Abstract
Blount's disease is commonly attributed to an intrinsic, idiopathic defect in the posteromedial proximal tibial physis resulting in progressive bowing of the leg, intoeing, and lateral knee thrust. Treatment has historically included bracing, physeal stapling, or corrective osteotomy, and was determined primarily by age at presentation. As we feel the pathology is not necessarily age dependent, we have elected to use the technique of guided growth using a lateral tension band plate to correct limb alignment as a first-line treatment in all patients presenting to our clinic as long as they had growth remaining and no evidence of a physeal bar.
We identified 17 patients with tibia vara (27 limbs) who were managed by means of guided growth of the proximal tibia, from age 1.8 years to 15.1 years. Clinical and radiographic parameters were followed pre- and postoperatively. The response to guided growth was documented as were any related complications.
Twenty-one (78%) limbs had complete normalization of their mechanical axis (middle 50% of knee). Time to correction averaged 13.5 months (8–19 months). There were no peri-operative complications. We observed hardware failure in 3 patients; 2 with screw breakage and 1 patient with hardware migration, none requiring subsequent osteotomy or further treatment. Two patients had rebound varus: one is being observed and another has undergone a repeat procedure.
Patients with pathologic tibia vara present at various ages and have historically undergone various treatments ranging from bracing to tibial osteotomy based on age at presentation. We have found that guided growth utilizing tethering plates can be used effectively as first-line treatment in all patients with growth remaining. This minimally invasive method is predictable and well tolerated. Recurrent deformity, though unlikely, is easily remedied by repeating the process and does not preclude osteotomy if eventually needed. Concomitant resolution of ligamentous laxity and inward torsion can be anticipated as the mechanical axis is restored to neutral. The only contraindications for guided growth include an unresectable physeal bar or skeletal maturity.
Keywords: blount disease, eight-plate, genu varum, hemiepiphysiodesis, tibia vara
1. Introduction
Blount's disease, also known as pathologic tibia vara, has proven to be a difficult condition to manage. Confusing the issue, is the treatment variability between the infantile (0–4 years), juvenile (4–10 years), and adolescent (>10 years) divisions of pathology.[11,27,28] Although presentation may vary among age groups, the risk of progressive bowing of the proximal tibia, with or without asymmetrical physeal closure, is universally problematic.
For the very young patient, some advocate conservative management with the utilization of bracing; yet the effectiveness of this approach remains controversial.[16,17,27,28] In the event bracing fails, the recommendation is generally a proximal tibial osteotomy, often achieving optimal results when the patient is 4 years of age or younger.[12–14,16,17,25] Osteotomies are technically challenging and carry many potential risks including nerve or vascular injuries, compartment syndrome, and infections.[14,16,23] Furthermore, there is a significant risk of recurrent varus following corrective osteotomy.[12–14,16]
For the older patient that develops pathologic tibia vara, bracing is not indicated. Surgical options generally include corrective high tibial osteotomy or hemiepiphysiodesis. For less severe deformities, hemiepiphysiodesis offers the advantage of a less invasive procedure with fewer major complications.[1,15,22–24] Several methods of hemiepiphysiodesis have been described including partial physeal ablation, physeal stapling, and more recently, tension-band plating.[1,5,15,19–24]
With the exception of those patients with a defined medial tibial physeal bar, we have taken the approach of initially managing all infantile, juvenile, and adolescent patients, presenting with pathologic tibia vara, with hemiepiphysiodesis using tension band plating without specific consideration for age or BMI (body mass index) as long as there is growth remaining. Our rationale is that there is no obvious difference in the underlying pathology, but only differences in patient age and body habitus at presentation. In reviewing these patients, our hypothesis was that guided growth with tethering plates is a safe and effective first line of treatment for skeletally immature patients regardless of age or BMI at presentation with the understanding that there is no definite physeal bar. Based on that hypothesis, the objective of this study was to review patients with pathologic tibia vara treated with hemiepiphysiodesis using tethering plates to establish efficacy in correcting deformity as well as to document complications associated with treatment.
2. Methods
This was an IRB approved, single institution, retrospective cohort study. Seventeen patients (27 limbs) were identified with a diagnosis of pathologic tibia vara and who were treated between 2004 and 2012 with temporary hemiepiphysiodesis using tension-band plating. All skeletally immature patients greater than 1 year of age who presented with pathologic tibia vara were included in the review. Failed prior treatment including osteotomy was not considered as exclusion criteria. Patients with metabolic and neurologic disorders, skeletal dysplasia, and previous trauma, were not considered for inclusion. All patients were followed in an outpatient setting by a single surgeon.
Full-length, weight-bearing, anterior–posterior radiographs of the lower extremities were evaluated for angular deformity, as well as proximal tibial and physeal morphology. The mechanical axis was evaluated by drawing a line from the center of the femoral head to the talus, bisecting the knee.[29] The knee was divided into 4 radiographic quadrants, varus designated as negative and valgus as positive. Normal variation falls within the central 2 quadrants (± zone 1). Genu varum was defined by medial deviation of the axis beyond the central 50% of the knee toward the joint margin (zone -2) or beyond (zone -3).[30] For the patient <4 years of age, Langenskiold changes of grade II or more along with progression of metaphyseal diaphyseal angle beyond 16 degrees verified a diagnosis of pathologic tibia vara.[26] For the older patient, progressive varus deformity of the proximal tibia with associated abnormalities of the proximal medial tibial physis confirmed the diagnosis. Other information collected from review of patient charts included sex, age at surgical intervention, and perioperative complications.
Guided growth using tethering plates has previously been described.[1] In young patients under 4 years, an arthrogram was often helpful for targeting the guide pins and screw placement (Fig. 1A–C). Immediate mobilization and full-length weight-bearing was encouraged after surgery. No casting or bracing was utilized postoperatively. Patients were subsequently evaluated in a clinical setting, typically at 3 to 4 month intervals, for tibia vara and tibial torsion. Full-length, weight-bearing, radiographs were acquired to allow for evaluation of mechanical axis deviation in relation to preoperative presentation. In all cases, the goal of treatment was to restore and maintain the mechanical axis within the central 50% (zone ± 1) of the knee, while preserving a horizontal joint line (Fig. 2A–C).[29] Once successful correction of leg alignment was attained, hardware was removed. It should be noted that we generally overcorrect to 3 to 5 degrees of genu valgus to allow for some physeal rebound following plate removal.
Figure 1.
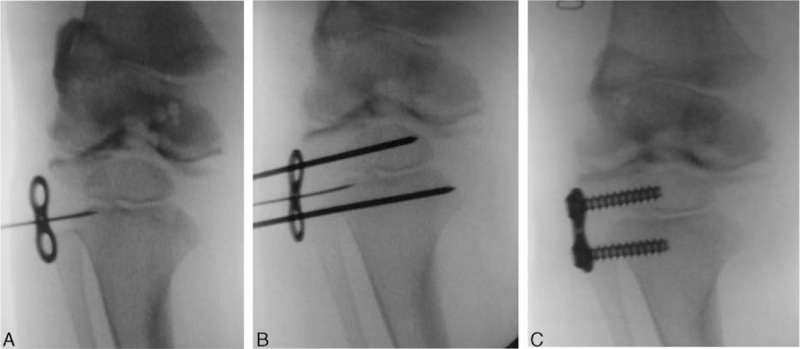
(A–C) Intraoperative placement of a tension band plate using fluoroscopy and an arthrogram.
Figure 2.
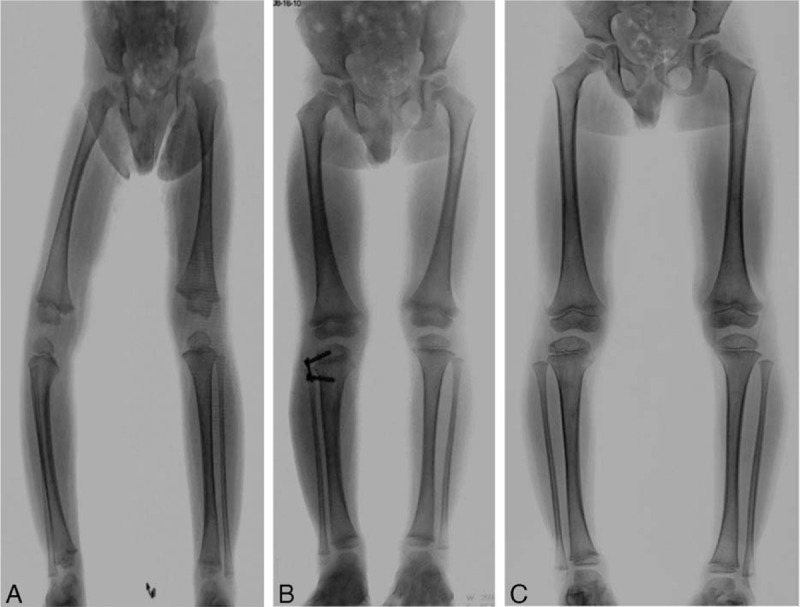
(A) Initial films revealing genu varum. (B) AP standing full length showing resolution of the genu varum after guided growth using an 8 plate. (C) AP standing full length after removal of hardware. AP = anteroposterior.
3. Results
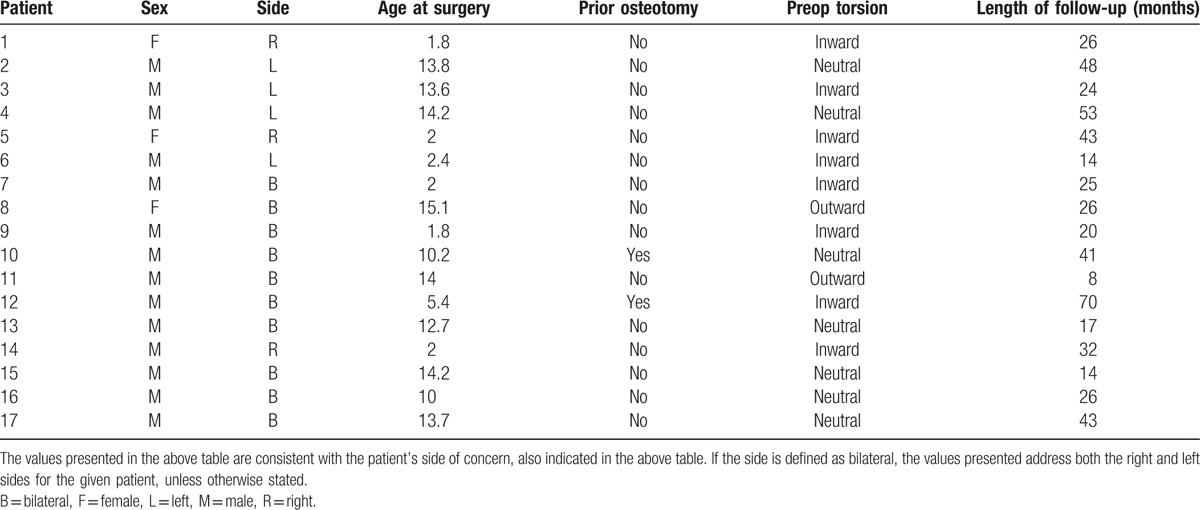
Pertinent patient demographic and preoperative data is listed in Table 1. Seventeen patients with 27 affected limbs underwent guided growth with tension-band plates. There were 14 boys and 3 girls, with ages ranging from 22 months to 14.2 years at the time of initial surgery.
Table 1.
Demographics.
The postoperative results are summarized in Table 2. Average follow-up from initial surgery date was 31 months (range 8 to 75 months). Of 27, 21 (78%) limbs had complete normalization of the mechanical axis (zone ±1). In patients with full correction, the average length of treatment from initiation to completion was 13.5 months (range 8–19 months) with none experiencing permanent growth arrest.
Table 2.
Results.
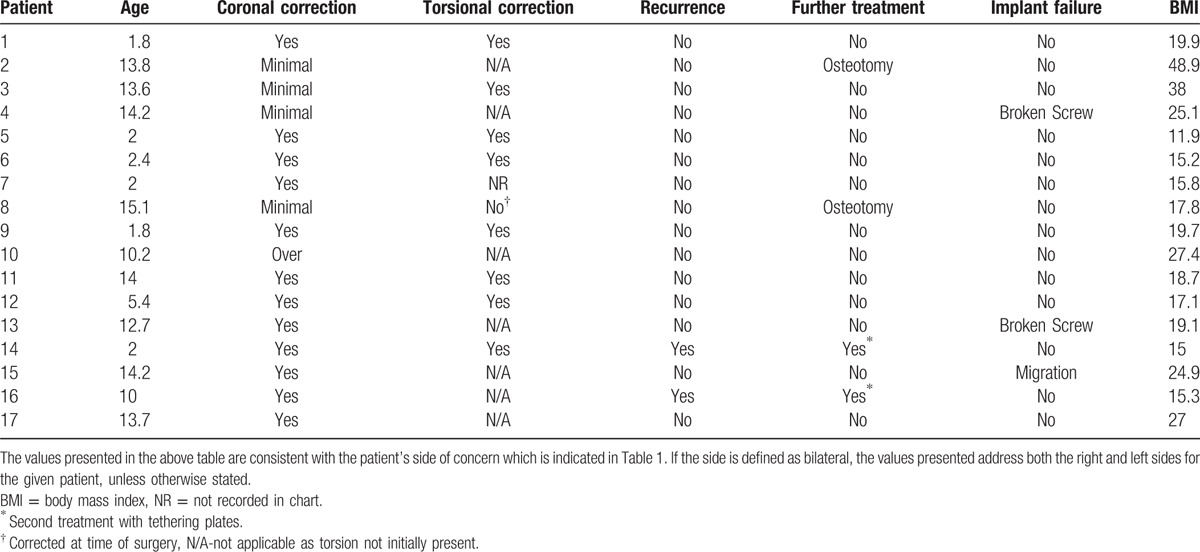
Five adolescent patients (6 limbs) had incomplete correction to a neutral mechanical axis. All of these patients were >13 years of age. Two of these patients are asymptomatic with a mild residual deformity and have required no further treatment. One of these patients received suggestion for an osteotomy to address a persistent moderate unilateral deformity but opted against further treatment. Two patients have undergone corrective osteotomies with good results.
Two of the patients selected for our study had previously undergone corrective osteotomies, using the Rab technique.[7] One patient was not initially followed at our institution and had undergone osteotomy prior to presentation with complete correction followed by subsequent recurrence. He was later treated at our institution with lateral tibial tension-band plating. This patient was lost to follow-up for 2 years after his tethering plates were placed. When he did return to clinic, he had overcorrected and his mechanical axis fell through the lateral border of his knee (zone 3+) requiring exchange of his hardware to the medial side of his tibia. He has subsequently corrected his mechanical alignment (Figure 3A–D). The second patient initially underwent an osteotomy of the left tibia for a severe deformity and right proximal tibial medial hemiepiphysiodesis for a mild right deformity. The osteotomy did not provide complete correction of the deformity. His residual deformity was treated with a hemiepiphysiodesis which later resulted in normalization of his mechanical alignment.
Figure 3.

(A) Reoccurrence of genu varum after osteotomy done at another institution. (B) Treated at our institution with lateral tibial tension-band plating. He was lost to follow-up after his tethering plates were placed. However, when he did return to clinic, he had overcorrected (lateral zone +2) (C). An exchange of his hardware to the medial side of his tibia resolved the genu valgum (D) at latest follow-up.
Ten of the 27 limbs (7 patients) had 15 to 30° of inward tibial torsion, determined by evaluation of the thigh-foot axis preoperatively. Each of these patients presented before the age of 6 years. Following tension-band plate application and correction of the varus angulation, the inward tibial torsion was noted to have spontaneously resolved. Although we do not have a good explanation of this phenomenon, it refutes the opinion held by many that osteotomy is required for correction of the inward rotational component that accompanies tibia vara in the younger patient.[23] Two of the 10 patients (4 limbs) over the age of 10 years had bilateral outward tibial torsion at presentation. One of the patients underwent bilateral inward rotational supramalleolar osteotomies at the time of tension-band plate application for tibia vara and went on to complete correction of both deformities. The second patient underwent only tension-band plate application for tibia vara. This patient eventually went on to have a multi-planar osteotomy with application of a spatial frame on the right side but had enough correction of the varus deformity on the left to require an isolated distal tibial rotational osteotomy to correct the excessive torsion.
None of the 17 patients experienced any immediate perioperative complications. However, 3 patients experienced hardware-related complications during treatment. Two patients had breakage of 1 or more of their screws including failure of a single metaphyseal screw in 1 patient and breakage of both the metaphyseal and epiphyseal screws in the other. The failures were noted at completion of correction in both patients and the hardware subsequently removed without further complication. Neither patient has had a recurrence of deformity. Interestingly, the third patient had migration of 1 screw through the physis. The reason for the migration is still unclear, but as with the screw failures, it was discovered at completion of treatment and simply removed with no evidence of further growth abnormality. Although these complications represent an implant failure rate of 15% (4 of 27 limbs), there appeared to be no significant consequence with respect to final outcome.
Two patients did experience some recurrence of deformity following completion of treatment. Both patients corrected at an average of 13.5 months, similar to the remainder of the group. The recurrences were noted at 6 and 26 months respectively, post implant removal. One deformity (now age 3 years) is very mild and as of yet, has not required further treatment. The other (now age 11 years) underwent reimplantation of the tension-band plate and has subsequently corrected his mechanical alignment.
One patient was lost to follow-up shortly after treatment. He was a 14-year-old male who failed to return to clinic after his lower extremity alignment had corrected and his hardware had been removed. While we do not know the current status of his lower leg alignment, we do know that he at least initially corrected. For this reason, we elected to leave this patient in the study as he did demonstrate success of initial correction.
4. Discussion
Tibia vara describes deformities resulting from a growth disturbance of the proximal tibial physis. The posteromedial aspect of the physis is primarily involved, with relative sparing of the lateral tibia and fibula.[2,3,11] This deformity can be accompanied by inward tibial torsion, (especially in younger patients),[23] lateral collateral ligament laxity, joint subluxation, and apparent shortening of the involved extremity. There may be associated ipsilateral varus (or occasionally valgus) of the distal femur.[4–10] As previously stated, the course of treatment for pathologic tibia vara has traditionally been based on the age of the patient and the surgeon preference.
In a previous report, Castañeda et al[19] condemned the use of hemiepiphysiodesis in adolescent Blount's disease, due to disappointing results in a series of 35 patients. It should be noted that their study evaluated the success of temporary and permanent hemiepiphysiodesis using techniques in existence prior to the advent of the tension-band plate. They suggested a lack of growth potential of the medial tibial physis as the underlying cause for failure. However, others have successfully corrected tibia vara by performing hemiepiphysiodesis of the proximal tibia employing the Blount staple and more recently, the tension-band plate.[1,5,15,20–24]
This study evaluated the efficacy of tension band hemiepiphysiodesis in skeletally immature patients with pathologic tibia vara without regard to patient age or body habitus as long as there was growth remaining. Overall success, when considering all patients, was 78% without any major complications. Although we had near or complete correction in only 62% (8 of 13 limbs) in patients over age the age of 12 using the tension-band plating, it is likely that all these patients would have required osteotomies had they not been treated with tension-band plating. As a consequence, we feel that this is a relatively safe and effective first-line treatment in this age group, especially given the potential complications associated with high tibial osteotomy.
Likewise, our patients under the age of 4 showed excellent response to treatment with tension-band plating. In this group of younger patients, all corrected with only 1 known recurrence. Again, without treatment, traditional management would have suggested osteotomy before the age of 4 in this patient population which could have resulted in up to 6 of these patients undergoing proximal tibial osteotomies. As of today, we have not had to perform corrective osteotomies in any of these younger patients.
As seen with tibial osteotomy, early intervention is preferred in order to prevent (or possibly even reverse) secondary issues such as ligamentous laxity, lateral subluxation, torsion, or recurrence of deformity. The theoretical risk of producing a permanent growth arrest or foreshortening the limb has not been an issue we have encountered. In the infantile patients, we noted spontaneous correction of inward tibial torsion and secondary rotational osteotomy was not required. The lateral collateral laxity and thrust also abated as the mechanical axis was restored to neutral. Thus, our experience would indicate that hemiepiphysiodesis may offer the delayed benefits of safe, gradual correction of malrotation and ligamentous laxity that occurs as the mechanical axis is restored to neutral.
Although the number of patients in this study was relatively small, it appears that there could be a correlation between Langerskiold classification and limits of correction. The problem here was that increasing age also appeared to correlate with incomplete correction. Thus, older patients with higher Langerskiold classifications were at highest risk incomplete correction. Patients with Langerskiold classifications less than V seemed to correct reliably as long as there was adequate growth remaining. Older patients were not corrected as reliably. This might suggest that age at initiation of correction was more important to the eventual outcome than severity of deformity assuming that a physeal bar was not present. To sort this out, larger numbers of patients would need to be studied so that the analysis could adequately control for age and Langerskiold classification.
Concerns have also been raised with regard to screw breakage associated with this application of the tension-band plate.[18,23] Some argue the patients and or their deformities are likely too large for a single screw, resulting in an unacceptably high rate of screw breakage. However, there has been no direct correlation drawn between BMI and hardware failure, nor a consistent pattern in relating failure with adolescent Blount's disease. In our series, there were only 3 incidents of screw breakage, all of which occurred near or at the end of treatment with no long-term adverse consequence. The reasons for the breakages were not entirely clear, but when reviewed carefully, it appears that the screws were widely divergent and may have impinged on the plate prematurely. As the screws splayed further apart with growth, the screws may have not been able to splay any further due to geometric constrains between the plate and screw resulting in eventual failure of the screw. This would suggest technical error likely explained the 3 failures we saw. However, because our incidence of hardware failure was low, and the consequence of failure minimal, we do not see this as a significant disadvantage in considering tension-band plating for the initial treatment of pathologic tibia vara even in the older or heavier patient.
There may have been other factors that could explain premature failure of screws. Some authors have addressed modification of technique, opting to defer pre-drilling the screw holes. We encourage at least pre-drilling the cortex, as a significant amount of torsional stress may be applied to the screws at insertion, possibly predisposing them to failure. Another plausible mode of failure may be related to the application of the plate itself. Radiographs of reported failures often reveal a gap between the distal end of the plate and the metaphyseal cortex, with the screw breaking at the entry point into the bone.[23] By not achieving coaptation of the plate to the bone, the exposed screw is subjected to a cantilever load and bending stresses for which it is not designed. The best means of preventing this scenario is to pre-bend the plate to better fit the contour of the lateral tibial metaphysis and to alternately tighten each screw in an effort to achieve better coaptation of the plate. Additional options for consideration could include 2 parallel plates, a single 4-hole plate and/or solid 4.5 mm screws.
We did see recurrence in 2 patients. Both patients were both younger in age (3 and 11 years). The first was only corrected to neutral, whereas the second was under-corrected by ∼2 degrees. These patients seemed to experience a period of asymmetric growth (lateral greater than medial) through the physis following removal of hardware which in turn resulted in a recurrence of varus alignment. When overcorrected by 3 to 5 degrees, we have not seen recurrence of pathologic varus alignment in our other patients. Though we feel it is possible children could have a recurrence following 3 to 5 degrees of overcorrection, we have not seen that happen as of yet. Additionally, younger age does not seem to be a reliable predictor of recurrence for this group of patients.
There were several limitations of this study. The most obvious included retrospective design and a small number of patients. Data collection was not uniform for every case as we did not find adequate clinical documentation of the pretreatment torsional profile in some of the patient charts. Finally, just under half of the patients were skeletally mature at follow-up suggesting that recurrence in the patients treated successfully could still be possible. However, as of this writing, we have seen continued maintenance of correction in all successfully treated patients aside from the 2 recurrences previously mentioned.
We suggest that hemiepiphysiodesis of the proximal tibia with tension-band plating affords the possibility of significant or complete correction for pathologic tibia vara in all pediatric patients having not yet reached skeletal maturity, and without the disadvantages and risks posed by more traditional high tibial osteotomy. Considering the known risks of staple migration and breakage, the tension-band plate technique offers the advantage of secure hardware fixation with less chance of device migration or failure. In the event of recurrence, even following an osteotomy, it is a technique that can be repeated provided there is not a definite physeal bar. In this series, 2 children (2 limbs) who originally had proximal tibial osteotomies with open physes later underwent subsequent tension-band plating to correct recurrent varus. We conclude that if the physis is open, osteotomy should be reserved as a salvage procedure in the event guided growth fails.
Until late 2004, staples were the only implant specifically available for hemiepiphysiodesis. The use of the nonrigid plate/screw construct as a tension band has expanded our indications and improved the outcome of guided growth and is an effective and safe first-line treatment in nearly all skeletally immature children with pathologic tibia vara.
Footnotes
Abbreviations: B = bilateral, BMI = body mass index, F = female, IRB = internal review board, L = left, M = male, R = right.
The authors have no funding and conflicts of interest to disclose.
References
- 1.Stevens PM. Guided growth for angular correction: a preliminary series using a tension band plate. J Pediatr Orthop 2007; 27:253–259. [DOI] [PubMed] [Google Scholar]
- 2.Cook SD, Lavernia CJ, Burke SW, et al. A biomechanical analysis of the etiology of tibia vara. J Pediatr Orthop 1983; 3:449–454. [DOI] [PubMed] [Google Scholar]
- 3.Stanitski DF, Stanitski CL, Trumble S. Depression of the medial tibial plateau in early-onset blount disease: myth or reality? J Pediatr Orthop 1999; 19:265–269. [DOI] [PubMed] [Google Scholar]
- 4.Bowen RE, Dorey FJ, Moseley CF. Relative tibial and femoral varus as a predictor of progression of varus deformities of the lower limbs in young children. J Pediatr Orthop 2002; 22:105–111. [PubMed] [Google Scholar]
- 5.Gordon JE, Heidenreich FP, Carpenter CJ, et al. Comprehensive treatment of late-onset tibia vara. J Bone Joint Surg Am 2005; 87:1561–1570. [DOI] [PubMed] [Google Scholar]
- 6.Gordon JE, King DJ, Luhmann SJ, et al. Femoral deformity in tibia vara. J Bone Joint Surg Am 2006; 88:380–386. [DOI] [PubMed] [Google Scholar]
- 7.Kline SC, Bostrum M, Griffin PP. Femoral varus: an important component in late-onset blount's disease. J Pediatr Orthop 1992; 12:197–206. [PubMed] [Google Scholar]
- 8.Myers TG, Fishman MK, Mccarthy JJ, et al. Incidence of distal femoral and distal tibial deformities in infantile and adolescent blount disease. J Pediatr Orthop 2005; 25:215–218. [DOI] [PubMed] [Google Scholar]
- 9.O’neill DA, Macewen GD. Early roentgenographic evaluation of bowlegged children. J Pediatr Orthop 1982; 2:547–553. [DOI] [PubMed] [Google Scholar]
- 10.Sabharwal S, Lee J, Zhao C. Multiplanar deformity analysis of untreated blount disease. J Pediatr Orthop 2007; 27:260–265. [DOI] [PubMed] [Google Scholar]
- 11.Brooks W, Gross R. Genu varum in children: diagnosis and treatment. J Am Acad Orthop Surg 1995; 3:326–335. [DOI] [PubMed] [Google Scholar]
- 12.Chotigavanichaya C, Salinas G, Green T, et al. Recurrence of varus deformity after proximal tibial osteotomy in blount disease: long-term follow-up. J Pediatr Orthop 2002; 22:638–641. [PubMed] [Google Scholar]
- 13.Doyle BS, Volk AG, Smith CF. Infantile blount disease: long-term follow-up of surgically treated patients at skeletal maturity. J Pediatr Orthop 1996; 16:469–476. [DOI] [PubMed] [Google Scholar]
- 14.Ferriter P, Shapiro F. Infantile tibia vara: factors affecting outcome following proximal tibial osteotomy. J Pediatr Orthop 1987; 7:1–7. [PubMed] [Google Scholar]
- 15.Henderson RC, Kemp GJ, Greene WB. Adolescent tibia vara: alternatives for operative treatment. J Bone Joint Surg Am 1992; 74:342–350. [PubMed] [Google Scholar]
- 16.Loder RT, Johnston CE. Infantile tibia vara. J Pediatr Orthop 1987; 7:639–646. [PubMed] [Google Scholar]
- 17.Schoenecker PL, Meade WC, Pierron RL, et al. Blount's disease: a retrospective review and recommendations for treatment. J Pediatr Orthop 1985; 5:181–186. [PubMed] [Google Scholar]
- 18.Burghardt RD, Specht SC, Herzenberg JE. Mechanical failures of eight-plate guided growth system for temporary hemiepiphysiodesis. J Pediatr Orthop 2010; 30:594–597. [DOI] [PubMed] [Google Scholar]
- 19.Castañeda P, Urquhart B, Sullivan E, et al. Hemiepiphysiodesis for the correction of angular deformity about the knee. J Pediatr Orthop 2008; 28:188–191. [DOI] [PubMed] [Google Scholar]
- 20.Mielke CH, Stevens PM. Hemiepiphyseal stapling for knee deformities in children younger than 10 years: a preliminary report. J Pediatr Orthop 1996; 16:423–429. [DOI] [PubMed] [Google Scholar]
- 21.Park S-S, Gordon JE, Luhmann SJ, et al. Outcome of hemiepiphyseal stapling for late-onset tibia vara. J Bone Joint Surg Am 2005; 87:2259–2266. [DOI] [PubMed] [Google Scholar]
- 22.Westberry DE, Davids JR, Pugh LI, et al. Tibia vara: results of hemiepiphyseodesis. J Pediatr Orthop B 2004; 13:374–378. [DOI] [PubMed] [Google Scholar]
- 23.Scott AC. Treatment of infantile Blount disease with lateral tension band plating. J Pediatr Orthop 2012; 32:29–34. [DOI] [PubMed] [Google Scholar]
- 24.McIntosh AL, Hanson CM, Rathjen KE. Treatment of adolescent tibia vara with hemiepiphysiodesis: risk factors for failure. J Bone Joint Surg Am 2009; 91:2873–2879. [DOI] [PubMed] [Google Scholar]
- 25.Li Y, Spencer SA, Hedequist D. Proximal tibial osteotomy and Taylor Spatial Frame application for correction of tibia vara in morbidly obese adolescents. J Pediatr Orthop 2013; 33:276–281. [DOI] [PubMed] [Google Scholar]
- 26.Levine AM, Drennan JC. Physiological bowing and tibia vara. The metaphyseal-diaphyseal angle in the measurement of bowleg deformities. J Bone Joint Surg Am 1982; 64:1158–1163. [PubMed] [Google Scholar]
- 27.Sabharwal S. Blount disease. J Bone Joint Surg Am 2009; 91:1758–1776. [DOI] [PubMed] [Google Scholar]
- 28.Bradway JK, Klassen RA, Peterson HA. Blount disease: a review of the English literature. J Pediatr Orthop 1987; 7:472–480. [PubMed] [Google Scholar]
- 29.Hsu RWW, Himeno S, Coventry MB, et al. Normal axial alignment of the lower extremity and load bearing distribution at the knee. Clin Orthop Rel Research 1990; 255:215–227. [PubMed] [Google Scholar]
- 30.Stevens PM, Maguire M, Dales MD, et al. Physeal stapling for idiopathic genu valgum. J Ped Orthop 1999; 19:645–649. [PubMed] [Google Scholar]


