Abstract
The majority of strokes are due to blockage of an artery in the brain by a blood clot. Prompt treatment with thrombolytic drugs can restore blood flow before major brain damage has occurred. We report the case series of all patients who were treated with rt-PA at Stroke Unit of HASSAN II University hospital between 2010 and 2013. There were 52 patients treated with intravenous rtPA during the study period. The mean age was 63 years with the no gender predominance (sex ratio 1.02). Hypertension was the most common vascular risk factor (31%) and 17% of patients suffered from atrial fibrillation. 17 of 52 patients (32.7%) were treated within a 3 hours window of stroke onset and 35 of 52 (67.3%) patients were treated within 3-4.5 h. Twenty five patients (48%) had significant early improvements within 24 hours and twenty one (40.3%) patients had good outcomes at 3 months and fifteen patients (29%) died within the same period.
Keywords: Intravenous thrombolysis, stroke, rt-PA
Introduction
Stroke is one of the leading causes of disability and death in both developing and developed countries. Each year, about 22 million people have a stroke world-wide. While the incidence of stroke in developed countries declined 42% between 1970 and 2008, it doubled in developing countries and exceeded the developed countries between 2000 and 2008 [1, 2]. The prevalence rate of stroke survivors in Morocco is 292/100.000 [3]. Intravenous thrombolytic therapy has been widely recommended as a standard treatment for acute ischemic stroke in most clinical practice guidelines. With the approval of tissue plasminogen activator (rt-PA) for the acute ischemic stroke management, the evolution of this emergency has changed dramatically. However, the number of stroke units and experience on stroke thrombolysis in North Africa is still limited. Lack of infrastructure is main barriers of thrombolysis therapy in developing countries [4, 5]. On 2007, the first stroke unit in Morocco was created in university hospital of Fez, and the first thrombolysis was done on 2010. We report the case series of thrombolytic therapy in Morocco.
Methods
Patient with acute ischemic stroke treated with intravenous rt-PA at Stroke Unit of HASSAN II University hospital between 2010 and 2013 were included. Intravenous rt-PA was prescribed for acute ischemic stroke within 4.5 hours of onset. Inclusion and exclusion criteria were even that those used in the National Institute of Neurological Disorders and Stroke (NINDS) study [6]. However, in our study older age (more than 80 years old) was not an exclusion criterion. Patients with high blood pressure (systolic blood pressure above 185 mmhg or diastolic blood pressure above 110 mmhg) were not excluded if their blood pressure could be controlled by intravenous nicardipine before rtPA administration.
All patients had pretreatment non contrast CT scans of the brain except for Wake up stroke, where the patients had cerebral MRI. CT scans were evaluated by a neurologist. Informed consent was obtained from all patients, after discussion of the potential benefits and risks, including the risk of symptomatic intracerebral hemorrhage (ICH). Contraindications for thrombolysis included evidence of intracranial hemorrhage, or hypodensity greater than 1/3 of the middle cerebral artery territory in the first year of study. After this period, we used Alberta Stroke Program early CT score (ASPECTS) [7]. Score < 7 was considered as exclusion criteria. The dose of administered rt-PA was 0.9 mg /kg body weight with a maximum of 90 mg. According to protocol, 1/10 of total dose of rt-PA was given intravenously in a bolus and the remaining 9/10 during 1 hour. All Patient treated with intravenous rtPA were admitted to Stroke Unit for clinical monitoring. The initial severity of the stroke and evolution after thrombolysis was evaluated using the National Instituted of Health Stroke Scale (NIHSS). A second cerebral CT scan was performed 24 hours after receiving thrombolysis. Hemorrhagic brain lesion and death were also recorded. Clinical assessment was repeated with NIHSS after 24 hours. Early clinical improvement was defined according to the NINDS criteria as 4-point improvement in the NIHSS score from baseline values or complete resolution of neurological deficit. Significant clinical deterioration was defined as 4-point NIHSS deterioration at 24 hours. The modified Rankin scale (mRS) was evaluated after 90 days. The outcome was considered as good outcome if mRS at 3 months was between 0 and 2. Symptomatic intracranial hemorrhage was defined according to ECASS III as any hemorrhage with neurologic deterioration combined with an NIHSS score 4 points greater than either the baseline value or the lowest value in the first 7 days, or death [8].
All patients were registered in the International Stroke Thrombolysis Register (ISTR) to compare our results with other centers worldwide [9]. It is an internet-based, international monitoring registry for auditing the safety and efficacy of routine therapeutic use of thrombolysis in acute ischemic stroke. To evaluate difference in prognosis between the first period of starting thrombolysis in our center without using ASPECTS and second period when we use it, we divided the group on two subgroups. First subgroup from April 2010 to December2011, the second from January 2012 to December 2013.
Results
There were 52 patients treated with intravenous rtPA during the study period. The demographic characteristics, vascular risk factors, stroke subtype, and baseline clinical parameters are given in Table 1. The mean age was 63 years with the no gender predominance (sex ratio 1.02). Hypertension was the most common vascular risk factor (31%) and 17% of patients suffered from atrial fibrillation. 17 of 52 patients (32.7%) were treated within a 3 hours window of stroke onset and 35 of 52 (67.3%) patients were treated within 3-4.5 h. Mean door-to-needle time was 75 min. Mean onset-to treatment time (OTT) was 212 minutes (Table 2). Systolic and diastolic blood pressures at admission were 139 mmHg and 78 mmHg respectively. Initial median NIHSS score was 14. The initial NIHSS was more severe in the first subgroup (NIHSS> 15 in 58 % of patients) than in the second subgroup (NIHSS> 15 in only 28 % of patients) (Table 3). Median NIHSS changes 2 hours post thrombolysis was -3. Median NIHSS changes 24 hours post thrombolysis was -2. There were three asymptomatic ICH (5,7%) and four symptomatic ICHs (7,7%). Two of the four symptomatic ICHs were fatal. Four patients had minimal gingival hemorrhages and only one case of hematuria without haemodynamic compromise. Twenty five patients (48%) had significant early improvements within 24 hours and twenty one (40,3%) patients had good outcomes at 3 months and fifteen patients (29%) died within the same period (Table 4). The causes of death were cerebral infarct (4/15: 26,6%), acute myocardial infarction (1/15: 6,6%), intracerebral hemorrhage (2/15:13,3%), unknown causes (4/15: 26,6%) and other cause (4/15: 26,6%).
Table 1.
Demographic and baseline clinical characteristics
| Baseline characteristics | Morocco center |
|---|---|
| Age (Mean) | |
| Female (%) | |
| Male (%) | |
| Risk factors | |
| Hypertension | 31% |
| Diabetes | 12% |
| Hyperlipidaemia | 8% |
| Curent smoker | 4% |
| Previous smoker | |
| Previous clin. diag. ischaemic stroke (earlier than 3 m) | 4% |
| Previous clin. diag. ischaemic stroke (within 3 m) | 2% |
| Atrial fibrillation | 17% |
| Congestive heart failure | 10% |
| Baseline NIHSS | |
| Median NIHSS | 14.0 |
| NIH LEVEL 0-7 | 2% |
| NIH LEVEL8-14 | 52% |
| NIH LEVEL 15PLUS | 46% |
| Ischemic Stroke Subgroups | |
| I63.0: Cerebral infarct, large vessel disease with significant carotid stenosis (>50% NASCET) | 9% |
| I63.3: Cerebral infarct, other large vessel disease | 23% |
| I63.4: Cerebral infarct, cardiac emboli | 50% |
| I63.5: Cerebral infarct, small vessel/lacunar | 0% |
| I63.6: Cerebral infarct, sinus venous thrombosis | 0% |
| I63.8: Cerebral infarct, other/ unusual cause | 0% |
| I63.9: Cerebral infarct, multiple/ unknown cause | 18% |
Table 2.
Time delay and comparison with SITS ISTR results
| Time delay (minutes) | Morocco Center | Within 3 hours SITS-ISTR | Within 3 to 4.5hours SITS-ISTR |
|---|---|---|---|
| Onset to treating hospital/door time(median) | 120.0 | 65.0 | 130.0 |
| Door to treatment/needle time (median) | 75.0 | 65.0 | 80 |
| Onset to treatment/needle time (median) | 209.0 | 138.0 | 210 |
Table 3.
Initial NIHSS in the 2 subgroups
| 2010-2011 | 2012-2013 | |
|---|---|---|
| Median NIHSS | 15 | 14 |
| NIH LEVEL0-7 | 3% | 0% |
| NIH LEVEL8-14 | 39% | 72% |
| NIH LEVEL15 Plus | 58% | 28% |
Table 4.
Clinical outcome details
| Clinical outcome details | Morocco Center |
|---|---|
| NIHSS changes within 24h | |
| Change in NIHSS 0-2h (median) | -3.0 |
| Change in NIHSS 0-24h (median) | -2.0 |
| Significant early improvements | 48% |
| Significant deterioration | 29% |
| Rankin 3 months | |
| 0 No symptoms at all | 16% |
| 1 No significant disabling symptoms | 18% |
| 2 Slight disability | 6% |
| 3 Moderate disability | 6% |
| 4 Moderate severe disability | 24% |
| 5 Severe disability | 2% |
| 6 Dead | 29% |
| Global Outcome (24h) | |
| Much better | 17% |
| Better | 33% |
| Unchanged | 23% |
| Worse | 12% |
| Much worse | 6% |
| Dead | 10% |
Discussion
We analyzed the data of 52 thrombolysed patients gathered over a 3years period. In developing countries like morocco, only a small proportion of patients with ischemic stroke currently receive the thrombolytic therapy with IV rt-PA. The reason for this include the scarcity of stroke units, in fact our stroke unit in Hassan II Hospital University is the only one in Morocco. Difficulties in patient recognition of stroke symptoms, delays in seeking appropriate emergency care, delays in obtaining urgent brain imaging scan and also cost constraint, indeed the rt-PA is not covered by medical insurance in morocco are the others reasons [4]. The important delay to admission at hospital (120 minutes) compared with SITS delay (65 minutes) was explained by the fact that all patients are transported on their own: car, taxi, private ambulance. This is due to lack of organization providing such transportation [10]. The lack of prehospital organization and lack of people awareness about stroke are the most frequent explanation in developing countries. Compared with SITS-ISTR, mean time to door is about 55 min longer in our serie than in the cohort of patients treated within 3 hours of onset and 10 min under in the cohort of patients treated within 3 to 4.5 hours. The median time delay from hospital admission to initiation of treatment in our center was 10 minutes longer in the 3 hours cohort and 5 minutes under in the 3- to 4.5-hour cohort [10].
Before we started performing rt-PA, we performed a series of teaching courses, to educate physicians in local emergencies on the importance of early recognition and treatment of stroke patients. We educated radiologists and laboratory personnel in importance of early and fast work-up of stroke patients, and that patient represents a true neurological emergency. These teaching courses resulted in acceptable door to needle time in our hospital. Our future plans include providing more effective public education and working closely with paramedical personnel to shorten the time between the symptom onset and arrival to the emergency department. A Portuguese study found that the pre-hospital care account for 82% of the total delay of care. It is especially at this level that we must also act to guide the patient directly to the hospital [11]. The group of independent patients at 3 months is 39% in our series (20 cases) compared to 55% in all patients treated within 3 hours and within 3 to 4.5 hours in the SITS-ISTR (Figure 1).
Figure 1.
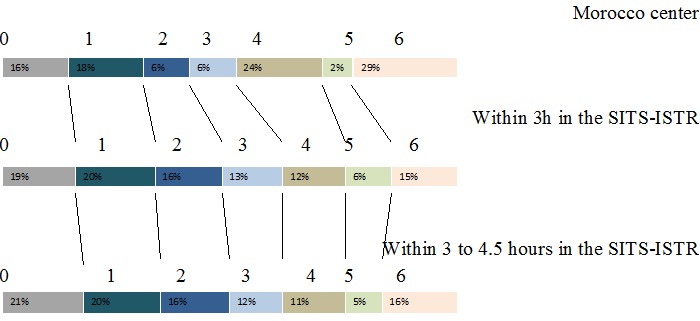
Comparison of mRS at 3 months between Moroccan patients, patients treated within 3–4.5 h and within 3 h in the SITS-ISTR
At the 3-month follow-up, only 21 patients (40%) were functionally independent (mRS ≤2). The death at 3 months in our study is significantly higher than in SITS-ISTR centers (29% compared to 16% for participants in 3 to 4.5 hours in the SITS-ISTR centers). The meta-analysis of Graham and Al. with 15 open studies (2639 patients) found a death rate of 13% [12]. The analysis of these results must take into account the initial NIHSS score is an average of 14 in our series compared with 09 in 3 to 4.5 hours cohort in the SITS-ISTR [10]. In addition, the percentage of patients with an initial thrombolysis NIHSS score less than 7 represents only 2% in our series. Another factor must also be taken into account in our context: the onset to treatment/needle time, thrombolysis patients in our series before 3 hours are only 26%, this explain the results very close to our center with 3 to 4.5hours cohort in the SITS-ISTR. Furthermore, the individual review of patient records included in the NINDS, ECASS I study and II, ATLANTIS (included patients until 6 assigns tests) showed that the positive effect in terms of deaths and dependence treatment was inversely correlated with the time of treatment after the onset of symptoms, noting that the risk-benefit ratio is favorable up to 4h 30 min [13]. In a 2009 Cochrane Systemic Review, symptomatic ICH was found in 7.7%, and death occurred in 16.5%, of the patients treated with thrombolysis [14]. Compared to the NINDS study and 2009 Cochrane data, a slightly lower symptomatic ICH and mortality rate were observed in our study. However, patients in the NINDS study were treated within three hours after the onset of stroke, which differed from our study. Patients with either symptomatic or asymptomatic ICH had less favorable outcomes and higher mortality rates compared to patients without ICH.
To improve our results, we must develop our multidisciplinary team of emergency physicians and nurses, radiologists, laboratory and paramedical personnel, and stroke neurologists for implementing the fast-track approach to providing thrombolysis. More rapid identification and evaluation in the emergency department, diagnosis, and initiation of treatment also could be responsible for the lower rate of SICH and better outcomes. Entry of the data for all our rt-PA-treated patients into the ongoing SITS multinational stroke registry (https://sitsinternational.org) is important initiative to ensure that our process and outcome measures in stroke thrombolysis are comparable to those in other international centers.
Conclusion
In, conclusion we have been able to show that IV thrombolysis feasible and safe in our hospital. This calls for a vigorous campaign among the public, health workers to develop other stroke unit.
What is known about this topic
Stroke is one of the leading causes of disability and death in both developing and developed countries;
The number of stroke patients receiving r-tPA in the developing world is extremely low;
The chief benefit of thrombolysis is improved final functional outcome through reperfusion salvage of threatened tissue.
What this study adds
The interest of this study is to bring our experience of 52 patients to encourage the realization of thrombolysis in Africa;
Increase the number of stroke units and the patients receiving r tPA in the developing countries;
Improving the management of ischemic stroke.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
All authors read and approved the final manuscript and have equally contributed to its content.
References
- 1.Strong K, Mathers C, Bonita R. Preventing stroke: saving lives around the world. Lancet Neurology. 2007 Feb;6(2):182–7. doi: 10.1016/S1474-4422(07)70031-5. [DOI] [PubMed] [Google Scholar]
- 2.Feigin VL, Lawes CM, Bennett DA, et al. Worldwide stroke incidence and early case fatality reported in 56 population-based studies: a systematic review. Lancet Neurology. 2009 Apr;8(4):355–69. doi: 10.1016/S1474-4422(09)70025-0. [DOI] [PubMed] [Google Scholar]
- 3.Engels T, Baglione Q, Audibert M, Viallefont A, Mourji F, El Alaoui Faris M. GRAVCM Study Group Socioeconomic status and stroke prevalence in Morocco: results from the Rabat-Casablanca study. PLoS One. 2014 Feb 28;9(2):e89271. doi: 10.1371/journal.pone.0089271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ghandehari K. Barriers of Thrombolysis therapy in developing Countries. Stroke Research and Treatment. 2011;2011:4. doi: 10.4061/2011/686797. (Article ID 686797) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Belkouch A, Jidane S, Chouaib N, Elbouti A, Nebhani T, Sirbou R, Bakkali H, Belyamani L. Thrombolysis for acute ischemic stroke by tenecteplase in the emergency department of a Moroccan hospital. The Pan African Medical Journal. 2015;21:37. doi: 10.11604/pamj.2015.21.37.6491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Adams HP, Jr, et al. Guidelines for Thrombolytic Therapy for Acute Stroke: a Supplement to the Guidelines for the Management of Patients with Acute Ischemic Stroke A Statement for Healthcare Professionals from a Special Writing Group of the Stroke Council, American Heart Association. Circulation. 1996 Sep 1;94(5):1167–74. doi: 10.1161/01.cir.94.5.1167. [DOI] [PubMed] [Google Scholar]
- 7.Barber PA, Demchuk AM, Zhang J, Buchan AM. For the ASPECTS Study Group: validity and reliability of a quantitative computed tomography score in predicting outcome of hyperacute stroke before thrombolytic therapy; Alberta Stroke Program Early CT Score. Lancet. 2000 May;355(9216):1670–74. doi: 10.1016/s0140-6736(00)02237-6. [DOI] [PubMed] [Google Scholar]
- 8.Bluhmki E, Chamorro A, Dávalos A, Machnig T, Sauce C, Wahlgren N, Wardlaw J, Hacke W. Stroke treatment with alteplase given 3.0-4.5 h after onset of acute ischaemic stroke (ECASS III): additional outcomes and subgroup analysis of a randomised controlled trial. Lancet Neurol. 2009 Dec;8(12):1095–102. doi: 10.1016/S1474-4422(09)70264-9. [DOI] [PubMed] [Google Scholar]
- 9.Wahlgren N, Ahmed N, Dávalos A, Ford GA, Grond M, Hacke W, Hennerici MG, Kaste M, Kuelkens S, Larrue V, Lees KR, Roine RO, Soinne L, Toni D, Vanhooren G SITS-MOST investigators. Thrombolysis with alteplase for acute ischaemic stroke in the Safe Implementation of Thrombolysis in Stroke-Monitoring Study (SITS-MOST): an observational study. Lancet. 2007 Jan 27;369(9558):275–82. doi: 10.1016/S0140-6736(07)60149-4. [DOI] [PubMed] [Google Scholar]
- 10.Niaz A, Lars K, Kennedy RL, Robert M, Turgut T, Danilo T. For the SITS Investigators Results of Intravenous Thrombolysis Within 4.5 to 6 Hours and Updated Results Within 3 to 4.5 Hours of Onset of Acute Ischemic Stroke Recorded in the Safe Implementation of Treatment in Stroke International Stroke Thrombolysis Register (SITS-ISTR): An observational study. JAMA Neurology. 2013 Jul;70(7):837–44. doi: 10.1001/jamaneurol.2013.406. [DOI] [PubMed] [Google Scholar]
- 11.National Institute of Neurological Disorders and Stroke rt-PA StrokeStudy Group. Tissue plasminogen activator for acute ischemic stroke. NEngl J Med. 1995;333:1581–87. [Google Scholar]
- 12.Graham GD. Tissue plasminogen activator for acute ischemic stroke in clinical practice: a meta-analysis of safety data. Stroke. 2003 Dec;34(12):2847–50. doi: 10.1161/01.STR.0000101752.23813.C3. [DOI] [PubMed] [Google Scholar]
- 13.Hacke W, Donnan G, Fieschi C, et al. Association of outcome with early strok treatment: pooled analysis of ATLANTIS, ECASS, and NINDS rt-PA stroke trials. Lancet. 2004;363:768–774. doi: 10.1016/S0140-6736(04)15692-4. [DOI] [PubMed] [Google Scholar]
- 14.Wardlaw JM, Murray V, Berge E, et al. Thromobolysis for acute ischemic stroke. Cochrane Database Syst Rev. 2009 Oct 7;4:CD000213. doi: 10.1002/14651858.CD000213.pub2. [DOI] [PubMed] [Google Scholar]


