Abstract
Background:
Endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) is a minimally invasive procedure that has become an important tool in diagnosis and staging of mediastinal lymph node (LN) lesions in lung cancer. Adequate sedation is an important part of the procedure since it provides patient's comfort and potentially increases diagnostic yield. We aimed to compare deep sedation (DS) versus moderate sedation (MS) in patients undergoing EBUS-TBNA procedure.
Methods:
PubMed, EMBASE, MEDLINE, and Cochrane Library were searched for English studies of clinical trials comparing the two different methods of sedations in EBUS-TBNA until December 2015. The overall diagnostic yield, LN size sampling, procedural time, complication, and safety were evaluated.
Results:
Six studies with 3000 patients which compared two different modalities of sedation in patients performing EBUS-TBNA were included in the study. The overall diagnostic yield of DS method was 52.3%–100% and MS method was 46.1%–85.7%. The overall sensitivity of EBUS-TBNA of DS method was 98.15%–100% as compared with 80%–98.08% in MS method. The overall procedural times were 27.2–50.9 min and 20.6-44.1 min in DS and MS groups, respectively. The numbers of LN sampled were between 1.33–3.20 nodes and 1.36–2.80 nodes in DS and MS groups, respectively. The numbers of passes per LN were 3.21–3.70 passes in DS group as compared to 2.73–3.00 passes in MS group. The mean of LN size was indifferent between two groups. None of the studies included reported serious adverse events.
Conclusions:
Using MS in EBUS-TBNA has comparable diagnostic yield and safety profile to DS. The decision on the method of sedation for EBUS-TBNA should be individually selected based on operator experience, patient preference, as well as duration of the anticipated procedure.
Keywords: Endobronchial ultrasound, sedation, transbronchial needle aspiration
INTRODUCTION
Endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) has become a standard procedure in diagnosis and staging of lung cancer.[1,2] Sedation method is one of the crucial steps in EBUS-TBNA procedures. A successful sedation provides comfortable environment for the patient while enabling the bronchoscopist to obtain adequate tissue.
Types of sedation in this procedure have been mostly institutional and practitioner dependent. Two common types of sedation used in EBUS-TBNA: (1) Deep sedation (DS) or general anesthesia and (2) moderate sedation (MS) or conscious sedation. DS using propofol has acceptable safety profile in endoscopic procedures.[3,4] Propofol is a rapid-acting sedative that allows quick recovery. This medication has both amnestic and antiemetic effects but has no analgesic activity.[5] MS is mostly preferred method for procedures which requires rapid recovery. A combination of fentanyl and midazolam is commonly used in endoscopic procedures for sedation. Midazolam is the benzodiazepine of choice because of its rapid-onset and short duration.[6] Fentanyl is a preferred opioid[7,8] because it has high potency, fast onset of action, few adverse events, synergy with benzodiazepines and it is cleared rapidly.[8,9,10] Meperidine, a short-acting opioid narcotic with a half-life of 3.2 h, also had been used in short procedures for MS.[11,12]
Only a few published studies compared types of sedation with procedural outcomes with EBUS-TBNA. In this study, we performed a systematic review of the medical literature to evaluate the studies that compared the impact of DS versus MS on diagnostic yield, safety, and lymph node (LN) sampling.
METHODS
Search strategy
The search strategy was developed by PA, CL, and FK. An experienced librarian was consulted for further developing the search strategy. The search included literature search from the following biomedical databases: EMBASE, MEDINE, and Cochrane Library for relevant studies published until December 2015. The search terms were “endobronchial ultrasound” or “endobronchial ultrasonography” or “EBUS” or “endobronchial ultrasound-guided” and “sedation” or “anesthesia” or “deep sedation” or “conscious sedation” or “moderate sedation”. References of identified articles were also searched manually. Only English papers were selected.
Study selection
Two reviewers (MK and FK) independently judged study eligibility while screening the citations. Only full-text articles that compared types of sedation in EBUS-TBNA were selected. Both prospective and retrospective studies were included in our study. Case studies, letter reports, conference abstracts, or pediatric population were excluded from this review. All data were verified for internal consistency and discrepancy was resolved by discussion among all reviewers. Disagreements were resolved by discussion and consultation with a fifth author (AA). The fifth author was involved in the writing, editing, and conducting the discussion. To ensure consistency, we conducted calibration exercises and pilot test the screening forms prior to starting the process.
We classified sedation method into two categories, DS and MS. DS is defined as a method using medication-induced depression of consciousness; during this method, patients cannot be easily aroused but respond purposefully following repeated or painful stimulation. The ability to independently maintain ventilatory function may be impaired. Patients may require assistance in maintaining a patent airway, and spontaneous ventilation may be inadequate.[13] In this review, propofol was the main medication used for DS method.
MS defined as a method using medication to suppress level of consciousness; by this method, patients will respond purposefully to verbal commands, either alone or accompanied by light tactile stimulation. No interventions are required to maintain a patient airway, and spontaneous ventilation is adequate.[13] In this review, midazolam, meperidine, and fentanyl are included in MS method.
Data abstraction and quality assessment
The following information was obtained from each study: Publication type (title, first author, center in which the study was done, time frame of each trial, and date published), study design, LN size, number of biopsy attempt, diagnostic yield, and complication. All data were verified for internal consistency and discrepancy was resolved by discussion among all reviewers. The quality of evidence presented in the studies were evaluated independently by two authors (CL and MK) using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) System.[14] All disagreements were resolved by discussion with the fifth author (AA).
RESULTS
Overview of eligible trials
The bibliographic search yielded 115 papers. Titles and abstracts were reviewed and 105 were excluded based on our exclusion criteria. The remaining 10 full-text articles were subsequently selected for further analysis. We excluded four studies that used only MS method.[15,16,17,18] Only six studies were included in our final analysis.[19,20,21,22,23,24]
Characteristics and quality of selected studies
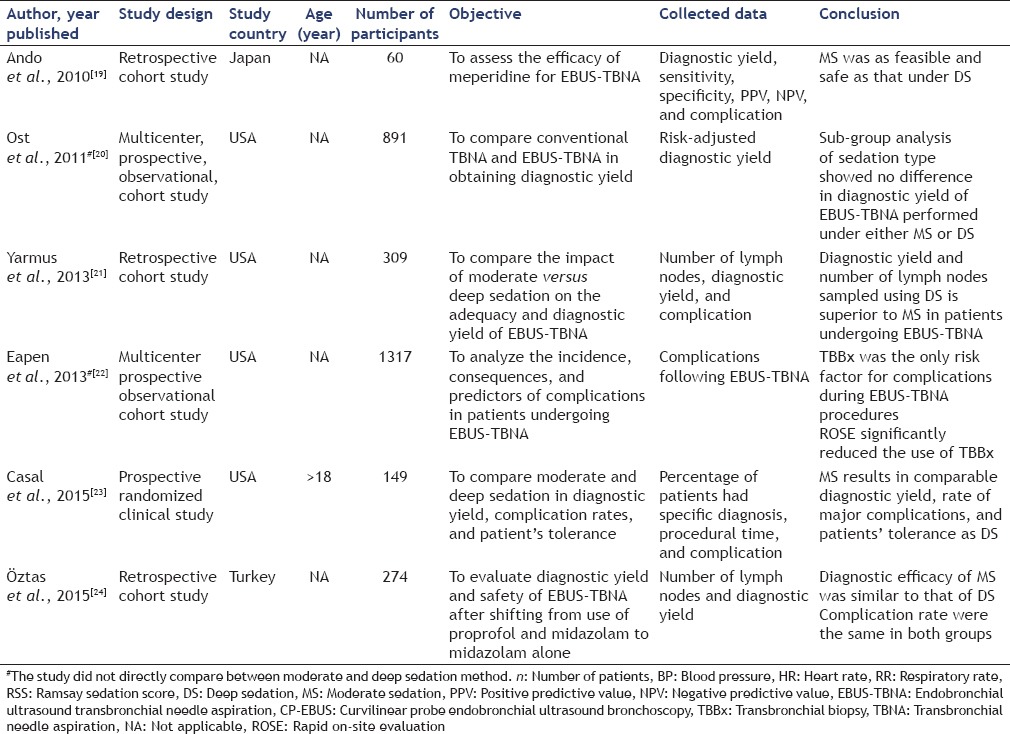
The main characteristics of eligible studies are described in Table 1. A total of six studies were included in the review.[19,20,21,22,23] All studies were published in English. Two of them were multicenter studies.[20,22] Four studies were conducted in USA,[20,21,22,23] one study in Turkey,[24] and one study in Japan.[19] According to the GRADE Scale,[14] the level of evidence was moderate in one study[23] and low in all the remaining studies.[19,20,21,22,24]
Table 1.
Characteristics of reviewed studies
Diagnostic yield
Five studies[19,20,21,23,24] assessed diagnostic yield [Table 2]. The overall diagnostic yields were 52.3%–100.0% in DS group and 46.1%–85.7% in MS group. Ost et al. in their prospective, multicenter, observational study showed diagnostic yield of 52.3% and 46.1% in DS versus MS, respectively (P = 0.08).[20] Under DS, diagnostic yield showed odds ratio (OR) of 1.11 (0.62–2.01) (P = 0.66).[20] There was significant heterogeneity among different centers in terms of diagnostic yield. Patient-level variables that affected diagnostic yield included LN size, smoking status, and number of LN stations undergoing biopsy.[20] Casal et al. in their randomized study showed no difference in diagnostic yield and sensitivity between DS and MS groups.[23] Diagnostic yield in DS group was 70.7% while in MS group was 68.9% (P = 0.816).[23] Sensitivity in DS group was 98.2% compared with moderate anesthesia group was 98.1% (P = 0.79).[23] Ando et al. in their retrospective study supported meperidine as feasible as DS method in diagnostic yield (DS 100% vs. meperidine group 75.7%, P = 0.15).[19] Recently, a retrospective cohort study by Öztas et al. also revealed that DS had similar diagnostic yield to MS method. (77.6% in DS group vs. 85.7% in MS group, P = 0.121).[24]
Table 2.
Compare diagnostic yield between moderate and deep sedation methods in reviewed studies
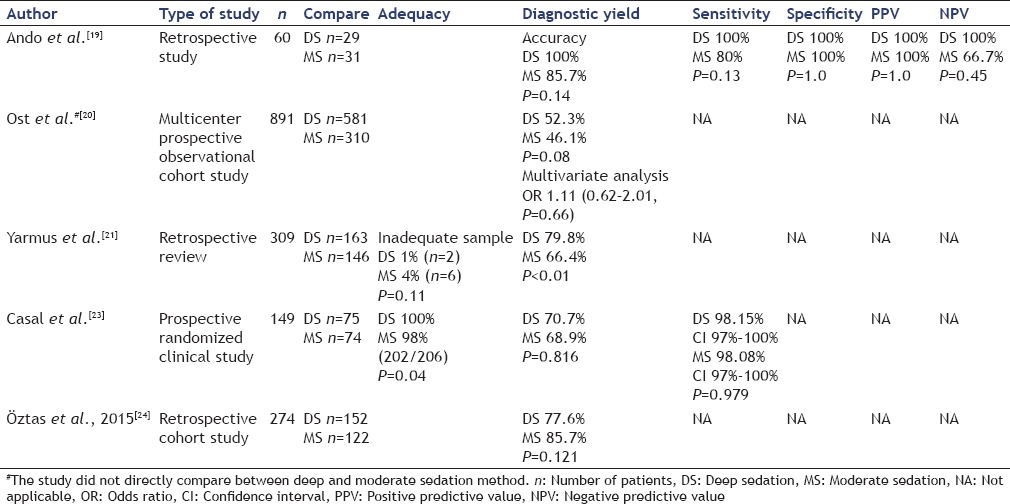
On the other hand, Yarmus et al. in their retrospective study showed that diagnostic yield was higher for the DS group (80% of patients) than for the MS group (66% of patients) (P < 0.01).[21]
Lymph node sampling
Four studies collected LN sampling data.[19,21,23,24] The overall numbers of LN samplings were 1.33–3.20 nodes and 1.36–2.80 nodes in DS and MS groups, respectively. Casal et al. in their randomized control study showed no difference in LN sampling between the two methods of sedation (P = 0.199).[23] However, a retrospective study by Yarmus el al. reported that DS group obtained more LN sampling than MS group (DS 2.17 ± 0.9 vs. MS 1.36 ± 0.6, P < 0.01).[21] A study by Ost et al. also showed that DS method was associated with more LN sampled site per patient (P < 0.001).[20] On the contrary, a study by Öztas et al. showed that the number of aspirated LN per patient was 1.33 ± 0.5 in DS group and 2.21 ± 1.3 in MS group (P = 0.001).[24]
Numbers of passes per lymph node
The overall numbers of passes per LN were 3.21–3.70 and 2.73–3.00 passes in DS and MS groups, respectively. Ando et al. in their study showed that number of aspiration of LN in DS group was higher than MS group (DS 3.21 ± 1.08 vs. MS 2.73 ± 0.69, P < 0.05).[19] Yarmus et al. also showed that number of aspiration of LN in DS group was higher than MS group (DS 3.7 vs. MS 3.0, P < 0.01) [Table 3].[21]
Table 3.
Compare lymph node sampling and procedural time between moderate and deep sedation methods in reviewed studies
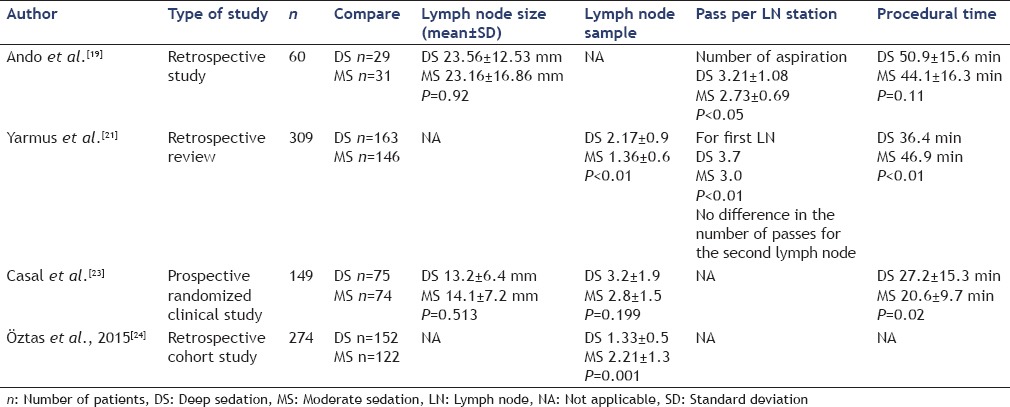
Lymph node size
The overall mean of LN size was 13.20–23.56 mm in DS group and 14.10–23.16 mm in MS group. In study by Ando et al., LN size in DS group was 23.56 ± 12.53 mm and in MS group was 23.16 ± 16.86 mm (P = 0.92).[19] In study by Casal et al., LN size was 13.2 ± 6.4 mm in DS group and 14.1 ± 7.2 mm in MS group (P = 0.513).[23]
Procedural time
Three studies provided data comparing procedural time between DS and MS groups.[19,21,23] The overall procedural times were 27.2–50.9 min in DS group and 20.6–44.1 min in MS group. Ando et al. showed no difference in procedural time between two groups.[19] Yarmus et al. showed DS group had shorter mean procedural time than the other group (P < 0.01).[21] However, Casal et al. showed DS group had more time consuming than MS group (DS 27.2 ± 15.3 min vs. MS 20.6 ± 9.7 min, P = 0.02)[23] [Table 3].
Safety
Complications from EBUS-TBNA were compared between two sedation methods [Table 4].
Table 4.
Compare complications between moderate and deep sedation methods in reviewed studies
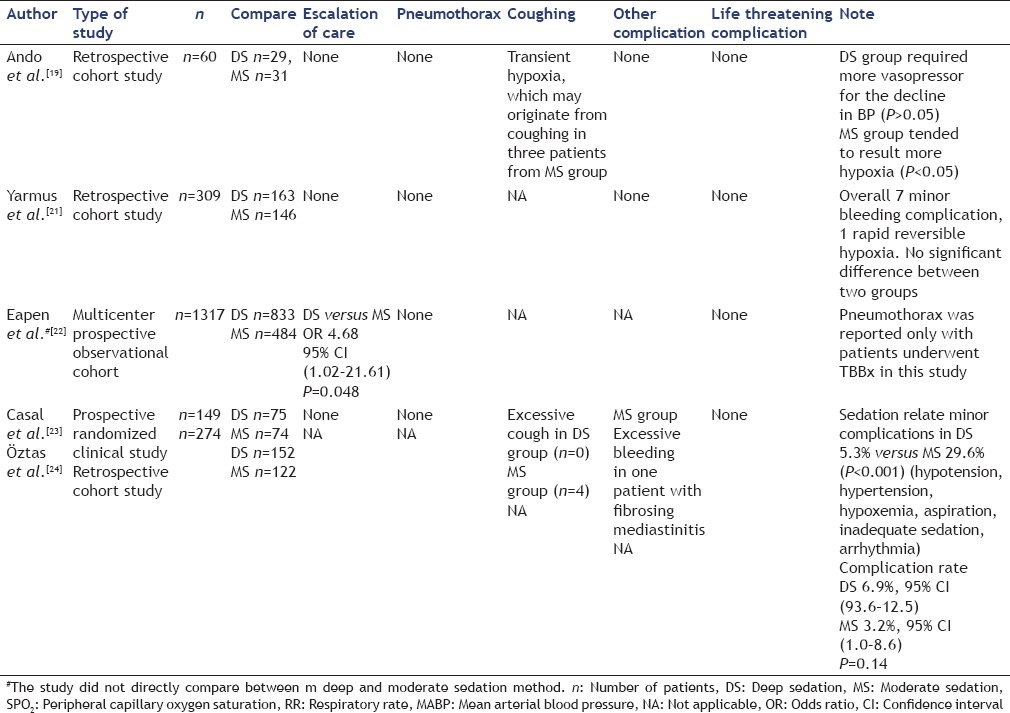
Coughing
Two studies assessed the incidence of coughing and concluded that coughing was more common in MS group.[19,23]
Pneumothorax and major bleeding
No pneumothorax or significant bleeding event was reported during the EBUS-TBNA procedure using DS or MS.
Escalation of care
Four studies compared escalation of care defined as transferring patient to into the intensive care unit between DS and MS groups.[19,21,22,23] Three studies showed no difference in escalation of care between two groups.[19,21,23] Multivariate analysis of Eapen's multicenter prospective observational cohort study founded that patients undergoing DS had higher incident of escalation of care compared to MS group (OR 4.68%, 95% confidence interval [CI] [1.02–21.61, P = 0.048]).[22]
Other specific considerations during procedure
Using meperidine in elderly patients
Although meperidine is known to cause cardiovascular as well as respiratory depression and should be cautiously used in elderly patients,[25,26] there was no statistically significant difference in complication between elderly and young group.[19]
Inadequate sedation for moderate sedation group
One patient in meperidine group in Ando et al. study needed additional midazolam because of increased restlessness during the examination.[19]
Cardiorespiratory depression in deep sedation group
Adverse effects of propofol are respiratory depression, apnea, and hypotension.[27] DS group required more vasopressor for the decline in blood pressure than MS group (DS 17.2% vs. MS 0, P < 0.05).[19] However, there was no significant difference in serious complication.
Patient satisfaction
Only Casal et al. study assessed patient satisfaction. There was no significant difference between two groups. The study showed that patients in the MS group recalled the procedure more often (P < 0.05).[23] However, most patients stated that they were willing to undergo the procedure again under the same modality.[23]
DISCUSSION
EBUS-TBNA has become the method of choice for enlarged hilar/mediastinal lymph adenopathy diagnosis as well as staging of lung cancer over the past decade. However, the optimal method for sedation in EBUS-TBNA is still debatable. To the best of our knowledge, this is the first systematic review that compares MS and DS methods in patients undergoing EBUS-TBNA.
Our review showed that the overall diagnostic yield is comparable between the two sedation modalities despite an increase in procedure time in the DS group. However, the choice of sedation should be chosen according to several factors. DS may be preferred in cases that require additional procedures such as endobronchial stent besides EBUS/TBNA or in centers where trainees are still acquiring skills of such a procedure. Moreover, DS might be advantageous for EBUS/TBNA procedures where comprehensive staging or small pulmonary node sampling is done, particularly for novice bronchoscopists.[28] For uncomplicated cases in experienced performers, either DS or MS might have similar outcome.[28] It is crucial to realize that the trials published comparing different modalities of sedation in patients undergoing EBUS/TBNA are performed in an academic and/or high volume patient population and thus, might not be applicable for physicians who perform such procedures nonroutinely. Another important issue to consider is whether MS or DS are cost-effective. Unfortunately, none of the studies presented compared the difference in cost care among different choices of sedation.
Our review had several limitations. We combined included only English-published literatures. The choice of sedation cannot be blinded to the operator performing EBUS/TBNA. Two studies did not directly compare between two sedation methods, and we could only imply results from subgroup analysis.[20,22] One study did not compare the procedure in the same center that may lead to information bias.[21] Finally, one study did not concurrently compare two methods of sedation; therefore, the increasing in procedural skill of the bronchoscopist overtime can be a confounding factor.[24]
CONCLUSIONS
Although our study showed that using MS in EBUS-TBNA had comparable diagnostic yield and safety to DS method, the decision to select sedation modality should be based on several factors such as physician expertise, duration of the procedure, patient choice, and possibly cost-effectiveness.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Yasufuku K, Chiyo M, Sekine Y, et al. Real-time endobronchial ultrasound-guided transbronchial needle aspiration of mediastinal and hilar lymph nodes. Chest. 2004;126:122–8. doi: 10.1378/chest.126.1.122. [DOI] [PubMed] [Google Scholar]
- 2.Ernst A, Anantham D, Eberhardt R, et al. Diagnosis of mediastinal adenopathy-real-time endobronchial ultrasound guided needle aspiration versus mediastinoscopy. J Thorac Oncol. 2008;3:577–82. doi: 10.1097/JTO.0b013e3181753b5e. [DOI] [PubMed] [Google Scholar]
- 3.Clarkson K, Power CK, O’Connell F, et al. A comparative evaluation of propofol and midazolam as sedative agents in fiberoptic bronchoscopy. Chest. 1993;104:1029–31. doi: 10.1378/chest.104.4.1029. [DOI] [PubMed] [Google Scholar]
- 4.Rex DK, Overley C, Kinser K, et al. Safety of propofol administered by registered nurses with gastroenterologist supervision in 2000 endoscopic cases. Am J Gastroenterol. 2002;97:1159–63. doi: 10.1111/j.1572-0241.2002.05683.x. [DOI] [PubMed] [Google Scholar]
- 5.McKeage K, Perry CM. Propofol: A review of its use in intensive care sedation of adults. CNS Drugs. 2003;17:235–72. doi: 10.2165/00023210-200317040-00003. [DOI] [PubMed] [Google Scholar]
- 6.Fragen RJ. Pharmacokinetics and pharmacodynamics of midazolam given via continuous intravenous infusion in intensive care units. Clin Ther. 1997;19:405–19. doi: 10.1016/s0149-2918(97)80126-9. [DOI] [PubMed] [Google Scholar]
- 7.Rayburn WF, Smith CV, Parriott JE, et al. Randomized comparison of meperidine and fentanyl during labor. Obstet Gynecol. 1989;74:604–6. [PubMed] [Google Scholar]
- 8.Mostert JW, Trudnowski RJ, Seniff AM, et al. Clinical comparison of fentanyl with meperidine. J Clin Pharmacol J New Drugs. 1968;8:382–91. doi: 10.1002/j.1552-4604.1968.tb00114.x. [DOI] [PubMed] [Google Scholar]
- 9.Flacke JW, Flacke WE, Bloor BC, et al. Histamine release by four narcotics: A double-blind study in humans. Anesth Analg. 1987;66:723–30. [PubMed] [Google Scholar]
- 10.Mather LE. Clinical pharmacokinetics of fentanyl and its newer derivatives. Clin Pharmacokinet. 1983;8:422–46. doi: 10.2165/00003088-198308050-00004. [DOI] [PubMed] [Google Scholar]
- 11.Robertson DJ, Jacobs DP, Mackenzie TA, et al. Clinical trial: A randomized, study comparing meperidine (pethidine) and fentanyl in adult gastrointestinal endoscopy. Aliment Pharmacol Ther. 2009;29:817–23. doi: 10.1111/j.1365-2036.2009.03943.x. [DOI] [PubMed] [Google Scholar]
- 12.Ali S, Davidson DL, Gremse DA. Comparison of fentanyl versus meperidine for analgesia in pediatric gastrointestinal endoscopy. Dig Dis Sci. 2004;49:888–91. doi: 10.1023/b:ddas.0000030106.01928.b4. [DOI] [PubMed] [Google Scholar]
- 13.American Society of Anesthesiologists Task Force on Sedation and Analgesia by Non-Anesthesiologists. Practice guidelines for sedation and analgesia by non-anesthesiologists. Anesthesiology. 2002;96:1004–17. doi: 10.1097/00000542-200204000-00031. [DOI] [PubMed] [Google Scholar]
- 14.Balshem H, Helfand M, Schünemann HJ, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. 2011;64:401–6. doi: 10.1016/j.jclinepi.2010.07.015. [DOI] [PubMed] [Google Scholar]
- 15.Dal T, Sazak H, Tunç M, et al. A comparison of ketamine-midazolam and ketamine-propofol combinations used for sedation in the endobronchial ultrasound-guided transbronchial needle aspiration: A prospective, single-blind, randomized study. J Thorac Dis. 2014;6:742–51. doi: 10.3978/j.issn.2072-1439.2014.04.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee HJ, Haas AR, Sterman DH, et al. Pilot randomized study comparing two techniques of airway anaesthesia during curvilinear probe endobronchial ultrasound bronchoscopy (CP-EBUS) Respirology. 2011;16:102–6. doi: 10.1111/j.1440-1843.2010.01861.x. [DOI] [PubMed] [Google Scholar]
- 17.Goyal G, Pisani MA, Murphy TE, et al. Advanced diagnostic bronchoscopy using conscious sedation and the laryngeal nerve block: Tolerability, thoroughness, and diagnostic yield. Lung. 2014;192:905–13. doi: 10.1007/s00408-014-9607-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chrissian AA, Bedi H. Bronchoscopist-directed continuous propofol infusion for targeting moderate sedation during endobronchial ultrasound bronchoscopy: A practical and effective protocol. J Bronchology Interv Pulmonol. 2015;22:226–36. doi: 10.1097/LBR.0000000000000187. [DOI] [PubMed] [Google Scholar]
- 19.Ando K, Ohkuni Y, Fukazawa M, et al. Sedation with meperidine for endobronchial ultrasound-guided transbronchial needle aspiration. J Bronchology Interv Pulmonol. 2010;17:329–33. doi: 10.1097/LBR.0b013e3181f4196d. [DOI] [PubMed] [Google Scholar]
- 20.Ost DE, Ernst A, Lei X, et al. Diagnostic yield of endobronchial ultrasound-guided transbronchial needle aspiration: Results of the AQuIRE bronchoscopy registry. Chest. 2011;140:1557–66. doi: 10.1378/chest.10-2914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yarmus LB, Akulian JA, Gilbert C, et al. Comparison of moderate versus deep sedation for endobronchial ultrasound transbronchial needle aspiration. Ann Am Thorac Soc. 2013;10:121–6. doi: 10.1513/AnnalsATS.201209-074OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Eapen GA, Shah AM, Lei X, et al. Complications, consequences, and practice patterns of endobronchial ultrasound-guided transbronchial needle aspiration: Results of the AQuIRE registry. Chest. 2013;143:1044–53. doi: 10.1378/chest.12-0350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Casal RF, Lazarus DR, Kuhl K, et al. Randomized trial of endobronchial ultrasound-guided transbronchial needle aspiration under general anesthesia versus moderate sedation. Am J Respir Crit Care Med. 2015;191:796–803. doi: 10.1164/rccm.201409-1615OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Öztas S, Aktürk ÜA, Alpay LA, et al. A comparison of propofol-midazolam and midazolam alone for sedation in endobronchial ultrasound-guided transbronchial needle aspiration: A retrospective cohort study. Clin Respir J. 2015 doi: 10.1111/crj.12442. [DOI] [PubMed] [Google Scholar]
- 25.Hagmeyer KO, Mauro LS, Mauro VF. Meperidine-related seizures associated with patient-controlled analgesia pumps. Ann Pharmacother. 1993;27:29–32. doi: 10.1177/106002809302700106. [DOI] [PubMed] [Google Scholar]
- 26.Stone PA, Macintyre PE, Jarvis DA. Norpethidine toxicity and patient controlled analgesia. Br J Anaesth. 1993;71:738–40. doi: 10.1093/bja/71.5.738. [DOI] [PubMed] [Google Scholar]
- 27.José RJ, Shaefi S, Navani N. Sedation for flexible bronchoscopy: Current and emerging evidence. Eur Respir Rev. 2013;22:106–16. doi: 10.1183/09059180.00006412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wahidi MM, Sterman DH. Bringing comfort to endobronchial ultrasound bronchoscopy. Am J Respir Crit Care Med. 2015;191:727–8. doi: 10.1164/rccm.201502-0291ED. [DOI] [PubMed] [Google Scholar]


