Abstract
Background
Understanding that cancer is caused by both genetic and behavioral risk factors is an important component of genomic literacy. However, a considerable percentage of people in the U.S. do not endorse such multifactorial beliefs.
Methods
Using nationally representative cross-sectional data from the U.S. Health Information National Trends Survey (N=2,529), we examined how information seeking, information scanning, and key information processing characteristics were associated with endorsing a multifactorial model of cancer causation.
Results
Multifactorial beliefs about cancer were more common among respondents who engaged in cancer information scanning (p=.001), were motivated to process health information (p=.005), and who reported a family history of cancer (p=.0002). Respondents who reported having previous negative information seeking experiences had lower odds of endorsing multifactorial beliefs (p=.01). Multifactorial beliefs were not associated with cancer information seeking, trusting cancer information obtained from the Internet, trusting cancer information from a physician, self-efficacy for obtaining cancer information, numeracy, or being aware of direct-to-consumer genetic testing (ps>.05).
Conclusion
Gaining additional understanding of how people access, process, and use health information will be critical for the continued development and dissemination of effective health communication interventions and for the further translation of genomics research to public health and clinical practice.
Keywords: Multifactorial beliefs, genetics, information seeking, information scanning, causal beliefs, cancer
Introduction
Many common health conditions, including cancer, diabetes, heart disease, stroke, obesity, and hypertension are multifactorial in nature—that is, they are caused by a combination of genetic, behavioral, and environmental factors (Collins, Green, Guttmacher, & Guyer, 2003). Understanding the multifactorial nature of disease etiology is a critical component of genomic health literacy, which has been defined as “the capacity to obtain, process, understand, and use genomic information for health-related decision making” (Hurle et al., 2013). Yet, many laypeople do not endorse the multifactorial model of disease causation (Ashida et al., 2011; Claassen et al., 2011; O'Neill, McBride, Alford, & Kaphingst, 2010; Parrott, Silk, & Condit, 2003; Sanderson et al., 2013; Sanderson, Waller, Humphries, & Wardle, 2011; Wang, Miller, Egleston, Hay, & Weinberg, 2010; Wold, Byers, Crane, & Ahnen, 2005). Examination of population-level data indicates that 21–36% of people in the U.S. do not hold multifactorial causal beliefs for many common health conditions (Waters, Muff, & Hamilton, 2014). The absence of multifactorial beliefs is particularly notable for cancer, with 35.7% of the population failing to recognize the interplay between genes and behavior. There is also preliminary evidence that multifactorial beliefs may be less common among men, people with less formal education, non-Hispanic whites, residents of urban geographic areas, and people with limited numeracy (Waters et al., 2014).
Endorsing a multifactorial model of cancer causation is important not only because multifactorial beliefs are an accurate reflection of how the disease develops, but also because causal beliefs are associated with engagement in health behaviors (Leventhal, Brissette, & Leventhal, 2003). For example, individuals who endorse genetic causal beliefs may believe that a disease will develop regardless of their lifestyle behaviors, and consequently choose to take a medication instead of changing their behavior (Cameron, Marteau, Brown, Klein, & Sherman, 2012; Marteau & Weinman, 2006). In contrast, individuals who endorse behavioral causal beliefs may believe that their behavior can modify their risk of developing a health condition, and consequently, change their behavior (Nguyen, Oh, Moser, & Patrick, 2015). Simultaneously endorsing both genetic and behavioral causes of cancer (i.e., multifactorial cancer beliefs) is associated with higher engagement in cervical, breast, colorectal, and prostate cancer screening (Waters et al., 2014).
In sum, the available evidence indicates that there are substantial unmet information needs about the multifactorial nature of cancer causation. These unmet needs are associated with lower engagement in key cancer detection behaviors and may be related to socio-demographic characteristics that are associated with cancer disparities. Causal beliefs are generally formed based on specific information people obtain about a health condition (Leventhal et al., 2003). Therefore, improving understanding of the process by which people obtain cancer information, as well as the relationship between this process and endorsement of multifactorial beliefs, could inform the development and dissemination of health messages aimed at improving knowledge about the multifactorial nature of cancer causation. Such efforts would further the translation of genomics research into practice by helping the public understand ongoing developments in scientific knowledge about the complex interplay between genes and behavior and increase their adherence to cancer screening guidelines.
Obtaining Cancer Information
Information seeking and information scanning are two general strategies through which people can obtain information about cancer and other health conditions. Information seeking refers to actively and deliberately searching for and gathering information from the media, interpersonal conversation, the Internet, medical providers, or other information sources that are outside of the normal flow of conversation (Niederdeppe et al., 2007; Powe, 2015; Wong, 2012). This is different from information scanning, which refers to passively encountering information or being exposed to information unintentionally (Lee, Zhao, & Pena, 2016; Shim, Kelly, & Hornik, 2006).
Theories of health behavior (Conner & Norman, 1995), persuasion (Chaiken, Giner-Sorolla, & Chen, 1996; Petty & Cacioppo, 1996), and communication (Griffin, Dunwoody, & Neuwirth, 1999; McGuire, 1984; R. E. Smith & Swinyard, 1982) posit that information affects behavior by changing attitudes and beliefs. Although there is ample empirical evidence that information seeking and scanning are indeed important precursors of engagement in health behaviors, such as fruit and vegetable consumption (Beaudoin & Hong, 2011; Lewis et al., 2012; Ramirez et al., 2013) and colon and breast cancer screening behaviors (Shim et al., 2006; Shneyderman et al., 2015), much less research has examined the direct effect of cancer information seeking and scanning on health knowledge, attitudes, and beliefs. One study reported that higher engagement in information scanning (but not information seeking) was associated with stronger beliefs about the preventability of colon cancer and heart disease (Hovick & Bigsby, 2015). Another study reported that obtaining information about the human papilloma virus (HPV) was associated with more favorable beliefs about vaccinating a daughter against HPV (McRee, Reiter, & Brewer, 2012).
Data regarding the relationships among information seeking, scanning, and genetics-related knowledge, attitudes, and beliefs are particularly sparse. Information seeking was related to increased genetic knowledge among family members and patients with inherited bone marrow failure syndromes in one study (Hamilton et al., 2015), and increased awareness of direct-to-consumer (DTC) genetic testing in another (Agurs-Collins et al., 2015). Research about the association between information scanning and genetics-related knowledge is lacking, and similarly, no research has examined how information seeking or scanning may be related to the endorsement of multifactorial beliefs about cancer. This gap in the literature has implications for the development and dissemination of cancer education and communication efforts. For example, understanding the extent to which information seeking versus scanning contributes to the formation of multifactorial beliefs could help determine whether messages that require active engagement versus passive exposure, respectively, may be more effective.
Processing Cancer Information
The development of multifactorial beliefs may also be influenced by the way in which individuals process cancer information. Information processing is an important determinant of whether a given piece of information actually changes attitudes, beliefs, and behavior (Chaiken et al., 1996; Griffin et al., 1999; Petty & Cacioppo, 1996). Factors such as beliefs about the source of the information, perceived and actual ability to learn more about the issue, prior experience with the specific issue in question, and motivation to process information can all influence the extent to which a given piece of information changes knowledge, attitudes and beliefs.
Relatively few studies have examined these factors in the cancer domain, but there is some empirical support for many of these proposed relationships. For example, one study reported that having high levels of trust in health information from government agencies was associated with higher awareness of tobacco cessation telephone hotlines (Kaufman, Augustson, Davis, & Finney Rutten, 2010). Other research demonstrated that individuals with limited actual ability to understand and use numerical information (i.e., low numeracy) responded to colon cancer educational materials with less favorable attitudes towards colon cancer screening compared to individuals who had higher numeracy (S. G. Smith et al., 2014). Another study reported that daily smokers who were more confident in their ability to quit smoking (i.e., high self-efficacy) had more favorable attitudes towards quitting in response to an anti-smoking public service announcement than those who had lower self-efficacy (Falcone et al., 2013). In contrast, individuals who reported having negative experiences while seeking cancer information reported more pessimistic beliefs about cancer prevention than individuals who had more positive experiences (Arora et al., 2008). People who reported not wanting to know their risk of cancer (i.e., low motivation) also had more pessimistic beliefs about cancer prevention activities (Emanuel et al., 2015). Although some research demonstrated that prior experience with DTC genetic testing was associated with higher odds of endorsing multifactorial beliefs about cancer causation (Waters et al., 2014), very little is known about what other information processing factors are associated with the development of multifactorial beliefs. Understanding these relationships could further inform the development of future cancer communication efforts.
Objective and Hypotheses
This study explores the possible role of cancer information seeking, scanning, and processing in the development of multifactorial beliefs about cancer. It is guided by a conceptual framework that describes how information seeking, information scanning, information processing, and socio-demographic factors might contribute to the development of multifactorial causal beliefs about cancer and, consequently, influence engagement in healthy behaviors (Figure 1). Adapted from prior research (Waters et al., 2014), this framework draws upon theoretical and empirical work from psychology, communication, public health, and genomic medicine (Chaiken et al., 1996; Collins et al., 2003; Costanzo, Lutgendorf, & Roeder, 2011; Griffin et al., 1999; Hesse, Arora, & Khoury, 2012; Leventhal et al., 2003; Marteau & Weinman, 2006; McBride et al., 2008; Petty & Cacioppo, 1996; US Department of Health and Human Services, 2012). The following hypotheses were tested:
H1. Cancer information seeking and scanning will be associated with increased odds of endorsing multifactorial beliefs about cancer.
H2. The following information processing factors will be associated with increased odds of endorsing multifactorial beliefs: Higher trust in sources of cancer information, higher perceived ability to obtain cancer information (i.e., self-efficacy), higher actual ability to obtain cancer information (i.e., numeracy), higher motivation to process cancer information, and having prior experiences with genetics (i.e., aware of DTC genetic testing) and/or cancer (i.e., family history).
H3. Reporting more negative information seeking experiences will be associated with decreased odds of endorsing multifactorial beliefs.
Figure 1.
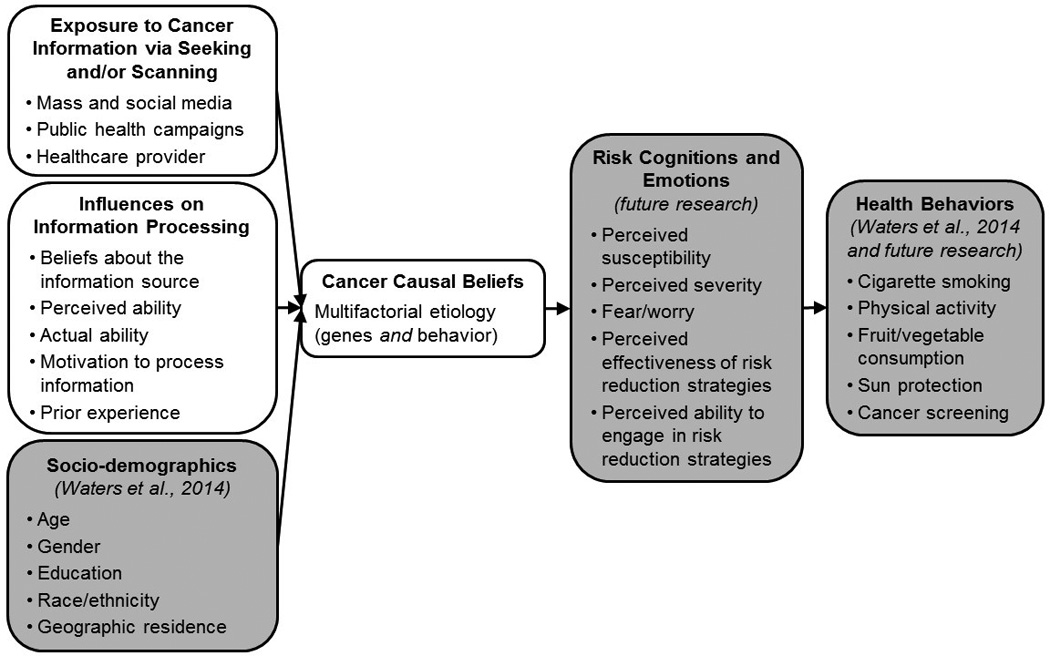
Conceptual framework describing the precursors and consequences of multifactorial beliefs about cancer causation, adapted from (Waters et al., 2014).
Methods
Data Source
Data were obtained from the Health Information National Trends Survey (HINTS 4, Cycle 2), which was administered through mailed self-report questionnaires from October 2012 through January 2013. HINTS is a population-based, nationally representative survey of the adult (ages 18 or older) civilian non-institutionalized population of the U.S. Detailed information about its methodology and response rate is available at hints.cancer.gov/docs/HINTS_4_Cycle2_Methods_Report.pdf.
Measures
Acquiring health information
Cancer information seeking was assessed with two items: “Have you ever looked for information about health or medical topics from any source?” and “Have you ever looked for information about cancer from any source?” [Yes; No]. Individuals who responded “No” to the health information seeking question were recoded as having not sought cancer information. Cancer information scanning was assessed indirectly with seven items that shared a question stem (Shim et al., 2006): “How much attention do you pay to information about cancer from each of the following sources: [In online newspapers; In print newspapers; In special health or medical magazines or newsletters; On the internet; On the radio; On local television news programs; On national or cable television news programs]?” The response options for each source ranged from [1] Not at all to [4] A lot. These seven items were averaged to create a scale in which higher scores were associated with more information scanning, α = 0.87.
Influences on information processing
Trust in the information source was assessed with two items: “In general, how much you would trust information about cancer from each of the following: [A doctor; Family or friends; Newspapers or magazines; Radio; Internet; Television; Government health agencies; Charitable organizations; Religious organizations and leaders]?” Response options ranged from [1] Not at all to [4] A lot. Because most people obtain their health information from the Internet (67.6%) or a healthcare provider (15.7%) (Volkman et al., 2014), we only examined trust in these two domains. Information seeking self-efficacy was assessed with the item: “Overall, how confident are you that you could get advice or information about cancer if you needed it?” Response options ranged from [1] not confident at all to [5] completely confident. Numeracy was assessed using the item, “As far as you know, who has a greater chance of getting cancer—a person with a 1 in 1,000 chance of getting cancer, or a person with a 1 in 100 chance?” Individuals who skipped the item were considered incorrect. Motivation to process cancer information was assessed with the item, “I’d rather not know my chance of getting cancer.” Response options ranged from [1] strongly agree to [4] strongly disagree.
Several items assessed prior experience
The family history of cancer item asked, “Have any of your family members ever had cancer? [Yes; No; Not sure].” Awareness of DTC genetic testing was assessed with the item, “Genetic tests that analyze your DNA, diet and lifestyle for potential health risks are currently being marketed by companies directly to consumers. Have you heard or read about these genetic tests? [Yes; No].” Negative cancer information seeking experience was assessed only for individuals who had ever sought cancer information. Four items shared the following question stem: “Based on the results of your most recent search for information about cancer, how much do you agree or disagree with each of the following statements: [It took a lot of effort to get the information you needed; You felt frustrated during your search for the information; You were concerned about the quality of the information; The information you found was hard to understand]?” Response options ranged from [1] strongly disagree to [4] strongly agree. These items were averaged to create a scale in which higher scores indicated more difficulty in obtaining and understanding cancer information, Cronbach’s α = 0.85 (Hesse, Arora, Burke Beckjord, & Finney Rutten, 2008).
Multifactorial beliefs
To examine the simultaneous endorsement of genetic and behavioral causal beliefs about cancer, we combined two causal beliefs items into a single dichotomous variable (Waters et al., 2014). The original items read, “How much do you think [health behaviors like diet, exercise, and smoking / genetics, that is characteristics passed from one generation to the next] determine whether or not a person will develop each of the following conditions: Diabetes; Obesity; Heart disease; High blood Pressure; Cancer?” The response options ranged from [1] Not at all to [4] A lot. Because this study focused specifically on cancer, only responses to the cancer items were examined. Respondents were defined as endorsing multifactorial beliefs about cancer if they responded “A lot” or “Somewhat” to both the genetic and behavior items. Respondents who provided any other combination of responses were coded as not endorsing multifactorial beliefs.
Covariates
Based on prior research examining predictors of multifactorial beliefs (Waters et al., 2014) and other research documenting differences in information seeking and/or scanning by socio-demographic characteristics (Finney Rutten et al., 2015; Kelly et al., 2010) and family history (Lee et al., 2016; Rutten, Squiers, & Hesse, 2006), several respondent characteristics were included as covariates. These included age, gender, education, race/ethnicity, and rural/urban geographic residence.
Analytic Strategy
In compliance with data analytic guidelines for HINTS (National Cancer Institute, 2013), data were analyzed using SAS 9.4 SURVEYFREQ and SURVEYLOGISTIC procedures using jackknife variance estimation. These procedures reduce the likelihood of a Type I error by accounting for the survey’s complex design and sampling scheme (Korn & Graubard, 1999). They also weight the data to yield estimates representative of the U.S. adult population.
There were 3,630 survey respondents, but our primary analytic sample is comprised of a subset of 2,529 individuals who provided complete data for all items of interest except those items assessing information seeking experiences. Information seeking experiences items were asked only of individuals who reported having ever purposefully sought cancer information. Because we were also interested in understanding the role of information scanning in the development of multifactorial beliefs, and information scanning can occur among people who do not seek information, we elected to examine information seeking experiences separately from the other information processing variables. Cancer survivors (n = 468) were also excluded due to the low number of respondents (which raised concerns about small cell sizes for some of the variables such as numeracy), as well as their unique information needs and experiences (Arora et al., 2008; Hesse et al., 2008). To permit accurate estimation of variance estimates for the subpopulation of respondents who provided complete data, the DOMAIN statement was used in conjunction with the SURVEY procedures (Korn & Graubard, 1999).
Respondents’ demographic characteristics, information seeking and scanning behavior, and information processing factors were examined using weighted descriptive statistics. Bivariate logistic regressions were used to examine the unadjusted associations between multifactorial beliefs (outcome) and information seeking, scanning, and processing (predictors). One multivariable logistic regression tested the combined influence of all information seeking, scanning, and processing variables (except negative information seeking experience) to determine which, if any, were most important for the endorsement of multifactorial cancer causal beliefs. A second multivariable logistic regression included negative information seeking experience as a predictor. Because negative information seeking experience was only relevant for information seekers, information seeking was not included in the second model. All multivariable analyses adjusted for age, gender, race, education, and geographic residence.
Results
Detailed information about respondents’ demographic and information seeking, scanning, and processing characteristics are described in Table 1. Weighted analyses indicated that the respondents were approximately equal in gender, primarily non-Hispanic white, primarily resided in an urban location, and were on average 43.5 years of age. A majority of respondents had at least some education beyond a high school diploma. The majority (65.6%) of the sample endorsed multifactorial beliefs about cancer causation. Information seeking and scanning behaviors were relatively limited; far less than half of respondents (37.3%) reported having ever sought cancer information, and the mean cancer information scanning rating was only slightly above “a little.” In general, trust in cancer information was moderate to high. Respondents reported “some” trust in cancer information obtained from the Internet and “a lot” of trust in cancer information from a doctor. Perceived (self-efficacy) and actual (numeracy) ability to obtain information were high. Motivation to process cancer information was moderate to high, with respondents “somewhat disagreeing” with not wanting to know their cancer risk. The sample also had relatively high prior experience with cancer, either through family history (66.5%) or awareness of DTC genetic testing (51.1%). Furthermore, respondents reported relatively low levels of negative information seeking experiences, generally “somewhat disagreeing” with statements about negative experiences.
Table 1.
Respondent characteristics (N = 2,529)
| Characteristic | n (unweighted) |
% (weighted) |
|---|---|---|
| Socio-demographics | ||
| Sex | ||
| Men | 995 | 50.7 |
| Women | 1534 | 49.3 |
| Education | ||
| Less than 12 years | 167 | 10.0 |
| 12 years or high school degree | 507 | 19.6 |
| Vo-Tech or some college | 757 | 38.4 |
| College graduate or more | 1098 | 32.0 |
| Race | ||
| Non-Hispanic white | 1575 | 68.0 |
| Non-white | 954 | 32.0 |
| Geographic location | ||
| Urban | 2170 | 84.8 |
| Rural | 359 | 15.2 |
| Age (Mean, SE) | 43.5 | 0.27 |
| Beliefs | ||
| Multifactorial beliefs | ||
| Yes | 1720 | 65.6 |
| No | 809 | 34.4 |
| Information Seeking and Processing | ||
| Seek Cancer Information | ||
| Yes | 1022 | 37.3 |
| No | 1507 | 62.7 |
| Actual Ability-Numeracy | ||
| Correct | 2254 | 91.3 |
| Not Correct | 275 | 8.7 |
| Prior Experience-Family History | ||
| Yes | 1726 | 66.5 |
| No | 803 | 33.5 |
| Prior Experience-Aware DTC Genetic Testing | ||
| Yes | 1300 | 51.1 |
| No | 1229 | 48.9 |
| Scan Cancer Information (Mean, SE) | 2.2 | 0.03 |
| Trust-Internet (Mean, SE) | 2.9 | 0.03 |
| Trust-Doctor (Mean, SE) | 3.7 | 0.02 |
| Perceived Ability-Self-Efficacy (Mean, SE) | 3.8 | 0.04 |
| Motivation to Process Information (Mean, SE) | 2.8 | 0.03 |
| Prior Experience-Negative Information Seeking (Mean, SE) |
2.2 | 0.04 |
Note. DTC = Direct-to-Consumer. Negative Information Seeking Experiences n = 986. All continuous variables except age have four response options.
Bivariate examination of the relationship between demographic variables and information seeking indicated that women engaged in more information seeking and scanning than men, but lower information seeking was associated with having less than a college degree and being a member of a racial or ethnic minority group (Table 2). In contrast, information scanning was associated race/ethnicity but not educational attainment.
Table 2.
Bivariate relationships between sociodemographic characteristics and information seeking and scanning
| Information seeking (N = 2,529) |
Information scanning (N = 2,529) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Predictor | OR | 95% CI | p | b | 95% CI | p | ||||
| Age | 1.0 | 1.0 | - | 1.0 | .12 | 0.0 | 0.0 | - | 0.0 | .80 |
| Female | 1.8 | 1.4 | - | 2.2 | .0001 | 0.2 | 0.1 | - | 0.2 | .0005 |
| Education | ||||||||||
| Less than 12 years | 0.2 | 0.1 | - | 0.4 | .0001 | 0.1 | −0.1 | - | 0.3 | .34 |
| 12 years or high school degree | 0.4 | 0.3 | - | 0.6 | .18 | −0.1 | −0.2 | - | 0.1 | .30 |
| Vo-Tech or some college | 0.6 | 0.5 | - | 0.8 | .01 | 0.0 | −0.1 | - | 0.1 | .91 |
| College graduate or more | Ref | Ref | ||||||||
| Non-White Race | 0.7 | 0.5 | - | 1.0 | .03 | 0.3 | 0.2 | - | 0.4 | .0001 |
| Rural Geographic Residence | 1.1 | 0.8 | - | 1.6 | .58 | −0.1 | −0.2 | - | 0.0 | .08 |
As shown in Table 3, bivariate analyses indicated that multifactorial beliefs were statistically significantly more common among people who had higher information scanning behaviors, higher motivation to process cancer information, and who had a family history of cancer (ps < .05). In contrast, multifactorial beliefs were significantly less common among people who had more negative information seeking experiences (p < .05). Endorsing multifactorial beliefs was not related to cancer information seeking, trust in cancer information obtained from the Internet, trust in cancer information obtained from a doctor, self-efficacy for obtaining cancer information, numeracy, or having prior awareness of DTC genetic testing services (ps < .05).
Table 3.
Predictors of endorsing multifactorial beliefs about cancer
| Bivariate analysis (N = 2,529) |
Multivariable analysis-A (N = 2,529) |
Multivariable analysis-B (N = 986) |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Predictor | OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | ||||||
| Information Seeking and Scanning | |||||||||||||||
| Seek Cancer Information | 1.1 | 0.8 | - | 1.5 | 0.52 | 0.8 | 0.6 | - | 1.2 | 0.28 | - | - | - | - | |
| Scan Cancer Information | 1.4 | 1.1 | - | 1.7 | 0.004 | 1.4 | 1.1 | - | 1.7 | 0.001 | 1.3 | 0.9 | - | 1.8 | 0.23 |
| Information Processing | |||||||||||||||
| Trust-Internet | 1.3 | 1.0 | - | 1.6 | 0.08 | 1.2 | 0.9 | - | 1.6 | 0.25 | 1.2 | 0.8 | - | 1.9 | 0.29 |
| Trust-Doctor | 1.1 | 0.9 | - | 1.4 | 0.30 | 1.0 | 0.8 | - | 1.2 | 0.73 | 0.9 | 0.6 | - | 1.4 | 0.68 |
| Perceived Ability-Self-Efficacy | 1.1 | 0.9 | - | 1.2 | 0.39 | 1.0 | 0.9 | - | 1.2 | 0.98 | 0.9 | 0.7 | - | 1.2 | 0.51 |
| Actual Ability-Numeracy | 1.2 | 0.8 | - | 1.7 | 0.32 | 1.2 | 0.8 | - | 1.8 | 0.32 | 1.6 | 0.7 | - | 3.6 | 0.29 |
| Motivation to Process Information | 1.2 | 1.1 | - | 1.4 | 0.01 | 1.3 | 1.1 | - | 1.5 | 0.005 | 1.3 | 1.1 | - | 1.6 | 0.01 |
| Prior Experience-Family History | 1.8 | 1.4 | - | 2.5 | <0.001 | 1.9 | 1.4 | - | 2.7 | 0.001 | 2.0 | 1.1 | - | 3.6 | 0.03 |
| Prior Experience-Aware DTC Genetic Testing |
1.2 | 0.8 | - | 1.6 | 0.40 | 1.2 | 0.8 | - | 1.6 | 0.36 | 1.0 | 0.6 | - | 1.7 | 0.92 |
| Prior Experience-Negative Information Seeking |
0.7 | 0.5 | - | 1.0 | 0.03 | - | - | - | - | 0.7 | 0.5 | - | 0.9 | 0.01 | |
| Socio-Demographic Covariates | |||||||||||||||
| Age | 1.0 | 1.0 | - | 1.0 | .13 | 1.01 | 1.00 | - | 1.02 | .02 | 1.0 | 1.0 | - | 1.0 | .13 |
| Female | 1.3 | 0.9 | - | 1.8 | .10 | 1.2 | 0.9 | - | 1.7 | .23 | 1.4 | 0.8 | - | 2.3 | .27 |
| Education | |||||||||||||||
| Less than 12 years | 0.6 | 0.4 | - | 1.3 | .61 | 0.7 | .04 | - | 1.3 | .44 | 0.5 | 0.1 | - | 1.9 | .50 |
| 12 years or high school degree | 0.8 | 0.5 | - | 1.3 | .55 | 0.8 | 0.5 | - | 1.3 | .79 | 0.5 | 0.3 | - | 1.1 | .44 |
| Vo-Tech or some college | 0.9 | 0.6 | - | 1.2 | .92 | 0.8 | 0.6 | - | 1.2 | 1.0 | 0.8 | 0.5 | - | 1.3 | .58 |
| College graduate or more | ref | ref | ref | ||||||||||||
| Non-White Race | 1.1 | 0.8 | - | 1.5 | .47 | 1.2 | 0.9 | - | 1.8 | .20 | 1.5 | 0.9 | - | 2.7 | .14 |
| Rural Geographic Residence | 1.5 | 0.9 | - | 2.3 | .11 | 1.6 | 1.0 | - | 2.8 | .06 | 1.4 | 0.7 | - | 2.9 | .37 |
Note. Multivariable models controlled for age, sex, education, race, and geographic residence. Prior experience-negative information seeking was asked only of individuals who reported ever seeking cancer information. Thus, it could not be included in analyses examining the relationship between cancer information seeking and multifactorial beliefs (i.e., Multivariable analysis-A). Similarly, the relationship between prior negative information seeking experiences and multifactorial beliefs could not be examined with cancer information seeking in the model (i.e., Multivariable analysis-B).
The adjusted multivariable models showed nearly identical results. In both models, higher motivation to process cancer information and having a family history of cancer were associated with higher endorsement of multifactorial beliefs (Table 3). The examination of information seeking, scanning, and negative experiences was more complex due to the skip patterns embedded within the survey. Model A examined cancer information seeking and scanning but not negative information seeking experiences, because the information seeking experiences scale was not administered to people who reported not seeking health information. In Model A, cancer information scanning was associated with endorsing multifactorial beliefs, but cancer information seeking was not (Table 3, Multivariable analysis-A).
Model B examined the role of negative information seeking experiences and information scanning, but only among people who reported seeking information in the previous year. Again, this was because the information seeking experiences scale was administered only to information seekers. In Model B, cancer information scanning was no longer statistically significant. However, as in the bivariate analysis, having prior negative information seeking experiences was associated with less endorsement of multifactorial beliefs (Table 3, Multivariable analysis-B).
Discussion
Multifactorial beliefs are a key component of genomic literacy and have cross-sectional associations with higher engagement in cancer screening behaviors (Waters et al., 2014). However, a sizeable proportion of the U.S. population does not endorse a multifactorial model of cancer causation. In addition to its potential implications for cancer screening behaviors, lack of concordance between lay and expert conceptualizations of risk, as indicated by not endorsing multifactorial beliefs, may promote mistrust of health communicators and skepticism of scientific findings (Gurmankin Levy, Weinstein, Kidney, Scheld, & Guarnaccia, 2008). This, in turn, could further complicate the translation of basic genomics research to clinical and public health practice.
This study sought to improve understanding of what information seeking, scanning, and processing factors may contribute to the development of multifactorial beliefs, with the goal of informing the development and dissemination of health communication interventions and furthering the translation of genomics research into clinical and public health practice. We found that happenstance encounters with cancer information (i.e., information scanning) may have a more important relationship with multifactorial beliefs than purposive cancer information seeking. This is consistent with research examining the combined association between information seeking and scanning with health beliefs (Hovick & Bigsby, 2015). To speculate, it could be that people who are searching for specific information, as is the case with purposive information seeking, are less open to other types of information that either do not seem directly relevant to their goals or that conflict with their pre-existing beliefs (Petty & Cacioppo, 1996). This relative lack of openness may result in the information seeker who is searching for specific types of cancer information (e.g., treatment) to either not read or not encode seemingly extraneous information about the multifactorial nature of cancer into their causal models. This question should be examined using experimental and prospective research designs to confirm the directionality and causal relationships among variables.
We also found support for some—but not all—of the examined information processing variables. Although theories of health communication and persuasion posit that information processing factors such as trust in the message source and individual ability are critical for shaping attitudes and beliefs (Chaiken et al., 1996; Griffin et al., 1999; Petty & Cacioppo, 1996), our findings suggest that other factors may have greater importance in this health context. We observed that multifactorial beliefs were more common among people with higher motivation to process information, who reported having a family history of cancer, and who had more positive prior information seeking experiences. These findings are consistent with other research (Arora et al., 2008; Emanuel et al., 2015), and suggest areas for future theoretical and empirical work. For instance, there is a need to better understand motivation to process health-related information, including identifying specific situations or strategies that can effectively enhance people’s motivation and/or increase their receptivity to communication regarding genetic and behavioral contributors to cancer. Clarifying the role of motivation in health information seeking and scanning may therefore facilitate the development of future genomics-related health communication efforts.
The absence of a relationship between multifactorial beliefs and numeracy was unexpected, because numeracy has been shown to be an important predictor of understanding health information generally (Nelson, Reyna, Fagerlin, Lipkus, & Peters, 2008) and genetic information in particular (Ostergren et al., 2015). It is possible that our results are due to a restricted range in numeracy; less than 10% qualified as having low numeracy in our analytic sample. This restricted range was likely the result of a single-item measure, which was implemented due to space constraints in the survey. Unfortunately, there was no health literacy item in the survey. Future research should examine the interrelationships among health literacy, numeracy, and multifactorial beliefs using validated measures.
A critical unanswered question regarding the formation of multifactorial beliefs about cancer relates to the temporal and causal relationships among information seeking, scanning, and processing. When comparing the two multivariable analysis models, it is notable that adding negative information seeking experiences to the model reduced the significance of information scanning to non-significance. Yet, the study data limit our ability to infer that negative information seeking experiences is a mediator of the relationship between cancer information scanning and multifactorial beliefs. First, because mediation is a causal process and our data were cross-sectional, it is not appropriate to test mediational hypotheses in this situation. Second, the model that includes negative information seeking experiences is comprised solely of information seekers, whereas the other model includes both seekers and non-seekers. Future research should attempt to unpack these relationships using an experimental design to manipulate the quality of an information seeking experience. This could be done by comparing information scanning levels after participants read health information written at a purposefully higher versus lower reading level, or by placing relevant information in the middle versus at the beginning of paragraphs.
Strengths, Limitations, and Additional Future Directions
A notable strength of this study is the use of a large, population-based survey to examine novel associations between information seeking, scanning, and processing and the presence of multifactorial beliefs about the etiology of cancer. Evidence consistent with some aspects of the conceptual framework and study hypotheses was obtained. Despite the cross-sectional nature of our data, these findings generate several hypotheses that can be examined in future studies. For example, a prospective study that experimentally varies the complexity of information (therefore producing more negative information seeking experiences) could yield important insights into the conditions under which people do and do not learn about the multifactorial basis of cancer. This type of study could help confirm the role of the information environment in shaping the development of multifactorial beliefs and the subsequent adoption of health-promoting behaviors. Prospective work should also confirm the directionality of the link between multifactorial beliefs and engagement in health behaviors.
As is true of HINTS and many other large, population-based surveys, single-item, self-reported measures were used to assess the study variables. As a result, there are limitations in the scope and depth of data available for examining these research questions. For example, items did not assess the frequency of cancer information seeking behaviors. Thus, while we did not observe a significant association between ever seeking information about cancer and multifactorial beliefs, it remains possible that these beliefs are more common among those who more frequently seek out cancer information. Furthermore, the measure of multifactorial beliefs was limited in scope, assessing only a dichotomous endorsement of the shared role of genetics and behavior in cancer causation. There is a need for measures of multifactorial beliefs that are more statistically powerful (e.g., scale measures, or single-item measures that assess this construct as a continuous variable) and comprehensive (e.g., incorporate a broader range of risk factors such as environmental exposures).
The constantly-evolving information environment also presents challenges to the assessment of information scanning behaviors. For instance, HINTS assessed information scanning from sources including “online newspapers” and “the Internet”; yet, the extent to which respondents conceptualize these as distinct sources of information is unclear. Respondents’ experiences with additional online sources that have gained increasing traction in recent years, including social media websites like Facebook, Twitter, and Instagram, as well as blogs of celebrities or laypeople, were not specifically evaluated. However, these information sources may have unique, strong, and lasting effects on the public’s understanding of health and disease (Dunn, Leask, Zhou, Mandl, & Coiera, 2015; Neubaum & Kramer, 2015).
Finally, it is unknown whether the observed relationships will hold true for non-cancer-related health conditions. Multifactorial beliefs for health conditions including heart disease, hypertension, diabetes, and obesity are fairly common (Waters et al., 2014). Future investigations should examine how exposure to health messages may influence people’s understanding of these and other important health conditions.
Conclusion
There is an abundance of cancer-related information available for public consumption, including messages that reflect growing scientific understanding about the role of genes and heredity in relation to traditional behavioral risk factors such as tobacco use, diet, and exercise. Making sense of this complex interplay of risk factors is challenging, and a key aspect of genomic literacy—understanding that cancer is caused by both genetic and behavioral factors—is limited. People who experience difficulties understanding and obtaining health information are particularly vulnerable to misunderstanding this concept, which may prompt them to reject messaging related to multifactorial beliefs. Improving the public’s awareness of the multifactorial nature of cancer causation is important, particularly because these beliefs are associated with the adoption of protective health behaviors. Gaining additional understanding of how people access, process, and use genetic and behavioral risk information will be critical for the continued development and dissemination of effective health communication interventions and for the further translation of genomics research to public health and clinical practice.
Acknowledgments
Funding: This work was supported by MRSG-11-214-01-CPPB (Erika A. Waters) and NCI 2 P30 CA08748-48 (Jada G. Hamilton). The funding agreement ensured the authors' independence in designing the study, interpreting the data, writing, and publishing the report. There are no real or potential conflicts of interest with the funding organization.
Footnotes
Compliance with Ethical Standards
Human and Animal Rights: This article does not contain any studies with human participants or animals performed by any of the authors.
Conflict of Interest: The authors declare that they have no conflicts of interest.
References
- Agurs-Collins T, Ferrer R, Ottenbacher A, Waters EA, O’Connell ME, Hamilton JG. Public Awareness of Direct-to-Consumer Genetic Tests: Findings from the 2013 U.S. Health Information National Trends Survey. Journal of Cancer Education. 2015;30(4):799–807. doi: 10.1007/s13187-014-0784-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arora NK, Hesse BW, Rimer BK, Viswanath K, Clayman ML, Croyle RT. Frustrated and confused: the American public rates its cancer-related information-seeking experiences. Journal of General Internal Medicine. 2008;23(3):223–228. doi: 10.1007/s11606-007-0406-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashida S, Goodman M, Pandya C, Koehly LM, Lachance C, Stafford J, Kaphingst KA. Age differences in genetic knowledge, health literacy and causal beliefs for health conditions. Public Health Genomics. 2011;14(4–5):307–316. doi: 10.1159/000316234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beaudoin CE, Hong T. Health information seeking, diet and physical activity: an empirical assessment by medium and critical demographics. International Journal of Medical Informatics. 2011;80(8):586–595. doi: 10.1016/j.ijmedinf.2011.04.003. [DOI] [PubMed] [Google Scholar]
- Cameron LD, Marteau TM, Brown PM, Klein WM, Sherman KA. Communication strategies for enhancing understanding of the behavioral implications of genetic and biomarker tests for disease risk: The role of coherence. Journal of Behavioral Medicine. 2012;35(3):286–298. doi: 10.1007/s10865-011-9361-5. [DOI] [PubMed] [Google Scholar]
- Chaiken S, Giner-Sorolla R, Chen S. Beyond accuracy: Defense and impression motives in heuristic and systematic information processing. In: Gollwitzer PM, Bargh JA, editors. The Psychology of Action: Linking Cognition and Motivation to Behavior. New York, NY: Guilford Press; 1996. pp. 553–578. [Google Scholar]
- Claassen L, Henneman L, Nijpels G, Dekker J, Marteau T, Timmermans D. Causal beliefs and perceptions of risk for diabetes and cardiovascular disease, The Netherlands, 2007. Preventing Chronic Disease. 2011;8(6):A130. [PMC free article] [PubMed] [Google Scholar]
- Collins FS, Green ED, Guttmacher AE, Guyer MS. A vision for the future of genomics research. Nature. 2003;422(6934):835–847. doi: 10.1038/nature01626. [DOI] [PubMed] [Google Scholar]
- Conner M, Norman P, editors. Predicting Health Behaviour. Buckingham/Philadelphia: Open University Press; 1995. [Google Scholar]
- Costanzo ES, Lutgendorf SK, Roeder SL. Common-sense beliefs about cancer and health practices among women completing treatment for breast cancer. Psycho-Oncology. 2011;20(1):53–61. doi: 10.1002/pon.1707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn AG, Leask J, Zhou X, Mandl KD, Coiera E. Associations Between Exposure to and Expression of Negative Opinions About Human Papillomavirus Vaccines on Social Media: An Observational Study. Journal of Medical Internet Research. 2015;17(6):e144. doi: 10.2196/jmir.4343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emanuel AS, Kiviniemi MT, Howell JL, Hay JL, Waters EA, Orom H, Shepperd JA. Avoiding cancer risk information. Social Science and Medicine. 2015;147:113–120. doi: 10.1016/j.socscimed.2015.10.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falcone M, Lerman C, Cappella JN, Sanborn P, Jepson C, Strasser AA. No untoward effects of smoking cues in anti-smoking public service announcements. Drug and Alcohol Dependence. 2013;133(1):279–282. doi: 10.1016/j.drugalcdep.2013.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finney Rutten LJ, Agunwamba AA, Wilson P, Chawla N, Vieux S, Blanch-Hartigan D, Hesse BW. Cancer-Related Information Seeking Among Cancer Survivors: Trends Over a Decade (2003–2013) Journal of Cancer Education. 2015 doi: 10.1007/s13187-015-0802-7. [DOI] [PubMed] [Google Scholar]
- Griffin RJ, Dunwoody S, Neuwirth K. Proposed model of the relationship of risk information seeking and processing to the development of preventive behaviors. Environmental Research. 1999;80(2 Pt 2):S230–S245. doi: 10.1006/enrs.1998.3940. [DOI] [PubMed] [Google Scholar]
- Gurmankin Levy A, Weinstein N, Kidney E, Scheld S, Guarnaccia P. Lay and expert interpretations of cancer cluster evidence. Risk Analysis. 2008;28(6):1531–1538. doi: 10.1111/j.1539-6924.2008.01110.x. [DOI] [PubMed] [Google Scholar]
- Hamilton JG, Hutson SP, Frohnmayer AE, Han PK, Peters JA, Carr AG, Alter BP. Genetic Information-Seeking Behaviors and Knowledge among Family Members and Patients with Inherited Bone Marrow Failure Syndromes. J Genet Couns. 2015;24(5):760–770. doi: 10.1007/s10897-014-9807-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hesse BW, Arora NK, Burke Beckjord E, Finney Rutten LJ. Information support for cancer survivors. Cancer. 2008;112(Suppl 11):2529–2540. doi: 10.1002/cncr.23445. [DOI] [PubMed] [Google Scholar]
- Hesse BW, Arora NK, Khoury MJ. Implications of Internet availability of genomic information for public health practice. Public Health Genomics. 2012;15(3–4):201–208. doi: 10.1159/000335892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hovick SR, Bigsby E. Heart Disease and Colon Cancer Prevention Beliefs and Their Association With Information Seeking and Scanning. J Health Commun. 2015:1–9. doi: 10.1080/10810730.2015.1049307. [DOI] [PubMed] [Google Scholar]
- Hurle B, Citrin T, Jenkins JF, Kaphingst KA, Lamb N, Roseman JE, Bonham VL. What does it mean to be genomically literate?: National Human Genome Research Institute Meeting Report. Genetics in Medicine. 2013;15(8):658–663. doi: 10.1038/gim.2013.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman A, Augustson E, Davis K, Finney Rutten LJ. Awareness and use of tobacco quitlines: evidence from the Health Information National Trends Survey. J Health Commun. 2010;15(Suppl 3):264–278. doi: 10.1080/10810730.2010.526172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly B, Hornik R, Romantan A, Schwartz JS, Armstrong K, DeMichele A, Wong N. Cancer information scanning and seeking in the general population. J Health Commun. 2010;15(7):734–753. doi: 10.1080/10810730.2010.514029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korn EL, Graubard BI. Analysis of health surveys. New York, NY: John Wiley & Sons; 1999. pp. 22–28.pp. 64–28. [Google Scholar]
- Lee CJ, Zhao X, Pena YLM. Theorizing the Pathways From Seeking and Scanning to Mammography Screening. Health Commun. 2016;31(1):117–128. doi: 10.1080/10410236.2014.942769. [DOI] [PubMed] [Google Scholar]
- Leventhal H, Brissette I, Leventhal EA. The common-sense model of self-regulation of health and illness. In: Cameron LD, Leventhal H, editors. The self-regulation of health and illness behaviour. New York, NY: Routledge; 2003. pp. 42–65. [Google Scholar]
- Lewis N, Martinez LS, Freres DR, Schwartz JS, Armstrong K, Gray SW, Hornik RC. Seeking cancer-related information from media and family/friends increases fruit and vegetable consumption among cancer patients. Health Commun. 2012;27(4):380–388. doi: 10.1080/10410236.2011.586990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marteau TM, Weinman J. Self-regulation and the behavioural response to DNA risk information: A theoretical analysis and framework for future research. Social Science and Medicine. 2006;62:1360–1368. doi: 10.1016/j.socscimed.2005.08.005. [DOI] [PubMed] [Google Scholar]
- McBride CM, Hensley-Alford S, Reid RJ, Larson EB, Baxevanis AD, Brody LC. Putting science over supposition in the arena of personalized genomics. Nature Genetics. 2008;40(8):939–942. doi: 10.1038/ng0808-939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuire WJ. Public communication as a strategy for inducing health-promoting behavior change. Preventive Medicine. 1984;13(3):299–313. doi: 10.1016/0091-7435(84)90086-0. [DOI] [PubMed] [Google Scholar]
- McRee AL, Reiter PL, Brewer NT. Parents' Internet use for information about HPV vaccine. Vaccine. 2012;30(25):3757–3762. doi: 10.1016/j.vaccine.2011.11.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Cancer Institute. Health Information National Trends Survey 4 (HINTS 4) Cycle 2 Analytic Recommendations. [Retrieved September 27, 2013];2013 [Google Scholar]
- Nelson W, Reyna VF, Fagerlin A, Lipkus I, Peters E. Clinical implications of numeracy: Theory and practice. Annals of Behavioral Medicine. 2008;35:261–274. doi: 10.1007/s12160-008-9037-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neubaum G, Kramer NC. Let's Blog About Health! Exploring the Persuasiveness of a Personal HIV Blog Compared to an Institutional HIV Website. Health Commun. 2015;30(9):872–883. doi: 10.1080/10410236.2013.856742. [DOI] [PubMed] [Google Scholar]
- Nguyen AB, Oh A, Moser RP, Patrick H. Perceptions of the roles of behaviour and genetics in disease risk: are they associated with behaviour change attempts. Psychology & Health. 2015;30(3):336–353. doi: 10.1080/08870446.2014.972958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niederdeppe J, Hornik RC, Kelly BJ, Frosch DL, Romantan A, Stevens RS, Schwartz JS. Examining the dimensions of cancer-related information seeking and scanning behavior. Health Commun. 2007;22(2):153–167. doi: 10.1080/10410230701454189. [DOI] [PubMed] [Google Scholar]
- O'Neill SC, McBride CM, Alford SH, Kaphingst KA. Preferences for genetic and behavioral health information: The impact of risk factors and disease attributions. Annals of Behavioral Medicine. 2010;40(2):127–137. doi: 10.1007/s12160-010-9197-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ostergren JE, Gornick MC, Carere DA, Kalia SS, Uhlmann WR, Ruffin MT, Group PGS. How Well Do Customers of Direct-to-Consumer Personal Genomic Testing Services Comprehend Genetic Test Results? Findings from the Impact of Personal Genomics Study. Public Health Genomics. 2015;18(4):216–224. doi: 10.1159/000431250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parrott RL, Silk KJ, Condit C. Diversity in lay perceptions of the sources of human traits: genes, environments, and personal behaviors. Social Science and Medicine. 2003;56(5):1099–1109. doi: 10.1016/s0277-9536(02)00106-5. [DOI] [PubMed] [Google Scholar]
- Petty RE, Cacioppo JT. The elaboration likelihood model of persuasion. In: Berkowitz L, editor. Advances in Experimental Social Psychology. Vol. 19. New York, NY: Academic Press; 1996. pp. 123–205. [Google Scholar]
- Powe BD. Health Information Seeking Among Rural African Americans, Caucasians, and Hispanics: It Is Built, Did They Come? Nursing Clinics of North America. 2015;50(3):531–543. doi: 10.1016/j.cnur.2015.05.007. [DOI] [PubMed] [Google Scholar]
- Ramirez AS, Freres D, Martinez LS, Lewis N, Bourgoin A, Kelly BJ, Hornik RC. Information seeking from media and family/friends increases the likelihood of engaging in healthy lifestyle behaviors. J Health Commun. 2013;18(5):527–542. doi: 10.1080/10810730.2012.743632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutten LJ, Squiers L, Hesse B. Cancer-related information seeking: hints from the 2003 Health Information National Trends Survey (HINTS) J Health Commun. 2006;11(Suppl 1):147–156. doi: 10.1080/10810730600637574. [DOI] [PubMed] [Google Scholar]
- Sanderson SC, Diefenbach MA, Streicher SA, Jabs EW, Smirnoff M, Horowitz CR, Richardson LD. Genetic and lifestyle causal beliefs about obesity and associated diseases among ethnically diverse patients: a structured interview study. Public Health Genomics. 2013;16(3):83–93. doi: 10.1159/000343793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanderson SC, Waller J, Humphries SE, Wardle J. Public awareness of genetic influence on chronic disease risk: are genetic and lifestyle causal beliefs compatible? Public Health Genomics. 2011;14(4–5):290–297. doi: 10.1159/000294280. [DOI] [PubMed] [Google Scholar]
- Shim M, Kelly B, Hornik R. Cancer information scanning and seeking behavior is associated with knowledge, lifestyle choices, and screening. J Health Commun. 2006;11(Suppl 1):157–172. doi: 10.1080/10810730600637475. [DOI] [PubMed] [Google Scholar]
- Shneyderman Y, Rutten LJ, Arheart KL, Byrne MM, Kornfeld J, Schwartz SJ. Health Information Seeking and Cancer Screening Adherence Rates. Journal of Cancer Education. 2015 doi: 10.1007/s13187-015-0791-6. [DOI] [PubMed] [Google Scholar]
- Smith RE, Swinyard WR. Information Response Models: An Integrated Approach. Journal of Marketing. 1982;46(1):81–93. [Google Scholar]
- Smith SG, Kobayashi LC, Wolf MS, Raine R, Wardle J, von Wagner C. The associations between objective numeracy and colorectal cancer screening knowledge, attitudes and defensive processing in a deprived community sample. Journal of Health Psychology. 2014 doi: 10.1177/1359105314560919. [DOI] [PubMed] [Google Scholar]
- US Department of Health and Human Services. Healthy People 2020. [Retrieved Feb 27, 2012];2012 from http://www.healthypeople.gov/2020/default.aspx.
- Volkman JE, Luger TM, Harvey KL, Hogan TP, Shimada SL, Amante D, Houston TK. The National Cancer Institute's Health Information National Trends Survey [HINTS]: a national cross-sectional analysis of talking to your doctor and other healthcare providers for health information. BMC Family Practice. 2014;15:111. doi: 10.1186/1471-2296-15-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C, Miller SM, Egleston BL, Hay JL, Weinberg DS. Beliefs about the causes of breast and colorectal cancer among women in the general population. Cancer Causes and Control. 2010;21(1):99–107. doi: 10.1007/s10552-009-9439-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waters EA, Muff J, Hamilton JG. Multifactorial beliefs about the role of genetics and behavior in common health conditions: prevalence and associations with participant characteristics and engagement in health behaviors. Genetics in Medicine. 2014;16(12):913–921. doi: 10.1038/gim.2014.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wold KS, Byers T, Crane LA, Ahnen D. What do cancer survivors believe causes cancer? (United States) Cancer Causes and Control. 2005;16(2):115–123. doi: 10.1007/s10552-004-2414-0. [DOI] [PubMed] [Google Scholar]
- Wong NC. Interaction of Comparative Cancer Risk and Cancer Efficacy Perceptions on Cancer-Related Information Seeking and Scanning Behaviors. Commun Res Rep. 2012;29(3):193–203. doi: 10.1080/08824096.2012.684808. [DOI] [PMC free article] [PubMed] [Google Scholar]


