Abstract
Introduction
Neonatal outcomes can be directly and indirectly affected by caesarean delivery (CD). Data on CD rates in semi-urban and rural hospitals in resource-limited settings are scarce and yet are needed to better guide the care of women and neonates in these settings. we carried out this study to determine the frequency of CD, its indications and the frequency of the various adverse neonatal outcomes (ANO) in the Limbe Regional Hospital (LRH) and the Buea Regional Hospital (BRH), Cameroon. We also assessed the relationship between the indication for CD and ANO in the said hospitals.
Methods
This was a hospital-based retrospective and prospective cross-sectional study using descriptive and analytic methods conducted in the LRH and the BRH maternity units within a nine months period in 2015. Informed consent was obtainedfrom mothers of the neonates. Data analyses were performed using Epi-Info 3.5.4 software.
Results
We recruited 199 neonates born through CD. The prevalence of CD was 13.3% with cephalopelvic disproportion (CPD) being the most frequent (32.2%) indication for CD. There were 52 (26.1%) ANO following CD and respiratory distress was the most common 24 (46.2%) of all ANO. Emergency indications for CD were associated with more ANO 49 (34.5%) as compared to elective indications for CD 3 (5.3%) [p-value<0.001]. We noted a significant association between indications for CD and the various type of ANO, with CPD having the worse prognostic neonatal outcomes 30.8% [p-value=0.02].
Conclusion
The prevalence of ANO associated with CD in our hospitals was high with a worrying prognosis. While the exact reasons are unknown, the creation of well-equipped neonatal units with trained staff, may contribute to reduce neonatal morbidity and fatalities. Furthermore, the association of CPD to worse prognostic neonatal outcomes calls for clinicians, to consider additional management options, such as antibiotic prophylaxis and oxygen therapy to the neonates, prior to CD.
Keywords: Caesarean delivery, adverse neonatal outcome, prevalence, resource-limited settings
Introduction
Worldwide rise in caesarean delivery (CD) rates during the last three decades has been a cause of alarm [1]. The rates of such delivery have increased dramatically in recent years, from 12% in 1990 to 24% in 2008 with no improvement in outcome for neonates [2]. The increasing rates of CD have been debated globally for over two decades, especially during the 1980s, when a peak was reached in industrialized Countries [3]. This lead to guidelines from the relevant United Nations (UN) agencies for CD rates in a country, it stated that; CD rates should be between 5% and 15% [4, 5] and further research on the issue was warranted.
In 2002, more than one-fourth of all births (26.1%) in United States were by CD, the highest ever reported rate [6]. In 2004, rate of births from CD, for first pregnancies increased to 29.1% of all births, continuing a rising trend [6], with labour dystocia, previous CD, breech presentation and fetal distress being the most common indications of CD amongst others. Babies born via caesarean delivery face more risks than babies born vaginally: they are more likely to have respiratory problems in the neonatal period, more likely to have difficulties establishing breastfeeding, and more likely to experience asthma in childhood and adulthood [7]. Babies delivered after a general anaesthesia have lower Apgar scores than those delivered after spinal anaesthesia [2]. Torkanetal [8], showed that, there is a higher incidence of low Apgar scores, need for resuscitations, birth injury, pulmonary hypertension and respiratory distress amongst neonates born through CD. Worldwide trends towards increased CD rates have also been observed in Africa. The rate of CD in a teaching hospital in Nigeria rose from 7.2% in 2000 to 11.8% in 2009 [9]. Furthermore, the course of increased CD rates has also been noted in Cameroon. The rate of CD in Cameroon varies between 2% and 3% of all deliveries, with higher rates reported for the main teaching hospital (CHU) in Yaoundé, and for the Central Hospital Yaoundé [10]. Also, in a study carried out by Forsah [11], in Buea, Cameroon the CD rate was 23.8%. Amongst the indications of CD; fetal distress, labour dystocia, breech presentation, multiple gestation and previous CD being the most common indications.
A study by Tebeuet al [12], found the poor foetal outcome of foetus delivered through CD in the Far North Region of Cameroon and revealed that one of three caesarean deliveries ended in foetal death. Furthermore Forsah [11], in Buea had a 14.4% Adverse Neonatal Outcome (ANO) following indication for CD. These ANO included respiratory distress, neonatal infections and neonatal death. Data on CD rates and their outcomes guide obstetricians and pediatricians in the management of pregnancy and it outcomes. Unfortunately, such data are rare for semi-urban areas in developing countries. We thus carried out this study to determine the frequency of CD, its indication and the frequency of the various adverse neonatal outcomes (ANO) in the Limbe and Buea Regional Hospitals, two second-level referral hospitals in semi-urban Cameroon. We also assessed the relationship between the indication for CD and ANO in the said hospitals.
Methods
Study design and setting
A hospital-based retrospective and prospective study using descriptive and analytic methods was carried out in the Limbé and Buea regional hospitals. These health facilities are located in the South West Region of Cameroon and serves as a second-level referral level maternities in the South West Region. About 160 deliveries are conducted each month amongst which are caesarean deliveries. The maternity units have a total of 50 beds. Both hospitals have qualified and experienced staffs: 5 Doctors (obstetrician/gynecologist, pediatrician), 4 Midwife, 10 Nurses and Birth attendants
Study population, sampling and study procedures
The study population was made of pregnant women who had delivered by CD and their neonates. A purposive sampling method was used. Any pregnant woman delivered by CD in the LRH and the BRH admitted in the hospitals maternity during the study period were eligible to take part for the prospective phase, while for the retrospective phase, delivery files were reviewed and only files with completed data (that is files with basic demographic and identification data, gestational age, type and indication for CD, and basic clinical examination of neonate) were used. The retrospective phase covered files from July 2015 to December 2015. For the prospective phase we used purposive sampling technique to approach and seek consent from eligible participants admitted in the hospital maternity using a consent form. Questionnaires were presented to those who consented to participate. Record(s) of participants involved in the study were reviewed and the following outcomes amongst neonates born by CD were recorded: the presence or not of respiratory distress, diagnosed based on Silverman-Anderson retraction score (i.e. a score >6) or Downes' Score (i.e. a score>6) [13]; neonatal infection diagnosed based on fever (temperature instability), poor feeding, seizures (seizure was graded using the Blantyre coma scale (i.e. a grade ≤4) [14]); birth injuries diagnosed based on joint dislocation, bone fracture, laceration [15]; the degree of resuscitation based on APGAR score at 1and 5 minute (i.e. a score<6) resuscitation with prolong ventilation (i.e> 5 minutes) [16]; and neonatal death based on brain death guides by Wijdicks [17].
Data management and data analysis
Data were collected and detailed recording of the types of CD, indications for CD and neonatal outcomes was done. To minimize errors from handling and filling the data sheet, one copy of the data sheet for each patient was filled on hard copy and another was keyed into the EPI info 3.5.4 database in the investigator's computer. 10% of entered questionnaires were double checked. Data were analyzed using Epi-Info 3.5.4 software. Numeric results were presented to the nearest two decimal places. Descriptive statistics (age, gestational age, place of delivery, marital status, type of delivery, type of anaesthesia, gender of neonates, neonatal outcomes, APGAR score, ANO and birth weight) were presented using absolute numbers, means and percentages. Proportions of outcome variables within categories of predictor variables were computed and compared using the Chi- square or Fisher's exact statistical tests where appropriate. Two-tailed p-values ≤ 0.05 were considered statistically significant.
Ethical Considerations
Administrative approvals were obtained from the South West Regional Delegation of Public Health, the BRH and the LRH. Ethical approval was obtained from the Institutional Review Board of the Faculty of Health Sciences, University of Buea, Cameroon. Written informed consent was obtained from all mothers (caretaker) of the neonates who were enrolled in the prospective phase of the study while a waiver of consent was granted for the retrospective phase of the study by the Institutional Review Board, as it would have been impossible to conduct the study if consent was to be sought from participants but the patient records/information was anonymized and de-identified prior to analysis. To reduce the inconvenience to neonates, clinical examination of neonates were done using standard sterile and temperature-controlled conditions
Results
Of the 1492 deliveries conducted during the study period, 199 were caesarean, giving an overall CD rate of 13.3% (Figure 1). The characteristics of the 199 women and their neonates included in this study and the outcomes of CDs are summarized in Table 1, Table 2. Most of our participants (58%) were in the age range between 25-34 years, majority (70%) had gestational age ranges between 38-41 weeks, 67% delivered in the BRH. As many as 83% of CDs were done under General anesthesia, and 71% were emergency CDs. Cephalo-pelvic disproportion (CPD) was the most frequent (32.2%) indication for CD (Figure 2). Also, of the 199 neonates born, 52 (26.1%) had at least one adverse neonatal outcomes (ANO), with respiratory distress being the most frequent (46.2%) ANO (Figure 3). Table 3 shows the association between the indications for CD and the various types of ANO. There was a statistical significant relationship between ANO and indication for CD, p-value=0.02 using Fisher's exact test (Table 3). Also, ANO were significantly more frequent following emergency CDs compared to elective CDs, p-value=<0.001 using Chi-square test (Table 4).
Figure 1.
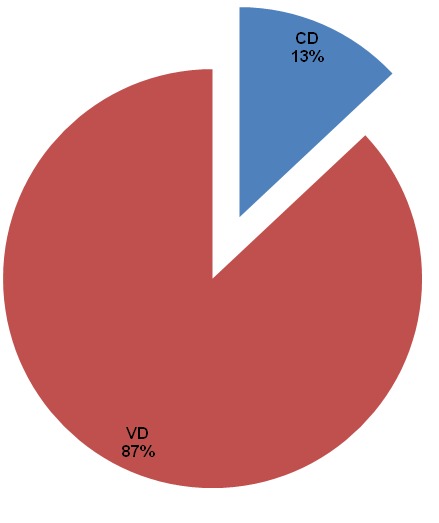
Route of delivery of 1492 neonates in the Limbe and Buea regional hospitals, Cameroon. (CD: Caesarean delivery; VD: vaginal delivery)
Table 1.
Characteristics of 199 women and neonates included in a study of Caesarean delivery in the Limbe and Buea regional hospital, Cameroon
| Characteristic | Level | n | % |
|---|---|---|---|
| Age (years) | 15-24 | 67 | 34 |
| 25-34 | 116 | 58 | |
| 35-44 | 8 | 16 | |
| Marital status | Married | 144 | 72 |
| Single | 55 | 28 | |
| Gestatiionalage (weeks) | 30-33 | 8 | 4 |
| 34-37 | 32 | 16 | |
| 38-41 | 139 | 70 | |
| 42 | 20 | 10 | |
| Place of delivery | LRH | 65 | 33 |
| BRH | 134 | 67 | |
| Gender of neonate | Male | 114 | 57 |
| Female | 85 | 43 | |
| Type of anaesthesia | General anaesthesia | 166 | 83 |
| Spinal anaesthesia | 33 | 17 |
Table 2.
Characteristics of 199 caesarean deliveries and their outcomes in the Limbe and Buea regional hospital, Cameroon
| Characteristic | Level | n | % |
|---|---|---|---|
| Type of CD | Emergency | 142 | 71 |
| Elective | 57 | 29 | |
| Outcome of CD | Favourable | 147 | 74 |
| ANO | 52 | 26 | |
| Types of ANO | Respiratorydistress | 24 | 46.2 |
| Neonataldeath | 15 | 28.8 | |
| Infection | 8 | 15.4 | |
| Resuscitation | 4 | 7.7 | |
| Birthinjury | 1 | 1.9 |
Figure 2.
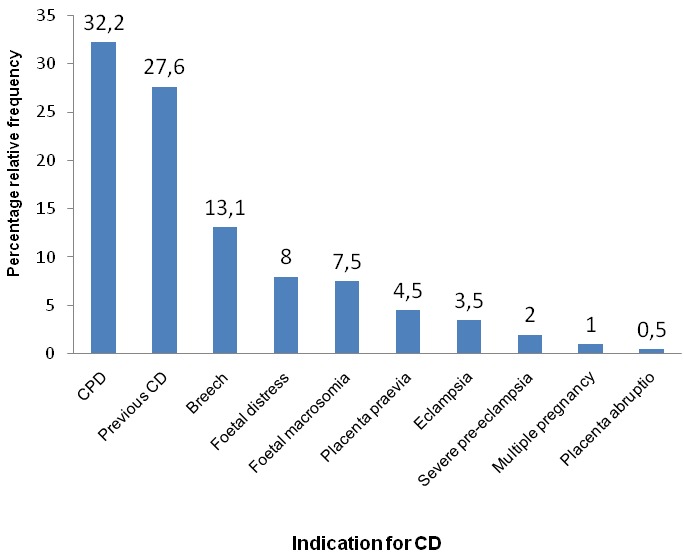
Frequency of indications for caesarean delivery amongst 199 studied participant in the Limbé and Buea regional hospitals, Cameroon
Figure 3.
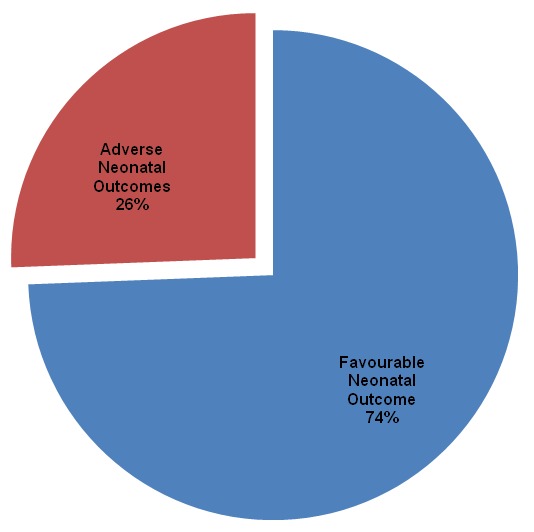
Overall neonatal outcomes following caesarean delivery in the Limbé and Buea regional hospitals, Cameroon
Table 3.
Association between indications for Caesarean Delivery and the various types of ANO
| TYPES OF ADVERSE NEONATAL OUTCOME | |||||||
|---|---|---|---|---|---|---|---|
| Indication for CD | RD n(%) | n(%) ND | Infection n(%) | RE n(%) | BI n(%) | TOTAL n(%) | P value |
| CPD | 6(25.0) | 6(40.0) | 2(25.0) | 2(50.0) | 0(0.0) | 16(30.8) | |
| Foetal Distress | 5(20.8) | 2(13.3) | 1(12.5) | 2(50.0) | 0 (0.0) | 10(19.2) | |
| Previous CD | 5(20.8) | 1(6.7) | 2(25.0) | 0(0.0) | 0(0.0) | 8(15.4) | |
| Breech | 0(0.0) | 2(13.3) | 2(25.0) | 0(0.0) | 0(0.0) | 4(7.7) | |
| FoetalMacrosomia | 2(8.3) | 1(6.7) | 0(0.0) | 0(0.0) | 1(100) | 4(7.7) | |
| Placenta Praevia | 2(8.3) | 2(13.3) | 0(0.0) | 0(0.0) | 0(0.0) | 4(7.7) | |
| Eclampsia | 2(8.3) | 0(0.0) | 1(12.5) | 0(0.0) | 0(0.0) | 3(5.8) | |
| Severe Pre-eclampsia | 1(4.2) | 1(6.7) | 0(0.0) | 0(0.0) | 0(0.0) | 2(3.8) | |
| Multiple Pregnancy | 1(4.2) | 0(0.0) | 0(0.0) | 0(0.0) | 0(0.0) | 1(1.9) | |
| Placenta Abruptio | 0(0.0) | 0(0.0) | 0(0.0) | 0(0.0) | 0(0.0) | 0(0.0) | |
| TOTAL | 24(100) | 15(100) | 8(100) | 4(100) | 1(100) | 52(100) | 0.02 |
RD=Respiratory Distress, ND=Neonatal Death, BI=Birth Injury, RE= Some Degree of Resuscitation
Table 4.
Association between adverse neonatal outcomes and types of CD
| Adverse Neonatal Outcome | ||||
|---|---|---|---|---|
| Type of CD | YES (%) | NO (%) | TOTAL | P-VALUE |
| Emergency | 49 (34.5) | 94 (65.5) | 142 | |
| Elective | 3 (5.3) | 54 (94.7) | 57 | |
| Total | 52 (26.1) | 147 (73.9) | 199 | <0.001 |
Discussion
In this study, we had a prevalence for caesarean delivery (CD) within expected ranges. Cephalopelvic disproportion (CPD) was the most common indication for CD. Furthermore we noted a high prevalence of adverse neonatal outcomes(ANO)with respiratory distress being the most frequent adverse neonatal outcome. There was also a significant association between indications for CD and the various types of ANO. The prevalence of CD was 13.3%. This prevalence falls in the range of 10 -15% as proposed by World Health Organisation (WHO) for the worldwide CD rate [18] and within ranges as reported in other studies [9, 19], the rate is however, lower than the rate observed in the study conducted by Forsah in Buea [11] and in other studies [20–33]. Doctors within our hospitals may be conscious of the WHO proposal that there is no justification for any region to have a CD rates higher than 10-15%, [18, 34, 35]. Also, much awareness is being made to ensure that the ranges of worldwide rate of CD as proposed by WHO [18], is met in SWR. Variation in studies could be attributed to multiple factors including: Maternal demands for the procedure, pressure of obstetrician favouring recourse to CD, changes in size of the population, socioeconomic factors and the limited use of vaginal instrumental delivery.
CPD was the most frequent indication for CD (32.2%). This findings correlates with that made by Forsah in Buea, Cameroon [11], Nana et al [36] in the Far-North region of Cameroon and Sugewe [31] in Yaoundé, Cameroon. It is also consistent with findings in many other studies out of Cameroon [9, 20, 23, 24, 33, 37–40]. The high frequency of CPD as indication was in contrast with reports of a previous CD being the most common indication in studies by Aziz et al in Pakistan [21] and Bangalet al in India [22]. In our study previous CD was only the third indication suggesting that obstetricians in our setting may not necessarily be adhering to the dictum that 'once a CD always a CD' [41, 42].
In this study, nearly one in every five neonates born through CD had an Adverse Neonatal Outcome (ANO). This correlates with findings made by Forsah in Buea, Cameroon [11] and Tebeuet alin Northern Cameroon [12]. This could be because most of the caesarean deliveries were done as emergencies, the relatively frequent use of general anesthesia and the lack of Neonatal Intensive Care Unit (NICU). Other studies have reported that increased use of general anesthesia in CDs was associated with increased ANO [2, 43–45]. Furthermore, in a study carried out by Nana et al in the Far-North Region of Cameroon, revealed that emergency indication for CD was associated with high ANO [36]. The absence of paediatricians and neonatologists may contribute to these high rates of ANO Respiratory Distress was the most common ANO identified (>30%). This is consistent with findings in other studies [19, 38, 46, 47]. On the other hand, in studies conducted by Allison in Australia [48] and Tebeuet al in Northern Cameroon [12], neonatal death (which is the second most frequent ANO in our study) was the most common ANO. This variation could be related to the different indications for CD: In the study by Allison in Australia [48] breech presentation was the most frequent indication for CD while “extreme ages of reproductive life” was the most frequent indication noted by Tebeuet al in Northern Cameroon [12].
In this study, there was an association between the types of CD and ANO. We observed more ANO (34.5%) with Emergency indications for CD. Similar findings were observed by Forsah and Tebeuet al in Cameroon [11, 12] and Zanardoet al in Italy [49]. The high rates of ANO could be due to the exigencies of the emergency indication for CD. There was also a significant association between the indications for CD and the various types of ANO with CPD emerging with the most (30.8%) types of ANO (infection, neonatal death, respiratory distress, degree of resuscitation), closely followed by foetal distress (19.2%), with similar ANO. It is also, worth noting that, placenta abruptio, had no risk for ANO, closely followed by; multiple pregnancy with 1(1.9%) ANO (Respiratory distress). This could be related to the high prevalence of CPD (32.2%) and low prevalence of multiple pregnancy (1%) and placenta abruptio (0.5%) observed in our study.
This study was limited to just two hospitals within Cameroon. Nevertheless result from our study are similar to those of other previous studies [9, 18, 19, 23, 33, 38, 39, 49]. Also, we limited this study to the short term outcomes following CDs. Future studies will need to assess the long term outcomes of CD in our milieu. Furthermore, other studies will need to compare the frequencies of adverse outcomes between neonates born via caesarean and neonates born via the vaginal route.
Conclusion
This study has shown that, the prevalence of CD (13.3%) is within the range acceptable toWHO, with CPD being the most frequent (32.2%) indication for CD. Moreover, at least one in every five neonates born through CD had an ANO with respiratory distress being the most frequent ANO. Furthermore, there was a significant association between indications for CD and the various types of ANO. CD for CPD had the worse prognosis of ANO. The CD rate combined with the high rates of adverse outcomes is a call for concern. Health personnel will need to be made aware and trained on the management of neonates born of CDs in this setting. The training ought to also reinforce the need for close monitoring of labour, through the appropriate use of a partogramme. This also allow for early detection of the need for a CD Furthermore, the technical capabilities of health facilities will need to be re-enforced to foster neonatal care.
What is known about this topic
The rate of CD;
Indications of CD.
What this study adds
At least one in every five neonates born through CD had an ANO;
A significant association between indications for CD and the various types of ANO;
CD for CPD had the worse prognosis of ANO.
Acknowledgments
We thank all study participants. We also, thank Mr and Mrs Tanyi for funding this project.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
TJT, JA, conceived the research questions, TJT designed the study protocol and collected data; TJT analyzed data. JA and KNP assisted with data interpretation. JA, TR, and PNF all assisted with study design and implementation. All authors wrote and or reviewed the manuscript.
References
- 1.Mukherjee SN. Rising caesarean section rate. In J Obstet Gynecol. 2006;4(56):298–300. [Google Scholar]
- 2.Lopes T, Spirtos N, Naik R, Monaghan J. 11th ed. Blackwell Publishing Ltd; 2010. Bonney's Gynaecological Surgery. [Google Scholar]
- 3.XII World Congress of Gynecology and Obstetrics, Rio de Janeiro, October 1988. Pregnancy and labor. Vol. 5. London: Parthenon Publishing Group; 1989. Advances.ingynecology and obstetrics. [Google Scholar]
- 4.UNICEF/WHO/UNFPA, (1997) Guidelines for monitoring the availability and use of obstetric services. New York: United Nations Population Fund; 1999. [Google Scholar]
- 5.UNDP/UNFPA/WHO/World Bank Special Programme of Research (2008) Highlights of achievements, 1990-2001. 124. Vol. 14. Geneva: World Health Organization, Department of Reproductive Health and Research, Family and Community Health; 2008. pp. 470–83. [Google Scholar]
- 6.Zelop C, Heffner LJ. The downside of cesarean delivery: short and long term complications. In J Obstet Gynecol. 2004;47(8):386–93. doi: 10.1097/00003081-200406000-00012. [DOI] [PubMed] [Google Scholar]
- 7.Boley JP. The history of cesarean section. Can Med Assoc J. 1991;145(4):319–22. [PMC free article] [PubMed] [Google Scholar]
- 8.Torkan B, Parsay S, Lamyian M, Kazemnejad A, Montazeri A. Postnatal quality of life in women after normal vaginal delivery and caesarean section. BMC Preg Childbirth. 2009;9(6):4. doi: 10.1186/1471-2393-9-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Geidam AD, Audu BM, Kawuwa BM, Obed JY. Rising trend and indications of caesarean section at the university of Maiduguri teaching hospital, Nigeria. Ann Afr Med. 2009;8(2):127–32. doi: 10.4103/1596-3519.56242. [DOI] [PubMed] [Google Scholar]
- 10.Diallo FB, Diallo MS, Bangoura S, Diallo AB, Camara Y. Cèsarienne, facteur derèduction de morbiditè etde mortalitèfoeto-maternelle au Centre Hospitalier UniversitaireIgnace Deen de Conakry (Guinée) Méd d'Afrique Noire. 1998;45(6):123–28. [Google Scholar]
- 11.Forsah SF. Unpublished MD thesis, Faculty of Health Sciences. Cameroon: University of Buea, Buea; 2012. Rates, Indications and Complications of Caesarean Deliveries: The case of Buea Regional Hospital. [Google Scholar]
- 12.Tebeu PM, Ngassa P, Mboudou E, Kongnyuy EJ, Binam F, Obama MT. Neonatal survival following cesarean delivery in northern Cameroon. Int J Gynaecol Obstet. 2008;103(3):259–60. doi: 10.1016/j.ijgo.2008.07.001. [DOI] [PubMed] [Google Scholar]
- 13.Pickrell K. An inquiry into the history of cesarean section. Bull Soc Med Hist (Chicago) 1935;4(56):414–53. [Google Scholar]
- 14.Molyneux ME, Borgstein A, Taylor TE, Wirima JJ. Clinical features and prognostic indicators in paediatric cerebral malaria: a study of 131 comatose Malawian children. Q J Med. 1989;71(265):441–59. [PubMed] [Google Scholar]
- 15.Alexander JM, Leveno KJ, Hauth J, Landon MB, Thom E, Spong CY, et al. National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Obstet Gynecol. 2006;108(4):885–90. [Google Scholar]
- 16.American Academy of Pediatrics. Committee on Fetus and Newborn, American College of Obstetricians and Gynecologists and Committee on Obstetric Practice. J Paediatr. 2006;117(22):1444–47. [Google Scholar]
- 17.Wijdicks EF. The diagnosis of brain death. NEJM. 2001;344(16):1215–21. doi: 10.1056/NEJM200104193441606. [DOI] [PubMed] [Google Scholar]
- 18.World Health Organisation. Appropriate technology for birth. Lancet. 1985;2(8452):436–7. [PubMed] [Google Scholar]
- 19.Toril K, Ola DS, Anne KD, Stein TN, Pal Planned cesarean versus planned vaginal delivery at term: comparison of newborn infant outcomes. Am J Obstet Gynecol. 2006;195(6):1538–43. doi: 10.1016/j.ajog.2006.05.005. [DOI] [PubMed] [Google Scholar]
- 20.Adekanle DA, Adeyemi AS, Fasanu AO. Caesarean section at a tertiary institution in Southwestern Nigeria: a 6-year audit. OJOG. 2013;3(20):357–61. [Google Scholar]
- 21.Aziz N, Yousfani S, Soomro I. Rising trend and indications of caesarean section at the Liaquat university of medical & health sciences. Quarterly Medical Channel. 2011;17(4):55–59. [Google Scholar]
- 22.Bangal VB, Thorat PS, Patel NH, Borawake SK. Caesarean sections-are we doing right? IJBR. 2012;3(4):281–84. [Google Scholar]
- 23.Furau C, Furau G, Dascau V, Ciobanu G, Onel C, Stanescu C. Improvements in cesarean section techniques: arad's obstetrics department experience on adapting the vejnovic cesarean section technique. MAEDICA J Clinic Med. 2013;8(3):256–60. [PMC free article] [PubMed] [Google Scholar]
- 24.Igberase GO, Ebeigbe PN, Andrew BO. High caesarean section rate: a ten year experience in a tertiary hospital in the Niger delta, Nigeria. Nigerian J Clinic Practice. 2009;12(3):294–97. [PubMed] [Google Scholar]
- 25.Inyang-Etoh EC, Etuk SJ. Demographic and obstetric determinants of emergency caesarean section among women in Calabar, Nigeria. Glo Res J Med Sci. 2013;3(7):20–24. [Google Scholar]
- 26.Kamath BD, Todd JK, Glazner JE, Lezotte D, Lynch AM. Neonatal outcomes after elective caesarean delivery. Obstet Gyncol. 2009;113(6):1231–8. doi: 10.1097/AOG.0b013e3181a66d57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lee HC, Gould JB, Boscardin WJ, El-Sayed YY, Blumenfeld YJ. Trends in cesarean delivery for twin births in the United States. Obstet Gynecol. 2011;118(5):1095–101. doi: 10.1097/AOG.0b013e3182318651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liston FA, Allen VM, O'Connell CM, Jangaard KA. Neonatal outcomes with caesarean delivery at term. Arch Dis Child Fetal Neonatal Ed. 2008;93(3):176–82. doi: 10.1136/adc.2006.112565. [DOI] [PubMed] [Google Scholar]
- 29.Mahmut K. The Delivery methods and the factors affecting among giving birth in hospitals in Yozgat, Turkey. Int J Caring Sci. 2012;5(2):157–61. [Google Scholar]
- 30.Ojiyi EE, Dike EI, Anolue F, Chukwulebe A. Appraisal of caesarean section at the Imo State University Teaching Hospital, Orlu, Southeastern Nigeria. Int J Obstet Gynecol. 2012;16(2):2. [Google Scholar]
- 31.Sugewe DE. Evolution des indications de césarienne à la maternité du CHU de Yaoundé sur une période de 10 ans (1990-1999), Unpublished MD thesis, Faculty of Medicine and Biomedical Sciences. Cameroon: University of Yaounde I, Yaounde; 2000. [Google Scholar]
- 32.Souza JP, Gülmezoglu AM, Lumbiganon P, Laopaiboon M, Carroli G, Fawole B, et al. Caesarean section without medical indications is associated with an increased risk of adverse short-term maternal outcomes: the 2004-2008 WHO Global Survey on Maternal and Perinatal Health. BMC Med. 2010;8(10):71. doi: 10.1186/1741-7015-8-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Teguete I, Traore Y, Sissoko A, Djire MY, Thera A, Dolo T, et al. Determining factors of cesarean delivery trends in developing countries: lessons from Point G National Hospital (Bamako - Mali. Tech Cesarean Delivery. 2012;200(9):162–200. [Google Scholar]
- 34.Villar J, Valladares E, Wojdyla D, Zavaleta N, Carroli G, Velazco A, et al. Caesarean delivery rates and pregnancy outcomes: the 2005 WHO global survey on maternal and perinatal health in Latin America. Lancet. 2006;367(9525):1819–29. doi: 10.1016/S0140-6736(06)68704-7. [DOI] [PubMed] [Google Scholar]
- 35.Althabe F, Sosa C, Belizán JM, Gibbons L, Jacquerioz F, Bergel E. Cesarean section rates and maternal and neonatal mortality in low, medium and high income countries: an ecological study. Birth. 2006;33(4):270–7. doi: 10.1111/j.1523-536X.2006.00118.x. [DOI] [PubMed] [Google Scholar]
- 36.Nana PN, Djenabou A, Fomulu JN, Mbu RE, Tonye R, Wandji JC, et al. Epidemio-clinical factors associated with caesarean delivery in two referral hospitals (Public/Faith-Based), Far-North Region, Cameroon. Clin Mother Child Health. 2011;8(2):1–5. [Google Scholar]
- 37.Doh AS. A clinical study of caesarean section at the University Teaching Hospital (CHU) Yaounde (1982-1989) Cent Afr J Med. 1991;37(10):326–28. [PubMed] [Google Scholar]
- 38.Olusanya OB, Solanke O. Maternal and neonatal factors associated with mode of delivery under a universal newborn hearing screening programme in Lagos, Nigeria. BMC Preg Childbirth. 2009;9(6):41. doi: 10.1186/1471-2393-9-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Onsrud L, Onsrud M. Increasing use of cesarean section, even in developing countries. Tidsskr Nor Laegeforen. 1996;116(1):67–71. [PubMed] [Google Scholar]
- 40.Roosmalen JV, Does V. Caesarean birth rates worldwide: a search for determinants. Trop Geogr Med. 1995;47(1):19–22. [PubMed] [Google Scholar]
- 41.Cragin EB. Conservatism in obstetrics. NY Med J. 1916;104(2):1–3. [Google Scholar]
- 42.Flamm BL. Once a cesarean, always a controversy. Obstet Gynecol. 1997;90(8):312–15. doi: 10.1016/S0029-7844(97)00263-9. [DOI] [PubMed] [Google Scholar]
- 43.Reynolds F, Seed PT. Anaesthesia for caesarean section and neonatal acid-base status: a meta-analysis. Anaesth. 2005;60(4):636–53. doi: 10.1111/j.1365-2044.2005.04223.x. [DOI] [PubMed] [Google Scholar]
- 44.Gordon A, McKechnie EJ, Jeffery H. Pediatric presence at cesarean section: justified or not? Am J Obstet Gynecol. 2005;193(3 pt 1):599–605. doi: 10.1016/j.ajog.2005.06.013. [DOI] [PubMed] [Google Scholar]
- 45.Algert CS, Bowen JR, Giles WB, Knoblanche GE, Lain SJ, Roberts CJ. Regional block versus general anaesthesia for caesarean section and neonatal outcomes: a population-based study. BMC. 2009;7(2):20. doi: 10.1186/1741-7015-7-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nkwabong E, Fomulu JN, Hamida A, Onana A, Tjek PT, Kouam L, et al. The Risk of adverse maternal and neonatal outcomes in cameroonian primiparous women aged more than 26 years. Clinics in Mother and Child Health. 2011;8(4):1–4. [Google Scholar]
- 47.Apgar V, Holiday DA, James LS, Weisbrot IM, Berrien C. Evaluation of the newborn infant: second report. JAMA. 1958;168(6):1985–88. doi: 10.1001/jama.1958.03000150027007. [DOI] [PubMed] [Google Scholar]
- 48.Allison S. Maternal and neonatal effects of caesarean section. BMJ. 2007;335(7628):1003–1004. doi: 10.1136/bmj.39372.587650.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zanardo V, Simbi AK, Franzoi M, Soldà G, Salvadori A, Trevisanuto D. Neonatal respiratory morbidity risk and mode of delivery at term: influence of timing of elective caesarean delivery. Acta Pædiatr. 2004;93(1):643–647. doi: 10.1111/j.1651-2227.2004.tb02990.x. [DOI] [PubMed] [Google Scholar]


