorders | ||||||
| Conjunctival hyperemia | 0 | 1 (5.9) | 1 (5.9) | 4 (23.5) | 6 (17.6) | 12 (14.1) |
| Ocular hyperemia | 0 | 0 | 2 (11.8) | 2 (11.8) | 0 | 4 (4.7) |
| Eyelid pruritis | 1 (1.7) | 0 | 0 | 1 (5.9) | 0 | 1 (1.2) |
| Eye irritation | 3 (5.1) | 0 | 0 | 0 | 0 | 0 |
| Foreign body sensation | 2 (3.4) | 0 | 0 | 0 | 0 | 0 |
| Skin and subcutaneous tissue disorders | ||||||
| Pruritus | 1 (1.7) | 0 | 0 | 0 | 0 | 0 |
| Nervous system disorders | ||||||
| Headache | 1 (1.7) | 0 | 0 | 0 | 0 | 0 |
Other safety evaluations
No clinically significant treatment-related abnormalities were observed in clinical laboratory studies, physical examinations, or cardiac function tests in any treatment group. The only ocular safety evaluation of note was the hyperemia assessment that accompanied the periodic ocular exams, using a visual scale. Hyperemia was assessed several times before, and after randomization, and the hyperemia rates by treatment are presented in Table 4. Hyperemia was assessed as mild in all subjects with the exception of 3 subjects in the 200 mcg group where moderate hyperemia was observed. As shown in Table 4, the incidence of hyperemia in every treatment group was similar before, and after, randomization, indicating that trabodenoson treatment did not add to the underlying hyperemia—measured before trabodenoson was administered—at any of the doses tested. High variability was observed in the incoming hyperemia rates across treatment groups to which subjects were ultimately randomized. Of note, the 500 mcg group had the highest incidence of hyperemia both before, and after randomization, a finding consistent with the spontaneous AE reports of hyperemia in this group.
Table 4.
Summary of Incidence of Hyperemia by Treatment Group and Time point—All Stages (%)
| Screening | Day −4 | Day −1 | Day 1-predose | Day 1-postdose | Day 14 | Day 28 | |
|---|---|---|---|---|---|---|---|
| Placebo | 8.5 | 3.4 | 1.7 | 3.4 | 0.6 | 3.5 | 3.8 |
| 50 mcg | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| 100 mcg | 5.9 | 5.9 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| 200 mcg | 0.0 | 0.0 | 0.0 | 0.0 | 2.0 | 1.0 | 0.0 |
| 500 mcg | 14.7 | 11.8 | 12.5 | 11.8 | n/a | 12.7 | 12.1 |
Efficacy results
Baseline IOP after washout ranged from 25.6 to 26.6 mmHg across treatment groups. Trabodenoson demonstrated a dose-dependent reduction in IOP. In the intent-to-treat (ITT) population, trabodenoson dose-related decreases in IOP in the study eye were observed, with statistically significant reductions observed at some time points at the 200 mcg dose, and at all time points at the 500 mcg dose.
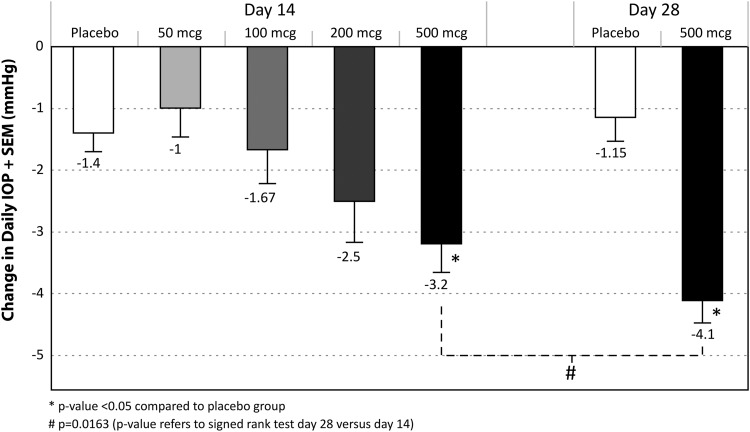
Figure 1 shows the Daily IOP Change for each of the dose groups. An increase in IOP-lowering efficacy was seen with increasing dose, with no apparent plateau in the dose-efficacy response up to the highest dose tested. In the 500 mcg group, efficacy significantly improved between weeks 2 and 4 of treatment (P = 0.0163).
FIG. 1.
Daily IOP Change on Day 14 and Day 28. IOP, intraocular pressure.
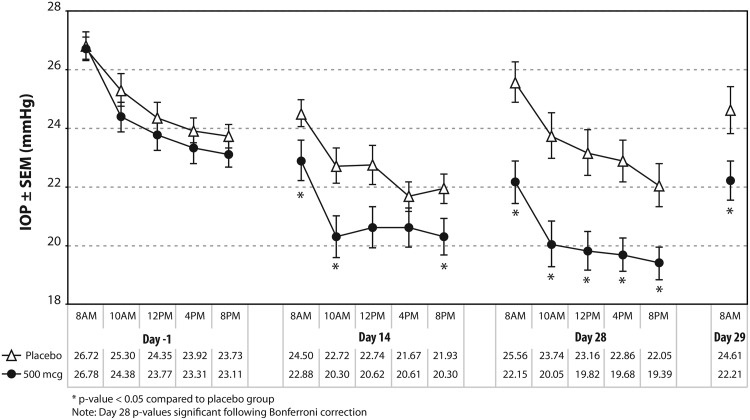
Figure 2 shows the mean IOP for the 500 mcg and placebo groups before randomization (Day −1), and at 14 and 28 days after randomization, over a 12-h dosing interval including 8 AM, 10 AM, 12 PM, 4 PM, and 8 PM, along with the mean IOP on Day 29 at 8 AM. On Day 28, there were statistically significant reductions in IOP in the 500 mcg trabodenoson group, compared with placebo subjects, at all time points throughout the 12-h dosing interval (P ≤ 0.005). All P values remained statistically significant after applying the Bonferroni multiplicity correction. The last dose of trabodenoson was administered at 8AM on Day 28, and a significant reduction in mean IOP versus placebo (P = 0.048) was observed 24 h after this dose at 8 AM on Day 29.
FIG. 2.
Mean IOP for the trabodenoson 500 mcg and placebo groups before randomization (Day −1) and after randomization (Days 14, 28, and 29).
The IOP Change (from diurnal baseline) for the 500 mcg group at Day 28 ranged from −3.5 to −5.0 mmHg with both a mean and median drop of 4.1 mmHg, compared to a range −1.0 to −2.5 mmHg with a mean and median of −2.0 mmHg and −1.6 mmHg, respectively for the concurrently treated placebo group.
The Study Baseline IOP Changes (from 8 AM predose study baseline) at Day 28 were consistent with the changes from the diurnal baseline for the 500 mcg trabodenoson dose, with all changes being statistically significant from the placebo group at all time-matched points (P value range between <0.001 and 0.021). The Study Baseline IOP Change for the trabodenoson 500 mcg dose ranged from −4.0 to −7.0 mmHg with a mean and median drop of −6.1 mmHg and −6.5 mmHg, respectively; placebo Study Baseline IOP Change ranged from −1.0 to −4.7 mmHg with a mean and median of −3.6 mmHg and −3.3 mmHg, respectively.
Subgroup analysis revealed no significant differences in IOP response based on Day 1, 8 AM pretreatment baseline IOP (≥25/<25 and ≥26/<26 mmHg), race (African American/not African American), diagnosis (OHT/POAG), or washout from prior antiglaucoma medications status (requiring washout/not requiring washout).
PK results
Trabodenoson was rapidly distributed into plasma with a tmax of ∼5 min for the 50–200 mcg dose groups and ∼17 min for the 500 mcg dose group. The increases in plasma exposure to trabodenoson and its metabolite INO-2446 were approximately proportional to the doses administered, with exposure to the metabolite ranging from ∼30%–39% of the parent based on AUC from time zero to the last time point (AUC0-last). Trabodenoson was rapidly eliminated from plasma with a mean half-life (t1/2) that ranged from 0.36 to 1.2 h. The apparent mean t1/2 for INO-2446 was ∼0.41–6.1 h.
Discussion
This study demonstrates that trabodenoson, a highly selective adenosine mimetic targeting the adenosine A1 receptor, is safe and well tolerated and produces clinically and statistically significant IOP reductions in eyes with ocular hypertension or POAG.
The overall placebo response observed in this trial, which likely represents a combination of regression to the mean and a true placebo effect, is consistent with a 2.01 mmHg change observed in a recent meta-analysis.21 Increasing doses of trabodenoson resulted in a dose-related improvement in IOP reduction, and no plateau in the dose-efficacy response was apparent up to the highest dose tested. This suggests that higher trabodenoson doses may result in greater IOP reduction than reported here. At the highest dose tested (500 mcg), trabodenoson dosed twice daily produced IOP reductions at Day 28 from diurnal baseline ranging from 3.5 to 5.0 mmHg and from study baseline ranging from 4.0 to 7.0 mmHg. The trabodenoson IOP reductions seen at Day 28 were greater than at Day 14, suggesting increased efficacy with longer treatment, and that reaching a pharmacodynamic steady state requires at least 4 weeks of therapy. Trabodenoson's IOP-lowering effect lasted at least 24 h after the last dose, as evidenced by significant IOP reduction at 8 AM on Day 29 in the 500 mcg group (Fig. 2).
Overall, trabodenoson was safe and well tolerated in all dose groups. There were no serious AEs, and no treatment-related AE was judged as severe by investigators. No subject discontinued the trial due to an AE. The most common treatment-related AEs were conjunctival and ocular hyperemia, together occurring in ∼20% of subjects receiving trabodenoson, with the majority (62.5%) being mild and the rest (37.5%) moderate. Approximately 50% of the cases of conjunctival hyperemia, and 75% of the cases of ocular hyperemia, were reported at a single site among the 18 clinical sites, suggesting a reporting bias. Based on the regular protocol-driven assessment of hyperemia during ocular exams, using a visual hyperemia scale, the frequency of conjunctival hyperemia in the dose groups—before receiving any study drug other than the placebo used during the run-in—was significantly unbalanced between treatment groups (Table 4). For example, at baseline (Day 1 AM predose, before receiving active study drug) the hyperemia rate was 11.8% in the treatment group that went on to be randomized to the 500 mcg trabodenoson group, compared to 0 to 1.7% across subjects that would be randomized to all other treatment groups. Thus, the 12.1% rate of conjunctival hyperemia in the 500 mcg group at the end of the study (on Day 28) may have been due to the underlying hyperemia burden present in this group at baseline, rather than secondary to trabodenoson treatment. Additionally, this higher hyperemia rate at baseline may have also contributed to the higher number of hyperemia-related AEs in this group. Lastly, in a Phase I study of trabodenoson at doses up to 3,200 mcg in the study eye twice daily (6,400 mcg daily), only a single sporadic AE of hyperemia was observed in a subject receiving the lowest dose of trabodenoson (200 mcg twice daily in the study eye). In this study, the only other treatment-related AE in the combined trabodenoson groups was a single case of eyelid pruritus graded as mild in a subject receiving 200 mcg twice daily. Across all subjects and doses of trabodenoson in both the Phase I study and this study (with total daily doses ranging from 100 to 6,400 mcg), no dose-limiting toxicities were identified.
Trabodenoson represents a potential new class of IOP-lowering drug therapy with a novel mechanism of action. Selective stimulation of the adenosine A1 receptor on human TM cells in culture results in the release of MMP-2, which is reported to be involved in the remodeling of the TM's ECM, as a means to lower IOP by increasing trabecular outflow facility.15–18 Of the current IOP-lowering medications available for use, only pilocarpine and related miotics consistently increase outflow facility.22 Although some prostaglandin analogs may also increase outflow facility, the literature is not entirely consistent on this point.23–25 POAG is characterized by reduction of outflow facility, with the site of outflow obstruction traditionally believed to be the juxtacanalicular region of the TM. The nature of this obstruction remains incompletely characterized, but is thought, in part, to involve abnormal aggregation of type IV collagen and elastic fibers within the trabecular ECM.26–28 Trabodenoson is an adenosine mimetic with a high binding affinity (Ki = 0.97 nM) and selectivity for the A1 receptor. Activation of the A1 adenosine receptor promotes the phosphorylation of the extracellular signal-regulated kinases ERK1 and ERK2, resulting in increased secretion of MMP-2 and changes in the ECM.29,30 These molecular changes are thought to increase outflow facility (decrease resistance at the TM) and result in an increase in the outflow of aqueous humor from the eye via the TM. With the balance of ECM deposition by TM cells, and its digestion and removal by MMPs in part restored, trabodenoson's mechanism of action may be addressing some of the underlying outflow pathophysiology associated with OHT and POAG.
In summary, trabodenoson safely and effectively lowered IOP in eyes with ocular hypertension and POAG, and did not appear to have reached a plateau in the efficacy dose response, at the doses tested to date. The treatment is well tolerated and offers a unique and relevant mechanism of action that may address part of the specific pathophysiology of OHT and glaucoma in the TM, with a resultant increase in aqueous outflow facility. These results support the further clinical evaluation of trabodenoson; Phase 3 clinical trials with higher doses of trabodenoson are underway.
Acknowledgment
The authors are grateful to the Trabodenoson Study Group for support of this clinical trial.
Author Disclosure Statement
J.S.M. is a consultant and member of the Inotek Scientific Advisory Board; R.A.B., W.M., and C.C.R. are employees and own stock and stock options of Inotek Pharmaceuticals; N.S. is a consultant; K.N.S. and H.D. have no competing financial interests.
References
- 1.Gordon M.O., Beiser J.A., Brandt J.D., et al. . The Ocular Hypertension Treatment Study: baseline factors that predict the onset of primary open-angle glaucoma. Arch. Ophthalmol. 120:714–720, 2002; discussion 829–830. [DOI] [PubMed] [Google Scholar]
- 2.Kass M.A., Heuer D.K., Higginbotham E.J., et al. . The Ocular Hypertension Treatment Study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch. Ophthalmol. 120:701–713, 2002 [DOI] [PubMed] [Google Scholar]
- 3.Leske M.C., Heijl A., Hussein M., et al. . Factors for glaucoma progression and the effect of treatment: the early manifest glaucoma trial. Arch. Ophthalmol. 121:48–56, 2003 [DOI] [PubMed] [Google Scholar]
- 4.Heijl A., Leske M.C., Bengtsson B., Hyman L., Bengtsson B., and Hussein M. Reduction of intraocular pressure and glaucoma progression: results from the Early Manifest Glaucoma Trial. Arch. Ophthalmol. 120:1268–1279, 2002 [DOI] [PubMed] [Google Scholar]
- 5.Schwartz G.F., Tan J., and Kotak S. Hyperemia-associated costs of medication changes in glaucoma patients treated initially with prostaglandin analogs. J. Ocul. Pharmacol. Ther. 25:555–561, 2009 [DOI] [PubMed] [Google Scholar]
- 6.Alm A., Grierson I., and Shields M.B. Side effects associated with prostaglandin analog therapy. Surv. Ophthalmol. 53 Suppl 1:S93–S105, 2008 [DOI] [PubMed] [Google Scholar]
- 7.Kucukevcilioglu M., Bayer A., Uysal Y., and Altinsoy H.I. Prostaglandin associated periorbitopathy in patients using bimatoprost, latanoprost and travoprost. Clin. Exp. Ophthal. 42:126–131, 2014 [DOI] [PubMed] [Google Scholar]
- 8.Sanderson J., Dartt D.A., Trinkaus-Randall V., et al. . Purines in the eye: recent evidence for the physiological and pathological role of purines in the RPE, retinal neurons, astrocytes, Muller cells, lens, trabecular meshwork, cornea and lacrimal gland. Exp Eye Res. 127:270–279, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Avila M.Y., Stone R.A., and Civan M.M. A(1)-, A(2A)- and A(3)-subtype adenosine receptors modulate intraocular pressure in the mouse. Br. J. Pharmacol. 134:241–245, 2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tian B., Gabelt B.T., Crosson C.E., and Kaufman P.L. Effects of adenosine agonists on intraocular pressure and aqueous humor dynamics in cynomolgus monkeys. Exp. Eye Res. 64:979–989, 1997 [DOI] [PubMed] [Google Scholar]
- 11.Crosson C.E., and Gray T. Characterization of ocular hypertension induced by adenosine agonists. Investig. Ophthalmol. Vis. Sci. 37:1833–1839, 1996 [PubMed] [Google Scholar]
- 12.Crosson C.E. Adenosine receptor activation modulates intraocular pressure in rabbits. J. Pharmacol. Exp. Ther. 273:320–326, 1995 [PubMed] [Google Scholar]
- 13.Crosson C.E., and Gray T. Modulation of intraocular pressure by adenosine agonists. J. Ocul. Pharmacol. 10:379–383, 1994 [DOI] [PubMed] [Google Scholar]
- 14.Crosson C.E. Ocular hypotensive activity of the adenosine agonist (R)-phenylisopropyladenosine in rabbits. Curr. Eye Res. 11:453–458, 1992 [DOI] [PubMed] [Google Scholar]
- 15.Crosson C.E., Sloan C.F., and Yates P.W. Modulation of conventional outflow facility by the adenosine A1 agonist N6-cyclohexyladenosine. Investig. Ophthalmol. Vis. Sci. 46:3795–3799, 2005 [DOI] [PubMed] [Google Scholar]
- 16.Shearer T.W., and Crosson C.E. Adenosine A1 receptor modulation of MMP-2 secretion by trabecular meshwork cells. Investig. Ophthalmol. Vis. Sci. 43:3016–3020, 2002 [PubMed] [Google Scholar]
- 17.Zhong Y., Yang Z., Huang W.C., and Luo X. Adenosine, adenosine receptors and glaucoma: an updated overview. Biochim. Biophys. Acta. 1830:2882–2890, 2013 [DOI] [PubMed] [Google Scholar]
- 18.Bradley J.M., Kelley M.J., Zhu X., Anderssohn A.M., Alexander J.P., and Acott T.S. Effects of mechanical stretching on trabecular matrix metalloproteinases. Investig. Ophthalmol. Vis. Sci. 42:1505–1513, 2001 [PubMed] [Google Scholar]
- 19.Bradley J.M., Vranka J., Colvis C.M., et al. . Effect of matrix metalloproteinases activity on outflow in perfused human organ culture. Investig. Ophthalmol. Vis. Sci. 39:2649–2658, 1998 [PubMed] [Google Scholar]
- 20.Daines B.S., Kent A.R., McAleer M.S., and Crosson C.E. Intraocular adenosine levels in normal and ocular-hypertensive patients. J. Ocul. Pharmacol. Ther. 19:113–119, 2003 [DOI] [PubMed] [Google Scholar]
- 21.Raber S., Mandema J.W., Li H., and Nickens D.J. A model-based dose-response meta-analysis of ocular hypotensive agents as a drug development tool to evaluate new therapies in glaucoma. J. Ocul. Pharmacol. Ther. 31:189–197, 2015 [DOI] [PubMed] [Google Scholar]
- 22.Toris C.B., Zhan G.L., Zhao J., Camras C.B., and Yablonski M.E. Potential mechanism for the additivity of pilocarpine and latanoprost. Am J. Ophthalmol. 131:722–728, 2001 [DOI] [PubMed] [Google Scholar]
- 23.Toris C.B., Gabelt B.T., and Kaufman P.L. Update on the mechanism of action of topical prostaglandins for intraocular pressure reduction. Surv. Ophthalmol. 53 Suppl 1:S107–S120, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Winkler N.S., and Fautsch M.P. Effects of prostaglandin analogues on aqueous humor pathways. J. Ocul. Pharmacol. Ther. 30:102–109, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Alm A. Latanoprost in the treatment of glaucoma. Clin. Ophthalmol. 8:1967–1985, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lutjen-Drecoll E., Futa R., and Rohen J.W. Ultrahistochemical studies on tangential sections of the trabecular meshwork in normal and glaucomatous eyes. Investig. Ophthalmol. Vis. Sci. 21:563–573, 1981 [PubMed] [Google Scholar]
- 27.Tektas O.Y., and Lutjen-Drecoll E. Structural changes of the trabecular meshwork in different kinds of glaucoma. Exp. Eye Res. 88:769–775, 2009 [DOI] [PubMed] [Google Scholar]
- 28.Lutjen-Drecoll E., Rittig M., Rauterberg J., Jander R., and Mollenhauer J. Immunomicroscopical study of type VI collagen in the trabecular meshwork of normal and glaucomatous eyes. Exp. Eye Res. 48:139–147, 1989 [DOI] [PubMed] [Google Scholar]
- 29.Lu Z., and Xu S. ERK1/2 MAP kinases in cell survival and apoptosis. IUBMB Life. 58:621–631, 2006 [DOI] [PubMed] [Google Scholar]
- 30.Joe M.K., Kwon H.S., Cojocaru R., and Tomarev S.I. Myocilin regulates cell proliferation and survival. J. Biolog. Chem. 289:10155–10167, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]