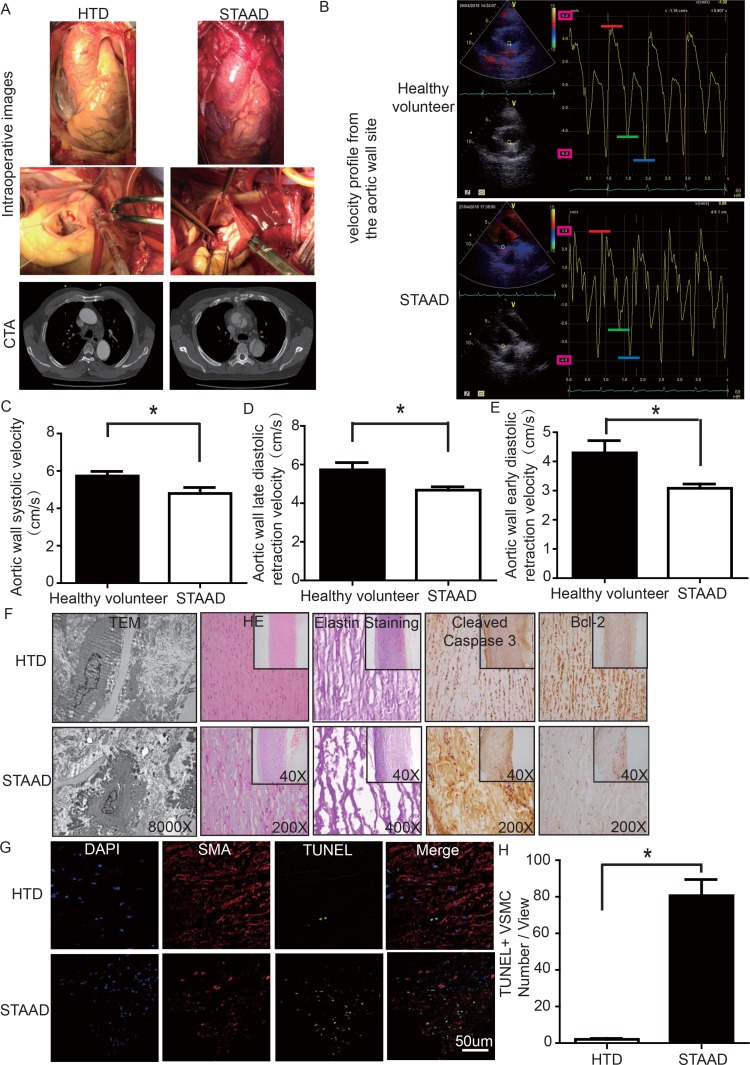
Figure 1.
(A) Intraoperative images and CTA results showing the enlarged ascending aorta and typical true and false cavities in STAAD. (B) Echocardiography showing the Vmax of healthy volunteers and patients with STAAD (including aortic wall systolic velocity (red line), late diastolic retraction velocity (blue line) and early diastolic retraction velocity (green line)). (C) The mean aortic wall systolic velocity of the ascending aorta was significantly lower in patients with STAAD than in healthy volunteers (n=5 in healthy volunteer group, n=5 in STAAD group, *p=0.0417). (D) The mean late-diastolic retraction velocity of the ascending aorta was significantly lower in patients with STAAD than in healthy volunteers (n=5 in Healthy volunteer group, n=5 in STAAD group, *p=0.0478). (E) The mean early-diastolic retraction velocity of the ascending aorta was significantly lower in patients with STAAD than in healthy volunteers (n=5 in healthy volunteer group, n=5 in STAAD group, *p=0.0407). (F) TEM showed partly fragmented and reduplicated elastic lamina and abnormal VSMCs, together with an electron-dense amorphous material peripheral cell membrane in the ascending aortic wall of patients with STAAD, H&E and elastin staining showed obvious ascending aorta tissue structure disorganization in patients with STAAD, and immuno-histochemistry showed that cleaved caspase-3 was present at high levels and bcl-2 was present at low levels in the ascending aortic wall of patients with STAAD relative to that of HTDs. (G, H) Confocal fluorescence microscopy showed that the numbers of double stained (TUNEL and α-SMA) cells was higher in the ascending aortic wall of patients with STAAD (n=19 in HTD group, n=23 in STAAD group, *p=0.0009).