Abstract
Objective
Coronary heart disease (CHD) is a major cause for mortality and morbidity in India but the focus on lifestyle interventions is very low. This study aims to evaluate the role of a multidisciplinary CHD prevention programme in southern India.
Methods
All patients enrolled between May 2014 and March 2016 with CHD (disease group) or with risk factors but no CHD (risk group) were included. Participants attended one–two sessions per week for 6–12 weeks; each session lasted 90–120 min, including exercise and education, and was adapted to the participants' sociocultural requirements. Resting heart rate, systolic and diastolic blood pressure, body mass index (BMI), waist circumference (WC) and functional capacity (FC) were documented at start and end of programme.
Results
Disease group was older (61±10 vs 51±14 years, p<0.01), had lower BMI and WC (26±4 vs 30±7 kg/m2, p<0.01; 39±4 vs 42±5 inches, p<0.01), attended more sessions (12±7 vs 6±3, p<0.0001) and had higher completion rates (82% vs 53%, p=0.02) than the risk group. Programme-completers (n=45, 67%) showed significant improvement in health-related behaviour, angina threshold (in all 8 subjects with stable angina), BMI (p=0.03), WC (p<0.01) and FC (p<0.01). Follow-up for a period of 16±6 months showed continued adherence to the healthy behaviour (n=44, 1 lost to follow-up) and maintenance of anthropometric and FC parameters.
Conclusions
A multidisciplinary approach to preventing CHD is lacking in India. This study shows that a comprehensive lifestyle intervention programme has significant benefits and can be incorporated in the routine management of all patients and at-risk individuals in the region.
Keywords: CORONARY ARTERY DISEASE
Introduction
Non-communicable diseases, particularly cardiovascular diseases (CVDs), are a global health burden and a growing threat to low and middle income countries (LMICs). The WHO recently reported that CVDs and diabetes are together responsible for 26% of all deaths in India and their incidence is steadily increasing each year.1 Coronary heart disease (CHD), the leading cause of cardiovascular mortality and morbidity, is taking a toll on lives irrespective of age, gender and socioeconomic strata and the implementation of effective prevention strategies is the need of the hour.2
A combination of behavioural and conventional risk factors such as abnormal lipids, hypertension, diabetes, obesity, physical inactivity, insufficient intake of fruits and vegetables, smoking, excessive alcohol intake and psychosocial factors account for most of the CHD cases in India, even among individuals below 60 years of age.3 4 While primordial prevention is key to curbing the CHD epidemic, risk-factor management by targeted pharmacotherapy and lifestyle intervention forms the cornerstone of prevention of CHD and its complications.5–7
The recent advances in coronary revascularisation techniques have clearly enhanced the outcome of acute coronary syndromes but there remains a lacuna in educating patients and their families on relevant issues such as CHD risk factors, health-related behaviour, cardiovascular drugs, and time expectations to resume normal physical, social, and sexual activities. Despite a strong message by key professional bodies to incorporate cardiac rehabilitation (CR) programmes in the secondary prevention of CHD in all eligible patients (class I recommendation),8 there is both a lack of CR services in India as well as a dearth of studies demonstrating its efficacy.9 This study aims to analyse the role of a multidisciplinary approach in the prevention of CHD in Chennai, a major metropolitan city in southern India.
Methods
Study subjects
The study cohort consisted of patients enrolled in the programme between May 2014 and March 2016 with established CHD (disease group) or with documented risk factors and no CHD (risk group). Patients with ischaemic heart disease, stable angina, compensated heart failure, and those with history of percutaneous coronary intervention (PCI) and coronary artery bypass graft (CABG) surgery were included, while patients with unstable angina, serious arrhythmias and uncontrolled heart failure were excluded. The procedures followed were in accordance with the ethical standards of the Indian Council of Medical Research and with the Declaration of Helsinki. Written informed consent was obtained from all patients at the time of enrolment. The study was approved by the ethical committee of our institute.
Clinical evaluation
A complete medical and family history was documented for all patients. Prior records of hospitalisation, investigations, medications, intervention and surgery were reviewed and relevant information noted. Resting heart rate, systolic blood pressure (SBP), diastolic blood pressure (DBP), body mass index (BMI), waist circumference (WC) and functional capacity (FC) were documented at baseline and at end-of-programme. Six-minute walk test (6MWT) was performed to assess the FC of participants and the 6 min walk distance (6MWD) was documented.10 Treadmill test (TMT) using the (modified) Bruce protocol was performed (RMS Vega 201 system) and the metabolic equivalents (METS) documented in participants who opted for this test. Target heart rate was calculated using the Karvonen formula, adjusting for β-blocker usage.
CHD risk factors were assessed as follows: already diagnosed with or currently under treatment for diabetes, hypertension and abnormal lipids, overweight/obesity (BMI>25 kg/m2 and/or WC >40 inches in men and >35 inches in women), inadequate physical activity (<150 min/week of aerobic exercise), insufficient intake of fruits and vegetables (<400 g/day of fruit and vegetable consumption), smoking (ex-smoker or current smoker of any form of tobacco), excessive alcohol consumption (history of binge drinking or habitual consumption of several drinks of alcohol) and presence of psychosocial factors (chronic stress, anxiety or depression). Verbal questioning and/or questionnaires were used to assess health-related behaviour. Metabolic syndrome was diagnosed based on the ATP III criteria.11
Programme design
A multidisciplinary team of healthcare professionals including a physician, physiotherapist, nutritionist and psychologist provided the programmes. The core components of the programme included exercise training, nutritional counselling, goal-setting to promote behaviour modification, psychosocial counselling, and education about risk factors, adherence to treatment, resuming normal activities and self-management. A typical centre-based programme (1–2 sessions per week for 6–12 weeks) was provided to patients living within 2 hours from the centre whereas the option of attending a modified programme with 1–2 sessions per month with more home-based components was offered for those with more than 2 hours travel time to the centre.
Each session consisted of an education/counselling component (30–40 min) and an exercise component (40–50 min), which included a warm-up period (7–10 min), an active exercise period (30–40 min, combination of treadmill walking, recumbent cycling, resistance exercises with free weights and theraband and floor exercises) and a cool-down period (7–10 min).
Based on the risk profile and personal preference of patients, they were provided group or individual exercise sessions. Rating of perceived exertion (Borg scale) and heart rate were used to assess cardiovascular response during exercise. The education/counselling sessions usually consisted of small groups (four to eight participants) in which the participants' family members were encouraged to participate.
An individualised programme was drafted for each participant upon enrolment with provision for rescheduling only in case of unavoidable absences. A record was maintained on attendance, session details and clinical progression. Adherence to the programme was considered good if a participant attended 50% or more of the planned sessions and poor if less than that. Baseline assessment was performed upon enrolment and end-of-programme evaluation upon completion of all planned sessions. A completion report outlining the nature and number of sessions attended and the outcomes was handed to the participants to share with their physicians.
Adaptations to suit patient population
The following adaptations were made to the programme to suit the sociocultural needs of our patient population:
First, as family members often provided care and support to individuals with heart disease, they were strongly encouraged to attend the education and counselling sessions. As women and elderly participants were typically accompanied by a family member, they were also routinely included in the interactive sessions.
Second, not all participants were comfortable wearing workout clothes. Hence, exercise sessions were made safe and convenient for participants wearing saree or dhoti, which are traditional southern Indian costumes. While mixed gender exercise groups were commonplace, women-only sessions were also provided based on participants' preference.
Third, nutritional counselling was adapted to the local cooking and eating habits. Some tactics employed were replacing a green leafy salad with ‘sundal’ (dried beans and pulses boiled and mixed with chopped raw onions, tomatoes, mangoes, cucumber, etc), encouraging iron-rich ingredients in everyday cooking like drumstick leaves, spinach, tofu, dates, dried fruits and nuts and encouraging whole wheat ‘rotis’ (Indian flat bread) and brown or parboiled rice.
Fourth, psychosocial counselling was aimed at addressing unresolved, longstanding and sensitive issues both at home and at work. For instance, issues arising out of strained relationships were dealt through additional focused sessions involving the participants and the concerned family members.
Statistical analysis
Categorical data are expressed as numbers (n) and percentages (%) and continuous data as mean and SD. Data were tested for normality and parametric and non-parametric statistics applied accordingly. χ2 test and unpaired t-test or Mann-Whitney test were used to compare categorical and continuous variables of the disease and risk groups at baseline, respectively. Baseline and end-of-programme characteristics were compared using paired t-test or Wilcoxon signed-rank test for normally distributed and non-normally distributed data, respectively. A p value <0.05 was considered statistically significant.
Results
Patient characteristics
The age of the subjects (n=67) was 56±13 years with the youngest a 16-year-old female and the oldest an 81-year-old male. There were 49 (73%) males. The demographic distribution of the study cohort is shown in table 1.
Table 1.
Demographic characteristics of the study subjects
| Demographic variable | Study subjects (n=67) |
|---|---|
| Age in years, n (%) | |
| <20 | 1 (1.5) |
| 20–39 | 5 (8) |
| 40–59 | 35 (52) |
| 60–79 | 25 (37) |
| >80 | 1 (1.5) |
| Marital status, n (%) | |
| Married | 59 (88) |
| Single | 3 (5) |
| Widowed | 5 (7) |
| Mother tongue, n (%) | |
| Tamil | 60 (90) |
| Telugu | 4 (6) |
| Kannada/Urdu/Punjabi | 3 (4) |
| Education, n (%) | |
| (Post)graduation | 42 (63) |
| School education | 21 (31) |
| Not attended school | 4 (6) |
| Employment, n (%) | |
| Working | 28 (25) |
| Retired | 25 (37) |
| Homemaker | 13 (19) |
| Student | 1 (1) |
| Travel time to reach centre, n (%) | |
| <2 hours | 50 (75)* |
| >2 hours, suburbs of city | 12 (18) |
| Out of city | 5 (7) |
*Three participants, a couple and another individual, from outside the city decided to stay in the city for the duration of the programme and are included in this group.
Vegetarians (n=18) and ovo-vegetarians (n=3) constituted 31% of the cohort. The disease group was older and had lower BMI and WC than the risk group (table 2).
Table 2.
Baseline clinical characteristics of the study subjects and differences between the two groups
| Characteristics | Study subjects (n=67) | Disease group (n=33) | Risk group (n=34) | p Value |
|---|---|---|---|---|
| Age, years (mean±SD) | 56±13 | 61±10 | 51±14 | 0.001 |
| Male, n (%) | 49 (73) | 28 (85) | 21 (62) | ns |
| Heart rate, bpm (mean±SD) | 77±12 | 75±11 | 80±13 | ns |
| SBP, mm Hg (mean±SD) | 133±17 | 133±17 | 134±17 | ns |
| DBP, mm Hg (mean±SD) | 78±9 | 76±8 | 79±9 | ns |
| BMI, kg/m2 (mean±SD) | 28±6 | 26±4 | 30±7 | 0.004 |
| WC, inches (mean±SD) | 40±5 | 39±4 | 42±5 | 0.0006 |
| Functional capacity | ||||
| 6MWD, metres (mean±SD) | 420±122 (n=56) | 420±124 (n=29) | 419±116 (n=27) | ns |
| TMT, METs (mean±SD) | 5±2 (n=11) | 5±2 (n=4) | 5±2 (n=7) | ns |
6MWD, 6 min walk distance; BMI, body mass index; DBP, diastolic blood pressure; METs, metabolic equivalents; ns, not significant; SBP, systolic blood pressure; TMT, treadmill test; WC, waist circumference.
Inadequate intake of fruits and vegetables was documented in 62 (92%) subjects, psychosocial risk factors in 59 (88%) subjects, insufficient physical activity in 53 (79%) subjects, hypertension in 47 (70%) subjects, overweight/obesity in 45 (67%) subjects, dyslipidaemia in 32 (48%) subjects, diabetes in 31 (46%) subjects, smoking in 9 (13%) and excessive alcohol consumption in 6 (9%) subjects. Metabolic syndrome was present in 23 (34%) subjects. Figure 1 shows the prevalence of the various risk factors in the two groups and figure 2 depicts the proportion of subjects with multiple risk factors.
Figure 1.
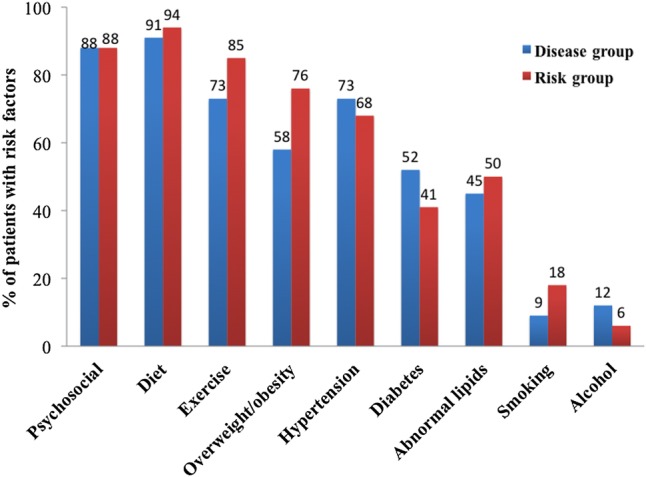
Prevalence of cardiovascular risk factors in the study subjects.
Figure 2.
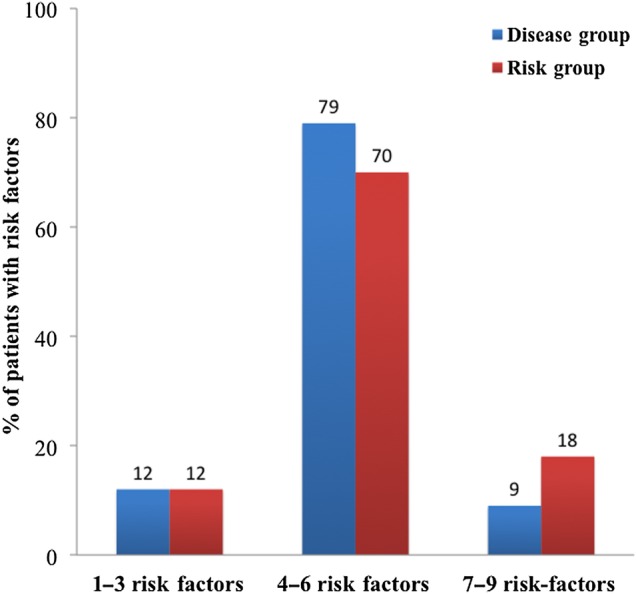
Grouping of subjects based on the number of cardiovascular risk factors harboured.
In the risk group (n=34), 29 (85%) subjects were treated for diabetes, hypertension and/or dyslipidaemia. Subjects presenting primarily for obesity management (n=5, 15%) were not on any therapy.
In the disease group (n=33), acute coronary syndrome was documented in 23 (70%) subjects among which 9%, 26% and 65% had single, double and triple vessel disease respectively. Apart from antidiabetic and antihypertensive medications, subjects were receiving a combination of antiplatelets, anticoagulants, statins and other lipid-lowering drugs, nitrates, β-blockers, and drugs that inhibit the renin–angiotensin system. Stable angina (Canadian Cardiovascular Society, grade II) was documented in eight (24%) subjects in this group. Left ventricular ejection fraction (LVEF) evaluated by echocardiogram prior to enrolment was below normal (36–49%) in seven (21%) subjects.
Time from CHD diagnosis to programme initiation was <2 years (5.7±6.7 months) in 21 subjects, 2–10 years (6.3± 2.7 years) in 8 subjects and >10 years (19.5±7.9 years) in 4 subjects. A history of revascularisation procedure was present in 10 (30%) subjects. PCI had been performed in 5 subjects; time from PCI to programme initiation was 18±21 months (range 1–51 months). CABG had been done in 5 subjects and time from CABG to start of programme was 12±6 years (range 3–21 years).
Programme characteristics
Tamil and English were the languages of instruction and all participants were fluent in one or both languages. A typical centre-based programme was attended by 60 subjects (89%) and a modified home-based programme by seven subjects (11%). A total of 30 (45%) subjects had a family member involved in the programme: 16 subjects had their spouse, parent or child enrolled in the programme and 14 subjects had a non-enrolled family member join most of the education/counselling sessions.
The subjects attended 606 exercise sessions (9±6 sessions per subject) and 545 education/counselling sessions (8±6 sessions per subject) during the study period. The topics covered pertained to risk factors of CHD and its management (2.2 sessions per subject), heart-healthy diet (2 per subject), exercise and its benefits (1.6 per subject), psychosocial issues (1.3 per subject) and goal-setting and group discussion (1 session per subject). Fifty-one subjects (76%) showed good adherence and 45 subjects (67%) completed the programme. Subjects in the disease group attended more sessions (12±7 vs 6±3, p<0.0001), had more participants attending 50% or more of the planned sessions (91% vs 62%, p<0.01) and had better completion rates (82% vs 53%, p=0.02) than the risk group.
Programme outcomes
End-of-programme evaluation was performed in all subjects who completed the programme (n=45). They had attended 503 (11±6) exercise sessions and 447 (10±6) education/counselling sessions over a period of 3±2 months. Improvement in exercise pattern, dietary behaviour and stress management was documented in all subjects. Angina threshold improved in all those (n=8) presenting with stable angina. There was a significant difference in BMI, WC and FC at the end of the programme (table 3).
Table 3.
Results of the programme in subjects who completed all planned sessions
| All (n=45) |
Disease group (n=27) |
Risk group (n=18) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Variable | Pre | Post | p Value | Pre | Post | p Value | Pre | Post | p Value |
| Heart rate, bpm (mean±SD) | 76±11 | 76±14 | ns | 74±11 | 73±11 | ns | 79±11 | 82±16 | ns |
| SBP, mm Hg (mean±SD) | 135±18 | 129±15 | ns | 132±17 | 126±12 | ns | 140±18 | 135±16 | ns |
| DBP, mm Hg (mean±SD) | 79±9 | 82±10 | ns | 77±9 | 79±9 | ns | 82±11 | 86±9 | ns |
| Weight, Kg (mean±SD) | 74±14 | 73±13.9 | 0.008 | 70±10 | 69±9 | ns | 79±18 | 79±18 | ns |
| BMI, kg/m2 (mean±SD) | 27.76±5.87 | 27.49±5.72 | 0.02 | 26.14±3.84 | 25.7±3.68 | 0.004 | 30.25±7.43 | 30.16±7.2 | ns |
| WC, inches (mean±SD) | 40±4 | 39±4 | 0.0 | 39±4 | 38±4 | 0.0 | 40±5 | 40±5 | 0.003 |
| 6MWD, metres (mean±SD) | 426±120 (n=37) | 489±132 (n=37) | 0.0002 | 411±124 (n=23) | 493±147 (n=23) | 0.001 | 448±112 (n=14) | 496±124 (n=14) | ns |
| TMT, METs (mean±SD) | 6±2 (n=6) | 8±2 (n=6) | 0.047 | 5±2 (n=3) | 8±3 (n=3) | ns | 7±2 (n=3) | 8±1 (n=3) | ns |
6MWD, 6 min walk distance; BMI, body mass index; DBP, diastolic blood pressure; METs, metabolic equivalents; ns, not significant; SBP, systolic blood pressure; TMT, treadmill test; WC, waist circumference.
Improvement in FC was assessed using 6MWT in 37 subjects and TMT in 6 subjects; change in FC could not be assessed in two subjects. The 6MWT appears to be a simple, efficient and reliable tool for assessing patients in an outpatient preventive cardiology setting. All the participants who completed the programme gave positive feedback about the various components of the programme and felt that the programme adequately complemented their routine medical management. No injuries, accidents or acute cardiac events occurred during the exercise sessions.
Of the 22 participants who failed to complete the programme, 6 subjects belonged to the disease group and 16 to the risk group. Three participants in the disease group had completed >90% of planned sessions but due to unexpected travel abroad in one subject, sudden change in family circumstances in one and development of unstable angina requiring CABG in one subject, did not attend the end-of-programme evaluation; other reasons were long commute time in two subjects and job transfer out of state in one subject.
Busy work life (n=6), long commute time (n=5), unexpected circumstances in the family (n=2), chronic untreated depression (n=2) and non-coronary death (n=1) were the primary reasons for non-completion in the risk group.
Follow-up
After programme completion (n=45), centre-based follow-up was done in 20 (44%) subjects and phone follow-up was carried out in 24 (53%) subjects as they could not visit the centre. One subject (2%) was lost to follow-up. The total follow-up period from end of programme was 16±6 months. Two patients with reduced LVEF succumbed to heart failure 8 and 16 months after programme completion, respectively. Time interval from programme completion to first centre-based follow-up was 5.7± 5 months; anthropometric measurements and FC did not differ from end-of-programme values.
Discussion
This study reports the outcomes of a comprehensive exercise-cum-education programme for the prevention and rehabilitation of CHD in India. While a multidisciplinary approach to CHD prevention is yet to gain momentum in the country, this study highlights the fact that a CR programme tailored to the sociocultural, psychological and linguistic needs of patients is an effective and valuable addition to the existing armamentarium. The outcomes of the programme, namely positive changes in health-related behaviours and significant improvement in angina threshold, anthropometrics and FC, demonstrate that multidisciplinary programmes work well in South Asians and should be incorporated in the primary and secondary prevention strategies.
The drop-out rate in CR programmes is reported to be around 20–40% globally as well as in India.12–14 In this study, which included patients with established CHD as well as at-risk patients, 76% of the participants showed good adherence to the programme and 67% completed the programme. Several studies originating from English-speaking countries have reported on the relatively lower levels of participation of South Asians in CR programmes.15 The programme reported here was designed based on established international guidelines and modified to suit the local population. The adaptations made to the exercise, education and counselling sessions made it possible for the patients to participate in the programme with ease. The study by Rajendran et al13 had reported improvement in FC, anthropometrics and blood metabolites after a 3-month CR programme in CABG patients from southern India. The main difference between that study and the present one is that the latter employed a structured exercise-cum-education programme with the participants attending more sessions over a similar time period. This is also the first study, to our knowledge, focusing on both primary and secondary prevention of CHD in India. While cardiopulmonary exercise testing is the gold-standard in FC assessment, the TMT and the 6MWT are used interchangeably for the same purpose in outpatient CR settings.16 The use of the TMT was limited especially in female participants and the elderly in this study, while the 6MWT proved to be a simple and reliable tool.
Follow-up over a period of 16±6 months showed that most of the participants who completed the programme were adherent to the healthy lifestyle behaviours adopted during the programme. This was confirmed by the anthropometric and FC measures that did not differ significantly from the end-of-programme values.
This being the only programme of this kind at the time of this study for prevention of CHD in the state of Tamil Nadu, with a population of close to 70 million, it is not surprising that difficult access was the prime barrier for programme completion. Also, individuals with fewer risk factors and a busy work-life had a tendency to drop out, which together with the lesser number of sessions attended, possibly accounts for the lack of significant improvement in the risk group. Digital media and telemonitoring, which have shown some promise in improving adherence to prevention programmes,17 might be effective in delivering sessions and monitoring adherence in low-risk patients in the Indian setting. This however needs to be confirmed. In our neighbours China and Pakistan too, there seems to be a paucity of CR programmes in large medical centres and attendance rates are suboptimal due to lack of easy access.18 19 And it has also become clear that less than 40% of the world's countries have an established CR programme in spite of the overall improvement in medical and surgical treatment modalities.20
Last but not the least, patients themselves have to pay for the programmes due to lack of medical insurance coverage and government aid for such preventive services. This is one of the major differences between CR programmes in LMICs and that in higher income countries. While there is some evidence to show cost-effectiveness of exercise-based CR in the latter group,21 the common model for delivering CR services based on 36 sessions of supervised, exercise-based outpatient rehabilitation, faces major cost and access challenges in LMICs.22 The most plausible solution appears to be shorter secondary prevention programmes, those based in a general practice set-up, and those staffed by generalists as proposed by Clark et al23 and as implemented in this study. The benefits of such a prevention programme, not only to the affected individuals and their families but also to the society and the nation at large, should be studied in detail through large-scale medical research efforts, which in turn could help convince policymakers and insurance companies to include it in their healthcare plans. Thus, in short, we believe that just like developed countries, growing economies also need a patient-centred, multidisciplinary secondary prevention programme for CHD, delivered through locally acceptable, easily accessible and cost-effective formats.24 25
Strengths and limitations
The observational design of the study together with the associated selection bias, small sample size, lack of controls and relatively short follow-up are limiting factors that might have influenced the study outcomes. Despite the limitations, the outcomes of the study are promising and provide for a working model of a multidisciplinary CHD prevention programme for India and neighbouring countries. The authors plan to conduct a prospective multicentre study involving tertiary hospitals in India to validate the study findings and to follow the participants on an ongoing basis to assess the long-term impact of the programme.
Conclusions
India is in the brink of a cardiovascular disease epidemic and the current treatment modalities, namely pharmacotherapy and revascularisation techniques, are not poised to reverse this trend on their own. A multidisciplinary approach to prevention that is based on international guidelines but sensitive to the needs of the local population appears to be a valuable addition to the current strategy to improve the cardiovascular health of the nation.
Key messages.
What is already known about this subject?
A multidisciplinary approach has been proven effective and has been incorporated in the routine management of patients with coronary heart disease in many developed countries. There is both a lack of awareness and a dearth of facilities providing such services in India and other Asian countries, where the mortality and morbidity due to the disease is rapidly rising.
What this study adds?
This study highlights the fact that a multidisciplinary programme tailored to the sociocultural, psychological and linguistic needs of the target population is well attended, has good outcomes and is an effective addition to the existing treatment modalities of coronary heart disease.
How might this impact on clinical practice?
This study will enlighten healthcare professionals about the benefits of systematic lifestyle interventions including supervised exercise, nutritional guidance and psychosocial counselling in the primary, secondary and tertiary prevention of coronary heart disease in India, thereby encouraging referral to and an increase in availability of such services.
Footnotes
Contributors: All the authors have made substantial contributions to the study. PC contributed to conception and design of study, acquisition of data, drafting the manuscript, final approval of the manuscript and accountable for all aspects of the work; NSV contributed to design of the study, acquisition and analysis of data, revising the manuscript for important intellectual content, final approval of the manuscript and accountable for all aspects of the work; NEV contributed to design of the study, acquisition and analysis of data, revising the manuscript for important intellectual content, final approval of the manuscript and accountable for all aspects of the work; VC contributed to conception of study, revising the manuscript for important intellectual content, final approval of the manuscript and accountable for all aspects of the work.
Competing interests: None declared.
Ethics approval: Cardiac Wellness Institute's ethics committee.
Provenance and peer review: Not commissioned; internally peer reviewed.
References
- 1.World Health Organization—Noncommunicable Diseases (NCD) Country Profiles. http://www.who.int/nmh/countries/ind_en.pdf, June 2016.
- 2.Shah B, Mathur P. Surveillance of cardiovascular disease risk factors in India: the need & scope. Indian J Med Res 2010;132:634–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yusuf S, Hawken S, Ounpuu S et al. , INTERHEART Study Investigators. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet 2004;364:937–52. doi:10.1016/S0140-6736(04)17018-9 [DOI] [PubMed] [Google Scholar]
- 4.Joshi P, Islam S, Pais P et al. . Risk factors for early myocardial infarction in South Asians compared with individuals in other countries. JAMA 2007;297:286–94. doi:10.1001/jama.297.3.286 [DOI] [PubMed] [Google Scholar]
- 5.Chomistek AK, Chiuve SE, Eliassen AH et al. . Healthy lifestyle in the primordial prevention of cardiovascular disease among young women. J Am Coll Cardiol 2015;65:43–51. doi:10.1016/j.jacc.2014.10.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eckel RH, Jakicic JM, Ard JD et al. . 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014;129:S76–99. doi:10.1161/01.cir.0000437740.48606.d1 [DOI] [PubMed] [Google Scholar]
- 7.Corrà U, Piepoli MF, Carré F et al. . Secondary prevention through cardiac rehabilitation: physical activity counselling and exercise training: key components of the position paper from the Cardiac Rehabilitation Section of the European Association of Cardiovascular Prevention and Rehabilitation. Eur Heart J 2010;31:1967–74. doi:10.1093/eurheartj/ehq236 [DOI] [PubMed] [Google Scholar]
- 8.Smith SC Jr, Benjamin EJ, Bonow RO et al. . AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation endorsed by the World Heart Federation and the Preventive Cardiovascular Nurses Association. J Am Coll Cardiol 2011;58:2432–46. doi:10.1016/j.jacc.2011.10.824 [DOI] [PubMed] [Google Scholar]
- 9.Madan K, Babu AS, Contractor A et al. . Cardiac rehabilitation in India. Prog Cardiovasc Dis 2014;56:543–50. doi:10.1016/j.pcad.2013.11.001 [DOI] [PubMed] [Google Scholar]
- 10.ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med 2002;166:111–7. doi:10.1164/ajrccm.166.1.at1102 [DOI] [PubMed] [Google Scholar]
- 11.https://www.nhlbi.nih.gov/files/docs/guidelines/atglance.pdf. June 2016.
- 12.Heran BS, Chen JM, Ebrahim S et al. . Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev 2011;(7):CD001800 doi:10.1002/14651858.CD001800.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rajendran AJ, Manoj S, Karthikeyan D et al. . Cardiac rehabilitation for CABG patients in South Indian setup: a prospective study. IJPMR 2004;15:23–33. [Google Scholar]
- 14.Babu AS, Maiya AG, George MM et al. . Effects of combined early in-patient cardiac rehabilitation and structured home-based program on function among patients with congestive heart failure: a randomized controlled trial. Heart Views 2011;12:99–103. doi:10.4103/1995-705X.95064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Galdas PM, Ratner PA, Oliffe JL. A narrative review of South Asian patients’ experiences of cardiac rehabilitation. J Clin Nurs 2011;21:149–59. doi:10.1111/j.1365-2702.2011.03754.x [DOI] [PubMed] [Google Scholar]
- 16.Bellet RN, Adams L, Morris NR. The 6-minute walk test in outpatient cardiac rehabilitation: validity, reliability and responsiveness-a systematic review. Physiotherapy 2012;98:277–86. doi:10.1016/j.physio.2011.11.003 [DOI] [PubMed] [Google Scholar]
- 17.Kraal JJ, Peek N, Van den Akker-Van Marle ME et al. . Effects of home-based training with telemonitoring guidance in low to moderate risk patients entering cardiac rehabilitation: short-term results of the FIT@Home study. Eur J Prev Cardiol 2014;21:26–3. doi:10.1177/2047487314552606 [DOI] [PubMed] [Google Scholar]
- 18.Zhang Z, Pack Q, Squires RW et al. . Availability and characteristics of cardiac rehabilitation programmes in China. Heart Asia 2016;8:9–12. doi:10.1136/heartasia-2016-010758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ali M, Qadir F, Javed S et al. . Factors affecting outpatient cardiac rehabilitation attendance after acute myocardial infarction and coronary revascularization—a local experience. J Pak Med Assoc 2012;62:347–51. [PubMed] [Google Scholar]
- 20.Turk-Adawi K, Sarrafzadegan N, Grace SL. Global availability of cardiac rehabilitation. Nat Rev Cardiol 2014;11:586–96. doi:10.1038/nrcardio.2014.98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Anderson L, Oldridge N, Thompson DR et al. . Exercise-based cardiac rehabilitation for coronary heart disease: Cochrane systematic review and meta-analysis. J Am Coll Cardiol 2016;67:1–12. doi:10.1016/j.jacc.2015.10.044 [DOI] [PubMed] [Google Scholar]
- 22.Oldridge NB, Pakosh MT, Thomas RJ. Cardiac rehabilitation in low- and middle-income countries: a review on cost and cost-effectiveness. Int Health 2016;8:77–82. doi:10.1093/inthealth/ihv047 [DOI] [PubMed] [Google Scholar]
- 23.Clark AM, Hartling L, Vandermeer B et al. . Secondary prevention programmes for coronary heart disease: a meta-regression showing the merits of shorter, generalist, primary care-based interventions. Eur J Cardiovasc Prev Rehabil 2007;14:538–46. doi:10.1097/HJR.0b013e328013f11a [DOI] [PubMed] [Google Scholar]
- 24.Grace SL, Turk-Adawi KI, Contractor A et al. . Cardiac rehabilitation delivery model for low-resource settings. Heart 2016;102:1449–55. doi:10.1136/heartjnl-2015-309209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sandesara PB, Lambert CT, Gordon NF et al. . Cardiac rehabilitation and risk reduction: time to “rebrand and reinvigorate”. J Am Coll Cardiol 2015;65:389–95. doi:10.1016/j.jacc.2014.10.059 [DOI] [PubMed] [Google Scholar]


