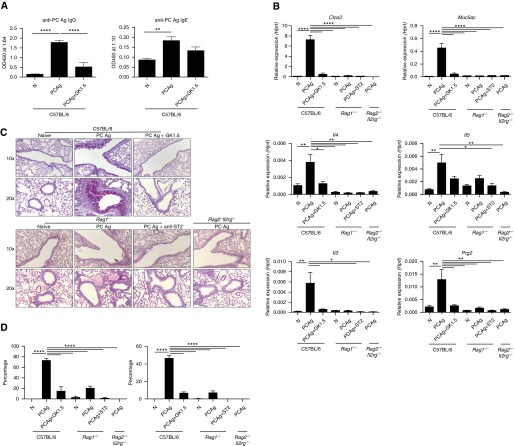
Figure 5.
CD4+ T cells, but not type II innate lymphoid (ILC2) cells, are the primary effectors of Pneumocystis antigen (PCAg)–driven pathology. C57BL/6 mice (n = 6 per group) were untreated, treated with PCAg, or treated with both PCAg and GK1.5 monoclonal antibody and killed at Day 14. Data represent the combination of two independent experiments. Naive Rag1−/− mice (n = 3), Rag1−/− mice treated with PCAg (n = 3), Rag1−/− mice treated with anti-ST2 antibody and PCAg (n = 4), and Rag2−/−Il2rg−/− mice treated with PCAg (n = 3) were also analyzed. (A) Anti-Pneumocystis (anti-PC) antibody production (IgG and IgE) is dependent on CD4+ T cells. (B) Expression of type II immune response genes in whole-lung homogenate at Day 14 appears to be mediated by CD4+ T cells but not ILC2 cells. (C) Periodic acid–Schiff staining of whole lung shows that CD4+ T cells drive the mucus response to PCAg, while limited ILC2-dependent mucus production was noted in Rag1−/− mice. (D) PCAg treatment significantly increased the percentage of total airways affected by mucus (left) and the area of individual airway periodic acid–Schiff–positive staining (right) in a CD4-dependent manner (*P < 0.05, **P < 0.01, and ****P < 0.0001 by one-way analysis of variance with Tukey’s multiple comparisons). Hprt = hypoxanthine phosphoribosyltransferase; OD450 = optical density at 450 nm.