Abstract
Background
Domestic violence is a global health problem as well as a violation against human rights. The aim of this study was to explore prevalence and incidence of domestic violence during pregnancy and 1 to 1.5 years postpartum as well as to explore the history of violence among new mothers in the southwestern region of Sweden. In addition, the aim was to explore the association between domestic violence postpartum and possible risk factors.
Methods
This is a longitudinal cohort-study including pregnant women ≥ 18 years of age. Total 1939 pregnant women were recruited to the study and requested to answer three questionnaires (QI-III) during pregnancy and postpartum. Statistical analysis were descriptive statistics, logistic regression and multiple regression with Odds ratios (OR) and 95 % confidence intervals (95 % CI).
Results
The response rate for those who received the Q-III (n = 755) at a Child Welfare Center was almost 97 % (n = 731). When all three questionnaires were answered the prevalence of domestic violence during pregnancy irrespective of type or severity was reported by 2.5 % (n = 40/1573). At 1 to 1.5 years postpartum the prevalence of domestic violence had increased to 3.3 % (n = 23/697). The incidence was 14 per 1000 women during pregnancy and 17.2 per 1000 women postpartum. The strongest risk factor for domestic violence reported at1-1.5 years postpartum was a history of violence whereby all of the women (n = 23) who had revealed their exposure to domestic violence postpartum also reported a history of violence (p < 0.001). Being single/living apart gave a 12.9 times higher risk for domestic violence postpartum (AOR 12.9; 95 % CI: 4.5–37.1). Having several symptoms of depression and a low score on the SOC-scale gave a 3.5 and 3.0 times higher risk respectively (AOR 3.5; 95 % CI: 1.2–10.4) and (AOR 3.0; 95 % CI 1.1–8.3).
Conclusion
Domestic violence increases as the pregnancy develops and postpartum. A history of violence and being single/living apart may be strong indicators for domestic violence during pregnancy as well as postpartum. Also, having symptoms of depression are associated with domestic violence both during pregnancy and postpartum. Collaboration between health care providers at Antenatal and Welfare centres is essential.
Keywords: Domestic violence, Longitudinally, Pregnancy, Postpartum, Prevalence, Incidence, Risk factors
Background
Domestic violence (DV) is a complex global public health problem as well as a violation against human rights [1]. The definition of DV, as used in this study, is in agreement with the WHO’s definition [2] where it is defined as physical, sexual or psychological, or emotional violence, or threats of physical or sexual violence that are inflicted on a pregnant woman by a family member, i.e. an intimate male partner, marital/cohabiting partner, parents, siblings, or a person very well known to the family, or a significant other, (i.e. former partner) when such violence often takes place in the home. Intimate partner violence (IPV) is included in the definition of DV. According to Swedish law, interpersonal violence is a criminal act [3] and for a child to grow up in a DV situation not only jeopardizes the health and the development of the child, but it is also a crime against the child [4]. According to Swedish law, a child who witnesses DV is a victim of a crime (ibid). Violence, perpetrated on the pregnant woman and directly or indirectly upon the unborn baby, can lead to serious consequences for their health [5–7]. The mothers-to-be’s health and wellbeing also reflects on the offspring’s health in the womb as well as after birth [8]. It is almost 1.5 times more likely to have a preterm baby and/or a low-birth-weight baby when exposed to DV during pregnancy [5].
In a meta-analysis of 55 independent studies, the most robust predictor for DV among pregnant women was a history of violence [9]. Several other risk factors for DV among pregnant women were identified such as; to be single, have a low standard of education as well as a low socioeconomic status and having an unintended pregnancy [9]. Another systematic review and meta-analysis disclosed that high levels of anxiety, symptoms of perinatal depression as well as posttraumatic stress disorder (PTSD) were significantly associated with the experience of DV during a woman’s lifespan, including while being pregnant [10]. A recently published systematic review including 43 selected studies, suggests that women who have experienced lifetime abuse have a significantly increased risk for depression during the pre-natal and postpartum period when compared to women without a history of abuse [11].
The prevalence of violence against pregnant women is lower, 13.3 %, in the developed countries compared to 27.7 % in the less developed countries [9]. The meta-analysis of 92 independent studies involving 23 countries (Sweden included) showed the average prevalence of DV during pregnancy to be 19.8 %. (ibid). However, cultural dissimilarities can make it problematic to compare prevalence rates across different countries as can variances in the methodology and definitions used. In our former studies (the first and the second parts of this project), the prevalence of DV during early pregnancy was shown to be 1 % in early [12] and 2 % in late pregnancy [13]. Another report from six European countries that used a considerable wider definition for the duration of experienced violence among pregnant women showed a prevalence in Sweden of 3.0 % which was the same as in Belgium and in Iceland, whereas in Denmark it was 3.3 %, in Norway 3.7 % and in Estonia 6.5 % [14]. However, the data is not truly comparable as the time point for the recruitment to the studies differs as well as the contexts. The duration for the experienced abuse was defined in a much wider way or included any experienced abuse over the last 12 months and further the perpetrator was not defined. A British longitudinal study reported the prevalence of physical DV to be 1 % during pregnancy compared to 3 % three years postpartum [15]. However, experience of any form of violence was reported to higher extent or 5.1 % (ibid). The postpartum period is not a violence free period for women [15–18]. In a national Swedish survey undertaken for more than a decade ago (based on one single question), focused on mothers with infants up to 1 year old, at least two percent of mothers were physically abused by their intimate partner [18]. International figures for the prevalence of IPV in the postpartum period from developed countries reported lower or much higher figures than those of Sweden; in a national sample of Canadian women, the figure of any abuse was 1 %, responded during 5 to 14 months postpartum [19]. A study from 16 U.S. cities found that physical IPV (solely) was experienced by 3.1 %, emotional abuse by 27 % and coercion-control behaviour by 41.0 % during a 12 month period postpartum [20]. Among Australian women 17 % experienced, physical and/or emotional, abuse by IPV during the first year postpartum [21].
Pregnancy obviously offers no protection against DV, and therefore can only be viewed as a continuum of already existing violence [12, 22], either decreasing [12, 15], or increasing [6, 23] or beginning during pregnancy [24, 25]. Nevertheless, DV is a significant threat against the health of the pregnant woman and her unborn child [5, 10, 26–29]. If violence already exists within the family, it can equally increase [15] as decrease [19, 30] after delivery.
There are no earlier published national population-based longitudinal cohort studies conducted among pregnant and newly delivered women that reveal both the prevalence and incidence of DV, as well as possible risk factors for DV during pregnancy and up to 1–1.5 years postpartum.
The aim of this study was to explore prevalence and incidence of domestic violence during pregnancy and 1 to 1.5 years postpartum as well as to explore the history of violence among new mothers in the southwestern region of Sweden. In addition, the aim was to explore the association between domestic violence postpartum and possible risk factors.
Methods
Design and setting
The present cohort study has a longitudinal design and represents the third report in the project entitled “Pregnant women and new mother’s health and life experience”. The data collection was performed in the southwest area of Sweden. The recruitment as well as the setting and the study participants are described in detail elsewhere [12]. The catchment area is characterized by multicultural diversity and the population includes registered women at an ANC from both a University City and an industrial city as well as the smaller surrounding municipalities.
The characteristics of participants
The inclusion criteria were women ≥ 18 years of age, registered at Antenatal Care (ANC) when pregnant and who could understand and write Swedish or English. Nearly 80 % of the participants had Sweden as their country of origin and the remaining women were born in 93 different other countries [12].
The process of recruitment
Power calculations showed that at least 2000 participants were needed for statistical calculations in order to achieve with 98 % certainty at least 2.5 % prevalence of DV.
Between March 2012 and September 2013 both primipara and multipara women were recruited while in early pregnancy, i.e. gestational week 13 (mean 12.8 weeks, SD 5.11) and were requested to answer Questionnaire I (Q-I) in a private place at the ANC (N = 1939). The second Questionnaire II (Q-II) was completed during late pregnancy at gestation week 34 (mean 33.9 weeks, SD 2.2). The response rate for Q-II was 78.8 % (N = 1527). As a final point, 732 mothers who visited 65 different Child-Welfare-Centers (CWC) with their child/children when they were 1 years old completed the third and the last Questionnaire III (Q-III) at the end of April 2015. One dataset was incomplete which resulted in a total of 731 completed answers of Q-III. Q-III was also completed in a private place (the facilities for privacy varied). If the Child-Welfare nurse missed the opportunity to hand over the Q-III at the 1st year’s routine visit, or if only the father/partner was present, the opportunity was given for the mother to hand over the questionnaire at the next visit, normally at 18 months after the child was born (Fig. 1). If the mother came alone with the child or the intimate partner (irrespective of gender) accompanied the mother to the CWC, the Child-Welfare nurse was permitted to hand over the Q-III to the woman in order for her to complete it at the CWC before going home. According to the WHO ethical and safety recommendations for research on DV against women, it would be strictly forbidden to complete the Q-III at home [31].
Fig. 1.
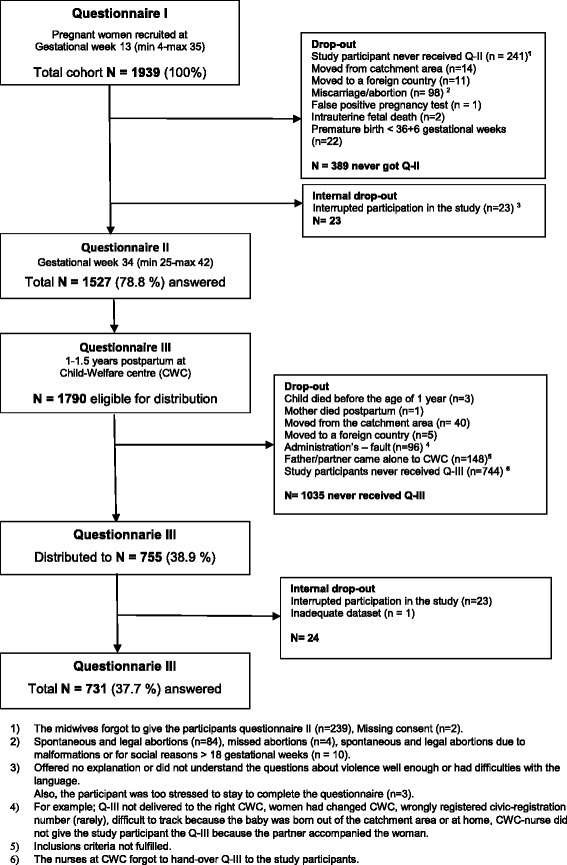
Flowchart over distributed and received answers in Questionnaires I-III
Questionnaires
All the self-reported questionnaires (Q-I, Q-II and Q-III) were completed in as private a place as possible at the ANC’s and CWC’s. Once the participants had completed Q-I, they were familiar with the questions related to any experience of domestic violence. The number of questions were reduced from 122 in Q-I to 93 in Q-II and then increased to 96 in the Q-III. Background questions and the Sense of Coherence scale (SOC-13) [32] were excluded in Q-II and Q-III and questions about breast-feeding were added to Q-III (questions about breastfeeding are not analyzed in the current study). The main instrument the NorVold Abuse Questionnaire (NorAQ) was used, this questionnaire has shown good reliability, validity and specificity regarding the abuse variables [33] and is thoroughly described in our previous study [12]. Questions about all types of violence; psychological, physical and sexual abuse are included in the study as well as the severity of the violence. One additional question, modified [16] from the Abuse Assessment Screen (AAS) [34] was used to investigate current abuse during pregnancy; Have you been exposed to abuse during current pregnancy? In order to investigate any emotional, physical and sexual abuse (yes/no, if yes by whom) was added to the questionnaires (ibid). The Edinburgh Postnatal Depression Scale (EPDS) [35], also used during pregnancy (EDS) [36] as well as the Alcohol Use Disorders Identification Test (AUDIT) [37] were added to the questionnaires and described in detail elsewhere [12].
Definitions
According to Swahnberg et al’s [33] definitions for severity of abuse, which classifies abuse as mild, moderate or severe and the type of abuse was used in the current study. A history of violence is defined as a lifetime experience of emotional, physical or sexual abuse occurring during childhood (<18 years), adulthood (≥18 years) or both, regardless of the level of abuse or the perpetrator’s identity, in accordance with the operationalization of the questions in the NorAQ (ibid).
Classification of the variables
In this study we have used the Same classification of variables as used in our earlier study [12] which were; Age, classified and dichotomized as 18–34 and ≥ 35 years, Language, as a foreign language spoken at home or Swedish (solely), Educational status, as a low educational status, i.e. basic education versus a high educational status such as high school or university. Cohabiting status was classified as being single/living apart, or as a common law spouse/married. Employment status was dichotomized as being employed (including parental leave and studying) or unemployed (including long-term illness). Financial distress was dichotomized as “no” (no problem) or “yes” (serious financial distress). Maternal characteristics concerning body mass index (BMI) were calculated from maternal weight postpartum and height and classified according to WHO’s definition [38] as underweight (<18.5), normal weight (18.50–24.99), overweight (≥25–29.99), and obese (≥30) and dichotomized as under-/normal weight or overweight/obese. Smoking/using wet tobacco was dichotomized as “yes” versus “no”, “yes” (if the woman was a daily smoker or wet-tobacco user at some point during pregnancy) and “no” (never smoked/ or used wet-tobacco or stopped before pregnancy). Alcohol consumption was dichotomized as “yes” (at least once a month) or “no”. Unintended pregnancy was dichotomized as “yes” or “no”. Abortion/miscarriage was classified and dichotomized to “no” or both “miscarriage/abortion”. Self-reported health was dichotomized as poor health versus rather good health. Sleep, was dichotomized as lack of sleep (during the last year, to such an extent that they had problems coping with their daily life), versus adequate sleep.
Statistical methods
Descriptive statistics were utilized to show the prevalence and severity of a lifetime experience of any type and level of abuse. Cochran’s Q-test was used to determine whether the proportion of participants who had reported history of abuse were statistically significant between answers received at the three time points at Q-I to Q-III. OR and 95 % CI were calculated for the crude associations between possible risk factors and ‘DV postpartum’, with ‘DV postpartum’ as a dependent variable for bivariate logistic regression. For the purpose of bivariate logistic regression, a variable for depression was computed based on EPDS scores, i.e. symptoms of depression postpartum, whereby an optimal cut-off of ≥ 13 was chosen as representing the presence of symptoms of depression [36]. The EPDS score was computed only for those responding to all ten questions (missing = 66). In order to analyze the association between the SOC score and exposure to ‘DV postpartum’, the SOC-scale was dichotomized utilizing the first quartile of the distribution as a cut-off value (SOC ≤ 64 and SOC >64) [39]. The SOC score was only computed for those responding to all thirteen items (missing = 47). Multiple logistic regression was performed in order to evaluate the influence of variables that were significant in the bivariate logistic regression except for “Lack of sleep and Age” with ‘DV postpartum’ as a dependent variable; the multiple logistic regression analyses were thus step-wise adjusted (forward selection) for; Single/living apart, EPDS ≥ 13, Low SOC-score, as well as Lack of sleep (not significant), and Age (not significant). Statistical significance was accepted at p < 0.05. Statistical analyses were performed using the Statistical Package for Social Sciences (SPSS) version 22.0 for Windows.
Results
The response rate for those women who actually received the Q-III (n = 755) at the CWC was almost 97 %. Internal dropout was 23 women who interrupted their participation in the study postpartum and one dataset was incomplete. Of the total cohort (n = 1939) of women who were recruited in early pregnancy and who answered Q-III there were 1790 women eligible to get Q-III, but 41.6 % (n = 744), never received the Q-III due to the nurses at the CWC forgetting to give the questionnaire to the participants (Fig. 1). Drop-out analyses showed that those who did not complete the study and did not answer the third and last questionnaire Q-III had a statistically significant higher education and were to a lesser extent unemployed (Table 1).
Table 1.
Dropout figures and women who remained throughout the study and answered Q-III (N = 1939)
| Characteristics | Total n (%) 1939 (100) | Drop-out n (%) 1208 (62.3) | Answereda Q-III n (%) 731 (731.7) | P-value χ2 |
|---|---|---|---|---|
| Age | ||||
| 18–25 | 342 (17.9) | 201(16.8) | 141 (19.6) | NS |
| 26–34 | 1218 (63.7) | 781 (65.4) | 437 (60.8) | |
| ≥ 35 | 353 (18.5) | 212 (17.8) | 141 (19.6) | |
| Parity | ||||
| Primiparae | 819 (45.8) | 518 (46.6) | 301 (44.5) | NS |
| Multiparae | 969 (54.2) | 518 (46.6) | 376 (55.5) | |
| Country of origin | ||||
| Sweden | 1549 (80.1) | 967 (80.2) | 582 (79.8) | NS |
| Nordic countries | 47 (2.4) | 33 (2.7) | 14 (1.9) | |
| Other countries | 338 (17.5) | 205 (17.0) | 133 (18.2) | |
| Cohabiting status | ||||
| Common law spouse/married | 1794 (92.5) | 1108 (94.6) | 662 (93.6) | NS |
| Single/Living apart | 99 (5.1) | 63 (5.4) | 45 (6.4) | |
| Educational status | ||||
| ≤ High school | 642 (33.2) | 369 (30.6) | 273 (37.4) | 0.002 |
| University | 1293 (66.8) | 837 (69.4) | 456 (62.6) | |
| Employment status | ||||
| Employed | 1827 (94.4) | 1150 (95.2) | 677 (93.0) | 0.042 |
| Unemployed | 109 (5.6) | 58 (4.8) | 51 (7.0) | |
| Smoking/Snuffing | ||||
| No | 1523 (78.5) | 957 (81.9) | 566 (79.7) | NS |
| Yes | 355 (18.3) | 211 (18.1) | 144 (20.3) | |
| Use of alcohol | ||||
| No | 776 (40.0) | 538 (46.4) | 345 (48.7) | NS |
| Yes | 1102 (56.8) | 622 (53.6) | 364 (51.3) | |
| Unintended pregnancy | ||||
| No | 1576 (82.4) | 980 (82.1) | 596 (82.9) | NS |
| Yes | 336 (17.6) | 213 (17.9) | 123 817.1) | |
| Abortion/miscarriage | ||||
| No | 1760 (93.5) | 1101 (93.7) | 659 (93.1) | NS |
| Yes | 123 (6.5) | 74 (6.3) | 49 (6.9) | |
Statistical significance accepted at p < 0.05, two-tailed
aWomen’s status in early pregnancy (Q-I). Missing answers are between 3–151
Table 2 provides a summary of the type and severity of lifetime abuse. History of violence was reported by 33.5 % (n = 241) 1 to 1.5 years postpartum. Self-reported experience of any abuse during the past year was 4.2 % (n = 31). A Cochran’s Q test determined that there was a statistically significant difference in the proportion of women who reported lifetime experience of abuse over time, p < 0.0005. Also there was a statistically significant difference in the proportion of women who reported lifetime physical abuse over time, p < 0.0005. There were no statistically significant differences in the proportion of women who reported lifetime experience of emotional and sexual abuse.
Table 2.
Type and severity of history of violence: in Questionnaire I-III
| Type and severity of abuse | Questionnaire I Early pregnancy | Questionnaire II Late pregnancy | Questionnaire III 1.5 year pp | |
|---|---|---|---|---|
| Missing | n (%) | n (%) | n (%) | |
| 1928 (100) 11a | 1497 (100) 30a | 720 (100) 12a | ||
| Lifetime experience of abuseb | 761 (39.5) | 562 (36.8) | 241 (33.5) | |
| Any abuse during the past year | 84 (4.3) | 38 (2.5) | 31 (4.2) | |
| Lifetime of emotional abuse | 374 (19.5) | 257 (16.8) | 113 (16.0) | |
| Mild | 307 (16.1) | 221 (14.5) | 100 (14,1) | |
| Moderate | 187 (9.8) | 123 (8.1) | 63 (8.9) | |
| Severe | 203 (10.6) | 135 (8.8) | 67 (9.4) | |
| Any emotional abuse during the past year | 61 (3.1) | 28 (1.8) | 23 (3.1) | |
| Lifetime of physical abuse | 561 (29.3) | 417 (27.3) | 177 (24.8) | |
| Mild | 529 (28.0) | 399 (26.1) | 170 (24.3) | |
| Moderate | 203 (10.7) | 171 (11.2) | 78 (11.0) | |
| Severe | 127 (6.7) | 89 (5.8) | 49 (7.0) | |
| Any physical abuse during the past year | 36 (1.9) | 13 (0.9) | 10 (5.3) | |
| Lifetime of sexual abuse | 302 (15.7) | 218 (14.3) | 99 (14.0) | |
| Mild c | 49 (2.6) | 37 (2.4) | 22 (3.2) | |
| Mild d | 208 (11.0) | 169 (11.1) | 71 (9.7) | |
| Moderate | 212 (10.9) | 166 (10.9) | 73 (10.0) | |
| Severe | 144 (7.4) | 94 (6.2) | 38 (5.4) | |
| Any sexual abuse during past year | 2 (0.1) | 5 (0.3) | 3 (2.8) |
aNot answered the questions about violence
bAny type of self-reported abuse during lifetime irrespective perpetrator
cEmotional or sexual humiliation
dNo genital contact
Prevalence and incidence of DV during pregnancy up to 1–1.5 years postpartum
When all three questionnaires (Q-I to Q-III) were answered, the prevalence of DV during pregnancy (solely) irrespective of type or severity was reported by 2.5 % of the participants (n = 40). One to 1.5 years postpartum the prevalence of DV, in the whole cohort, had increased to 3.3 % (n = 23), but also the cohort had decreased in number since their recruitment in early pregnancy (Table 3). A Cochran’s Q test determined that there was no statistically significant difference of women who reported DV at the three time points for Q-I to Q-III. The incidence of DV during pregnancy between early pregnancy (Q-I) and late pregnancy (Q-II) was 11 cases as well as between late pregnancy (Q-II) and delivery (Q-III). A total of 22 new cases of self-reported DV during pregnancy gave an incidence of 14 new cases per 1000 women. In the postpartum period, up to 1–1.5 years postpartum, there were 12 new cases of reported DV, which gives an incidence of 17.2 new cases per 1000 women postpartum (the incidence rate is exclusively presented in the text).
Table 3.
Prevalence of DV during pregnancy and 1–1.5 year postpartuma (N = 1939)
| Characteristics | Prevalence of DV early pregnancy | Prevalence of DV late pregnancyb | Prevalence of DV during pregnancyc | Prevalence of DV 1.5 years pp |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | |
| In the analysis | 1928 (99.4) | 1467 (75.7) | 1573 (81.1) | 697 (35.9) |
| Missing d | 11 (0.6) | 472 (24.3) | 336 (18.9) | 35 (4.8 ) |
| Emotional abuse | 15 (0.8) | 24 (1.6) | 36 (2.3) | 18 (2.6) |
| Physical abuse | 7 (0.4) | 11 (0.7) | 13 (0.8) | 8 (1.2) |
| Sexual abuse | 2 (0.1) | 2 (0.1) | 2 (0.1) | 2 (0.3) |
| Total of any type of abuse | 18 (1.0) | 29 (2.0) | 40 (2.5) | 23 (3.3) |
aSome women may report more than one type of violence
bSelf-reported at least once in Q-I, Q-II or both questionnaires
cSelf-reported at least once in Q-I, Q-II, Q-III or in all questionnaires
dExcluded in the analysis, because the questions about violence or the whole questionnaire were not answered
Association between possible risk factors and exposure to DV postpartum
The single strongest risk factor for DV reported at 1–1.5 years postpartum was a history of violence whereby all of the women (n = 23) who had revealed exposure to DV postpartum had also reported a history of violence (p < 0.001). Women who were Single/living apart were almost 13 times more likely to report exposure to DV postpartum (p < 0.001). In addition, women having an EPDS-score of ≥ 13 indicating the presence of several symptoms of depression were 6.2 times more likely to be exposed to DV postpartum (p < 0.001). Of those 9.9 % (n = 66) who had high scores on EPDS ≥ 13 postpartum, 62 % (n = 41) had solely reported high scores in Q-III. Finally, women having a low score on the SOC-scale (in early pregnancy), indicating an inability to use their own resources to maintain and improve their health in stressful situations were 5.2 times more likely to be exposed to DV postpartum (p < 0.001) (Table 4).
Table 4.
Association between possible risk factors and DV 1–1.5 years postpartum (N = 731).a
| DV | ||||
|---|---|---|---|---|
| 1–1.5 year postpartum | P-value | |||
| Independent variable | n (%) | n (%) | OR 95 % CIb | (two-tailed) |
| History of violencec | 241 (33.5) | 23 (9.5) | - | <0.001 |
| Age ≥ 35 | 141 (19.6) | 3 (2.1) | 0.6 (0.2–2.1) | NS |
| Multiparae | 376 (55.5) | 11 (2.9) | 0.8 (0.3–1.9) | NS |
| Low educational status | 273 (37.4) | 10 (3.7) | 0.8 (0.3–1.8) | NS |
| Unemployed | 51 (7.0) | 4 (7.8) | 2.9 (1.0–9.0) | NS |
| Foreign language | 183 (25.2) | 9 (4.9) | 2.0 (0.8–4.6) | NS |
| Single/living apart | 36 (4.9) | 8 (22.2) | 12.8 (5.0–32.7) | <0.001 |
| Financial distress | 357 (49.0) | 15 (4.2) | 2.0 (0.8–4.7) | NS |
| Alcohol consumptiond | 481 (66.8) | 13 (2.7) | 0.7 (0.3–1.7) | NS |
| Smoking/using wet tobacco | 142 (19.6) | 5 (3.5) | 1.1 (0.4–3.1) | NS |
| Overweight/obese | 238 (32.6) | 5 (2.1) | 0.5 (0.2–1.4) | NS |
| Unintended pregnancy | 123 (17.1) | 3 (2.4) | 0.7 (0.2–2.5) | NS |
| Miscarriage/abortion | 49 (6.9) | 1 (2.0) | 0.6 (0.1–4.6) | NS |
| Self-reported poor health | 62 (8.8) | 3 (4.8) | 1.8 (0.5–6.2) | NS |
| Lack of sleep | 79 (11.2) | 5 (6.3) | 2.4 (0.9–6.7) | NS |
| EPDS ≥ 13 | 66 (9.9) | 8 (12.1) | 6.2 (2.5–15.6) | <0.001 |
| SOC Low scoree | 190 (27.8) | 15 (7.9) | 5.2 (2.2–12.5) | <0.001 |
aMissing system = 12
bMethod used: bivariate logistic regression showing unadjusted univariable odds ratios and confidence intervals
cAll (n = 23) reported history of violence and therefore OR with 95 % CI not showed
dAt least once a month
eSOC-score measured in early pregnancy
The following variables were checked in a multiple regression analysis; Single/living apart, EPDS ≥ 13, Low SOC-score, Lack of sleep, and Age (excluded from the model). Model 1: The strongest predictor was single/living apart as an independent variable according to the p-value in Table 4 remaining significant (p < 0.001) and had a 12.9 times higher risk of being associated with DV postpartum. Model II: The second strongest predictor was EPDS ≥ 13 (p < 0.03), included in the model and had had a 3.5 times higher risk of being associated with DV postpartum. Model III: The third strongest predictor, Low score SOC (p < 0.03) was added to the model, and had a 3.0 times higher risk of being associated with DV postpartum. In model II and III the effect remains by both EPDS and low SOC-scores. In model IV the variable Lack of sleep was added to the model but remained non-significant (Table 5).
Table 5.
Association between possible risk factors and exposure to DV 1–1.5 years postpartum (N = 23)
| Variables | Model I OR (95 % CI) | Model II OR (95 % CI) | Model III OR (95 % CI) | Model IV OR (95 % CI) |
|---|---|---|---|---|
| Single/living apart a | 12.8 (5.0–32.7) | 12.1 (4.4–33.5) | 12.2 (4.4–34.2) | 12.9 (4.5–37.1) |
| EPDS ≥ 13 b | 4.5 (1.6–12.1) | 3.3 (1.2–9.2) | 3.5 (1.2–10.4) | |
| Low score SOC c | 2.9 (1.1–7.7) | 3.0 (1.1–8.3) | ||
| Lack of sleep d | 0.7 (0.2–2.5) |
aSingle/living apart versus cohabiting (reference category)
bEPDS ≥13, indicating having a risk of depression versus not ≤ 13 (reference category)
cLow score SOC indicating inability to use their own resources to maintain and improve their health in stressful situations versus medium-high score (reference category). Questions answered in early pregnancy
dLack of sleep versus adequate sleep (reference category)
Women separated from their partners during pregnancy or postpartum
Of 731 women who answered both QI and QIII, thirteen had separated from their partner and nine had become a common law spouse/married. Further, of those women who revealed that they were exposed to DV postpartum (n = 23), four of them had separated from their partner postpartum. Additionally, one woman had separated during pregnancy (only presented in the text).
Discussion
This is the first Swedish longitudinal study with the aim to explore both the prevalence and incidence of DV during pregnancy and up to 1–1.5 years postpartum as well as to explore possible risk factors. The prevalence of DV during pregnancy (solely) irrespective of type or severity was revealed by 2.5 % of the participants (reported in gestation weeks: 13, 34 and until directly after delivery). In actual figures this means that statistically at least 225 pregnant women in the catchment area are exposed to DV during pregnancy annually (calculated on 9000 deliveries) and that the prevalence has increased since our last two reports [12, 13]. This indicates that the violence is not only a continuum of violence [12, 22], but increases as the pregnancy advances which is supported by earlier research [6, 23]. However, the figures agree with those of earlier research carried out in northern Europe, such as that 5.1 % of emotional and physical cruelty from a partner during pregnancy was reported from a longitudinal study from England [15]. In Norway, the prevalence of violence during pregnancy was reported to be 5 % [40] and in a cohort of primipara Danish women the prevalence of violence-exposed pregnant women was 2.5 % [24]. According to the present study’s results the prevalence of DV during pregnancy in Sweden is as common as gestational diabetes (In Sweden/Scania prevalence 1.1 and 2.7 % respectively) and almost as common as preeclampsia (In Sweden/Scania prevalence 2.8 and 2.7 respectively) [41]. Awareness of this fact is very important for working midwives in clinical practise as well as other health care providers. Therefore, to identify, support and guide the women exposed to violence to the right authority and thereby prevent any complications that violence can cause to both the woman and the unborn or new-born baby.
The present study also revealed that the prevalence of DV increased from 2.5 % during pregnancy to 3.3 % up to 1–1.5 years postpartum. However, the study cohort had decreased considerably since recruitment in early pregnancy, but the figures are small and there was no statistically significant difference among women who reported DV during pregnancy compared to postpartum. Hypothetically, it is possible that the prevalence of violence has now, 1–1.5 years postpartum, returned to the earlier levels experienced by non-pregnant women before pregnancy. In addition, in the present study there is an indication that the prevalence of DV 1–1.5 years postpartum might be underestimated because 4.2 % of the newly delivered women revealed experience of abuse in the past year. It is a possibility that a lost to follow-up participants might have been abused and therefore the prevalence and the incidence is reported lower. That violence increases during the postpartum period is supported by earlier research from England [15]. An earlier report from Sweden revealed the prevalence of a 2 % exposure to violence at 1 year postpartum [18] as well as a retrospective study with a national sample from Canada revealing decreased prevalence of DV during pregnancy of 1.4 to 1 % postpartum [19]. Cultural differences as well as differences in the methodology used can make it difficult to compare prevalence rates across countries and different contexts. Sweden, is known internationally for its democracy and gender equality [42], which may have an impact on the huge differences in prevalence of violence compared to Australia [21] and U.S. [20]. However, it cannot be the only explanation. For example, when comparing the US with Sweden there are major differences between the two societies, for example the general acceptance of the possession of weapons. Therefore, it is important to undertake research in domestic violence in different contexts, in each different country. Nevertheless, awareness by the personnel at the CWC about the possible existence of DV is crucial for both the mother’s and the child’s health and welfare.
The current study revealed an incident rate of 14 new cases per 1000 women of self-reported DV during pregnancy as well as an incident rate of additional 17.2 new cases per 1000 women up to 1–1.5 years postpartum. In actual figures, this means that at least 126 new cases during pregnancy respectively 155 women postpartum will be exposed to DV annually in the catchment area. In addition, this indicates that the violence-exposed women becomes aware of the violence and admit that they are violence-exposed, dependent on the fact that they are repeatedly asked about violence over time, which is supported by a Cochrane review [43]. If the health-care providers ask sensitive questions early in the pregnancy and repeat them later in pregnancy as well as postpartum, the violence-exposed women may become more aware of their difficult situation and the possible stigma surrounding the subject will decrease, and the victims of violence may ask for support in their difficult situation. It would be helpful if the philosophy of maternity care was women-centered thereby underpinning the one-to one- relationship with the woman as well as the focus on the women’s needs, expectations and aspirations [44].
One of three women who answered Q-III (the last questionnaire) self-reported a lifetime experience of violence. This is supported by a WHO report [45] related to the global prevalence of violence against women. However, in the current study the cohort has decreased over time as well as the reported prevalence of lifetime experience of violence, which was almost 40 % in early pregnancy compared to 36.8 % in late pregnancy and finally 33.5 % postpartum. Nevertheless, it is disturbing to know that three to four out of ten women, the midwives meet in early pregnancy, may have unprocessed experience of abuse, which could influence their health during pregnancy. This should be taken into account when the midwife discloses a history of violence.
Not surprisingly, a history of violence was the single strongest risk factor for DV during pregnancy, which is supported by the literature [9]. Therefore, it is important to ask the pregnant women at their first visit to the ANC about their lifetime experience of violence as a part of the anamnesis. It is almost thirteen times more likely for the woman to be single/living apart if exposed to DV during the postpartum period, which is supported by earlier research [9].
Assuming that the cultural context of Swedish society is internationally recognized as being gender-equal and that the women are generally well educated and independent. As this is the case, some women choose, not to cohabit, or be married despite their being pregnant, for example if their relationship is rather new. However, it is extremely important for health care providers to be aware that single women/living apart should be seen as a risk group for abuse. Already this group is vulnerable, as a single parent to be, and therefore individually prepared support should be offered.
In the current study at least five out of 13 women who had ended their partnership at the time they answered the last questionnaire 1–1.5 years postpartum also had experience of abuse during the study period. Therefore, the DV could have been a reason, for those women, for ending their partnership. Four of the five ended their relationship postpartum. This is in line with our previous results where it was shown that women exposed to violence during pregnancy were not willing to leave the perpetrator of the violence during pregnancy, as they believe that it is best for the baby that they stay in the relationship until postpartum [6]. The result indicating that women who were single/living apart were 13 times at higher risk for abuse than a cohabiting/married women may have several hypothetical explanations.
Still fifteen of 23 women who were exposed to DV postpartum remain in their violent relationship. As earlier research has shown, those women who are living with the perpetrator during their pregnancy are very isolated and lack social support as well as being unwilling to leave the perpetrator during the pregnancy for the sake of the unborn baby that they believe they are protecting [6]. In addition, self-blame and shame are parts of this complex social behavior (ibid). In addition, in the current study, the results revealed that women who had several symptoms of depression were 3.5 times more likely to be exposed to DV postpartum and this association is supported by a systematic review [9]. As well, another systematic review indicates that there is an association between maternal lifetime abuse and depressive symptoms during the perinatal period [11]. Depression during the perinatal period is of special importance due to the negative effects on the mother’s health as well as the risk of a negative health outcome for the child.
Strength and weakness in the study
This is a longitudinally designed study based on prospectively collected data, which allows comparison of pregnant and newly delivered women who are exposed to violence with those who are not throughout the same time-period, which, is considered as a strength to the study as it offers the possibility to explore both the prevalence and incidence of violence. In addition, using validated instruments in the questionnaires [32–35, 37, 46] where the main instrument has been previously used in a multi-country study, [47] and validated within a Swedish population, [33] is also considered to be a strength. However, there were 1790 study participants eligible to complete the last Q-III, but no less than 1035 women never received the questionnaire. The main reason being that the nurses at the CWC’s forgot to hand-over the Q-III to the study participants (n = 744) or it was their partner (n = 148) who took the child to a CWC instead of the mother or both parents (Fig. 1). This may reflect how strained the CW-nurses working situation was and highlights the result of many staff changes due to vacation and sick leave. The cohort was considerably reduced from Q-I to Q-III and Q-III was distributed to a cohort of 755 women or about 39 % of the original cohort. However, of those women who received the Q-III, there were only about 3 % who did not answer it which can be regarded as very good response rate. Due to the cohort being reduced from initially 1939 participants who answered Q-I to 731 participants who answered the Q-III we must allow for the fact that the prevalence and incidence of DV postpartum may be underestimated.
Conclusion
Pregnancy as well as the postpartum period up to 1–1.5 years are no free zones for domestic violence. Domestic violence increases as the pregnancy develops as well as in the postpartum period. A history of violence and being single/living apart are the strongest risk factors for domestic violence during pregnancy as well as postpartum. In addition, having several symptoms of depression has an association to domestic violence both during pregnancy and postpartum. Collaboration between health care providers at Antenatal-care and Child-Welfare Centres is essential. In order to improve maternal and child health there is a real need to address this vulnerable group of women both at the ANCs and at CWCs.
Implications
The health care providers play a crucial role for the survival of mothers and children faced with domestic violence not only to prevent the progression of the violence but also to empower the survivors and give them individually planned support. In the postpartum period up to 1–1.5 years, there is a need for special attention to those women who have a history of violence and are single/living apart, as well as those who show several types of depression symptoms.
Acknowledgements
The authors would like to thank all the midwives who carried out the recruitment as well as all the CWC nurses who made it possible for us to fulfill the study with the last questionnaire. Special thanks go to the midwife Susan Elvén who also helped with the collection of Q-III. Exceptional thanks go to Mathias Grahn for his excellent statistical support.
NorAQ was developed by NorVold, a research network established in 1997 to explore the prevalence of violence against women and its effects on women’s health. The NorVold research network was supported by grants from the Nordic Council of Ministers. Principal investigators are Barbro Wijma, Berit Schei. Coordinator: Katarina Swahnberg. Local investigators are: Denmark: Katrine Sidenius, Malene Hilden, Finland: Erja Halmesmäki, Ulla Pikkarinen, Iceland: Tora Steingrimsdottir, Norway: Berit Schei, Hildegunn Stoum-Hinsverk, Kristin Offerdal, Sweden: Barbro Wijma, Katarina Swahnberg.
Funding
The Swedish Crime victim Compensation and Support authority as well as the General Maternity Hospital Foundation contributed with funding for the research. The Swedish Society for Health Sciences (Vårdalinstitutet) contributed by giving their permission for scanning.
Availability of data and materials
The datasets generated during and/or analysed during the current study are not publicly available due to the fact that we are still working with the dataset but may possibly be available from the corresponding author on reasonable request.
Authors’ contributions
HF and AKD conceived the study. HF and AKD performed the collection of the data and HF performed the analysis, which was discussed with the co-author AKD. Both authors, HF, AKD, participated in the study design, coordinated, and helped to draft the manuscript. Both authors have read and approved the final manuscript.
Author’s information
The first author Hafrún Finnbogadóttir, RN, RM), PhD and working as Senior lecturer and researcher at the Faculty of Health and Society, Department of Care Science, Malmö University, Sweden. Anna-Karin Dykes, RN, RM, PhD occupied as Senior professor at the Department of Health Sciences, Medical Faculty, Lund University, Sweden.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The Current study was accomplished in accordance with the WHO’s ethical and safety recommendations for research on DV against women [31]. The main principals to justify this research were fulfilled according to the World Medical Association Declaration of Helsinki [48]. Furthermore, the participants were informed about the law governing the procedures of the Swedish Data Inspection (PUL). At the time of their recruitment, the participants were fully informed about the content of the study and their informed written consent was obtained before participation. The women were promised confidentiality and informed that it was entirely up to them if they wished to disclose, to their midwife, that they were living in a violent relationship. Those who were in need of support were guaranteed professional help. Completed questionnaires were collected by the first author, were given a unique code number, and were then kept in a locked safety deposit until they were scanned. Approval was obtained from the Regional Ethical Review Board of Southern Sweden (Dnr: 640/2008).
Abbreviations
- AAS
Abuse Assessment Screen
- ANC
Antenatal Care
- AUDIT
Alcohol Use Disorders Identification Test
- BMI
Body mass index
- CI
Confidence intervals
- DV
Domestic violence
- EDS
Edinburgh Depression Scale
- EPDS
Edinburgh Postnatal Depression Scale
- NorAQ
NorVold Abuse Questionnaire
- OR
Odds ratios
- Q-I
Questionnaire I
- Q-II
Questionnaire II
- Q-III
Questionnaire III
- SOC-13
Sense of Coherence Scale-short form
- WHO
World Health Organization
Contributor Information
Hafrún Finnbogadóttir, Email: hafrun.finnbogadottir@mah.se.
Anna-Karin Dykes, Email: anna-karin.dykes@med.lu.se.
References
- 1.World Health Organization; Violence against women. Intimate partner and sexual violence against women. Facta sheet No 239 [http://www.who.int/mediacentre/factsheets/fs239/en/]. Accessed 8 July 2015.
- 2.Krug EG, Dahlberg LL, Mercy J, Zwi AB, Lozano R. World report on violence and Health. 2002. [Google Scholar]
- 3.Svensk författningssamling (SFS) Brottsbalk 1962:700. Lag (2013:367) 4 a §. Swedish: In English: Swedish Statute Book.Penal code 1962:700 Law (2013:367); 2013. p. 4 a §. [Google Scholar]
- 4.Socialstyrelsen (The National Board of Health and Welfare) Socialtjänstlag. 2001. p. 453. [Google Scholar]
- 5.Shah PS, Shah J, Knowledge Synthesis Group on Determinants of Preterm/LBW Births Maternal exposure to domestic violence and pregnancy and birth outcomes: a systematic review and meta-analyses. J Womens Health. 2010;19(11):2017–2031. doi: 10.1089/jwh.2010.2051. [DOI] [PubMed] [Google Scholar]
- 6.Finnbogadottir H, Dykes AK, Wann-Hansson C. Struggling to survive for the sake of the unborn baby: a grounded theory model of exposure to intimate partner violence during pregnancy. BMC Pregnancy Childbirth. 2014;14(1):293. doi: 10.1186/1471-2393-14-293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Finnbogadottir H, Dykes AK. Midwives’ awareness and experiences regarding domestic violence among pregnant women in southern Sweden. Midwifery. 2012;28(2):181–189. doi: 10.1016/j.midw.2010.11.010. [DOI] [PubMed] [Google Scholar]
- 8.Provencal N, Binder EB. The effects of early life stress on the epigenome: From the womb to adulthood and even before. Exp Neurol. 2015;268:10–20. doi: 10.1016/j.expneurol.2014.09.001. [DOI] [PubMed] [Google Scholar]
- 9.James L, Brody D, Hamilton Z. Risk factors for domestic violence during pregnancy: a meta-analytic review. Violence Vict. 2013;28(3):359–380. doi: 10.1891/0886-6708.VV-D-12-00034. [DOI] [PubMed] [Google Scholar]
- 10.Howard LM, Oram S, Galley H, Trevillion K, Feder G. Domestic violence and perinatal mental disorders: a systematic review and meta-analysis. PLoS Med. 2013;10(5):e1001452. doi: 10.1371/journal.pmed.1001452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alvarez-Segura M, Garcia-Esteve L, Torres A, Plaza A, Imaz ML, Hermida-Barros L, San L, Burtchen N. Are women with a history of abuse more vulnerable to perinatal depressive symptoms? A systematic review. Arch Womens Ment Health. 2014;17(5):343–357. doi: 10.1007/s00737-014-0440-9. [DOI] [PubMed] [Google Scholar]
- 12.Finnbogadottir H, Dykes AK, Wann-Hansson C. Prevalence of domestic violence during pregnancy and related risk factors: a cross-sectional study in southern Sweden. BMC Womens Health. 2014;14:63–6874–14–63. doi: 10.1186/1472-6874-14-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Finnbogadóttir H, Dykes AK, Wann-Hansson C. Prevalence and incidence of domestic violence during pregnancy and associated risk factors: a longitudinal cohort study in southern Sweden. BMC Pregnancy and Childbirth. 2016;16:228. doi:10.1186/s12884-016-1017-6. [DOI] [PMC free article] [PubMed]
- 14.Lukasse M, Schroll AM, Ryding EL, Campbell J, Karro H, Kristjansdottir H, Laanpere M, Steingrimsdottir T, Tabor A, Temmerman M, Van Parys AS, Wangel AM, Schei B. Prevalence of emotional, physical and sexual abuse among pregnant women in six European countries. Acta Obstet Gynecol Scand. 2014;93(7):669–677. doi: 10.1111/aogs.12392. [DOI] [PubMed] [Google Scholar]
- 15.Bowen E, Heron J, Waylen A, Wolke D, ALSPAC Study Team Domestic violence risk during and after pregnancy: findings from a British longitudinal study. BJOG. 2005;112(8):1083–1089. doi: 10.1111/j.1471-0528.2005.00653.x. [DOI] [PubMed] [Google Scholar]
- 16.Stenson K, Heimer G, Lundh C, Nordstrom ML, Saarinen H, Wenker A. The prevalence of violence investigated in a pregnant population in Sweden. J Psychosom Obstet Gynaecol. 2001;22(4):189–197. doi: 10.3109/01674820109049973. [DOI] [PubMed] [Google Scholar]
- 17.Hedin LW. Postpartum, also a risk period for domestic violence. Eur J Obstet Gynecol Reprod Biol. 2000;89(1):41–45. doi: 10.1016/S0301-2115(99)00164-5. [DOI] [PubMed] [Google Scholar]
- 18.Radestad I, Rubertsson C, Ebeling M, Hildingsson I. What factors in early pregnancy indicate that the mother will be hit by her partner during the year after childbirth? A nationwide Swedish survey. Birth. 2004;31(2):84–92. doi: 10.1111/j.0730-7659.2004.00285.x. [DOI] [PubMed] [Google Scholar]
- 19.Daoud N, Urquia ML, O’Campo P, Heaman M, Janssen PA, Smylie J, Thiessen K. Prevalence of abuse and violence before, during, and after pregnancy in a national sample of Canadian women. Am J Public Health. 2012;102(10):1893–1901. doi: 10.2105/AJPH.2012.300843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Charles P, Perreira KM. Intimate Partner Violence During Pregnancy and 1- Year Post-Partum. J Fam Violence. 2007;22(7):609–619. doi: 10.1007/s10896-007-9112-0. [DOI] [Google Scholar]
- 21.Gartland D, Hemphill SA, Hegarty K, Brown SJ. Intimate partner violence during pregnancy and the first year postpartum in an Australian pregnancy cohort study. Matern Child Health J. 2011;15(5):570–578. doi: 10.1007/s10995-010-0638-z. [DOI] [PubMed] [Google Scholar]
- 22.World Health Organization (WHO) WHO Multi-country Study on Women’s Health and Domestic Violence against Women. Initial results on prevalence, health outcomes and women’s responses. World Health Organization: Geneva; 2005. [Google Scholar]
- 23.Lau Y. Does pregnancy provide immunity from intimate partner abuse among Hong Kong Chinese women? Soc Sci Med. 2005;61(2):365–377. doi: 10.1016/j.socscimed.2004.12.002. [DOI] [PubMed] [Google Scholar]
- 24.Finnbogadottir H, Dejin-Karlsson E, Dykes AK. A multi-centre cohort study shows no association between experienced violence and labour dystocia in nulliparous women at term. BMC Pregnancy Childbirth. 2011;11:14. doi: 10.1186/1471-2393-11-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Garcia-Moreno C, Jansen H, Ellsberg M, Heise L, Watts C. WHO Multi-Country study on women’s health and domestic violence against women. Geneva: World Health Organization; 2005. [Google Scholar]
- 26.Jasinski JL. Pregnancy and domestic violence: a review of the literature. Trauma Violence Abuse. 2004;5(1):47–64. doi: 10.1177/1524838003259322. [DOI] [PubMed] [Google Scholar]
- 27.Boy A, Salihu HM. Intimate partner violence and birth outcomes: a systematic review. Int J Fertil Womens Med. 2004;49(4):159–164. [PubMed] [Google Scholar]
- 28.Sharps PW, Laughon K, Giangrande SK. Intimate partner violence and the childbearing year: maternal and infant health consequences. Trauma Violence Abuse. 2007;8(2):105–116. doi: 10.1177/1524838007302594. [DOI] [PubMed] [Google Scholar]
- 29.Shoffner DH. We don’t like to think about it: intimate partner violence during pregnancy and postpartum. J Perinat Neonatal Nurs. 2008;22(1):39–48. doi: 10.1097/01.JPN.0000311874.30828.4e. [DOI] [PubMed] [Google Scholar]
- 30.Silva EP, Ludermir AB, Araujo TV, Valongueiro SA. Frequency and pattern of intimate partner violence before, during and after pregnancy. Rev Saude Publica. 2011;45(6):1044–1053. doi: 10.1590/S0034-89102011005000074. [DOI] [PubMed] [Google Scholar]
- 31.World Health Organization: Putting women first . Ethical and safety recommendations for research on domestic violence against women. Switzerland: WHO/FCH/GWH/01.1 Geneva; 2001. [Google Scholar]
- 32.Antonovsky A. The structure and properties of the sense of coherence scale. Soc Sci Med. 1993;36(6):725–733. doi: 10.1016/0277-9536(93)90033-Z. [DOI] [PubMed] [Google Scholar]
- 33.Swahnberg IM, Wijma B. The NorVold Abuse Questionnaire (NorAQ): validation of new measures of emotional, physical, and sexual abuse, and abuse in the health care system among women. Eur J Public Health. 2003;13(4):361–366. doi: 10.1093/eurpub/13.4.361. [DOI] [PubMed] [Google Scholar]
- 34.McFarlane J, Parker B, Soeken K, Bullock L. Abuse Assessment Screen. J Med Assoc. 1992;267:3176–78. doi: 10.1001/jama.1992.03480230068030. [DOI] [PubMed] [Google Scholar]
- 35.Cox JL, Holden JM, Sagovsky R. Detection of Postnatal Depression. Development of the 10-item Edinburgh Postnatal depression Scale. Br J Psychiatry. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- 36.Rubertsson C, Borjesson K, Berglund A, Josefsson A, Sydsjo G. The Swedish validation of Edinburgh Postnatal Depression Scale (EPDS) during pregnancy. Nord J Psychiatry. 2011;65(6):414–418. doi: 10.3109/08039488.2011.590606. [DOI] [PubMed] [Google Scholar]
- 37.Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption--II. Addiction. 1993;88(6):791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- 38.WHO;Global Database on Body Mass Index. BMI classificatons. [http://apps.who.int/bmi/index.jsp?introPage=intro_3.html]. Accessed 22 Oct 2013.
- 39.Ekelin M, Crang Svalenius E, Larsson AK, Nyberg P, Marsal K, Dykes AK. Parental expectations, experiences and reactions, sense of coherence and grade of anxiety related to routine ultrasound examination with normal findings during pregnancy. Prenat Diagn. 2009;29(10):952–959. doi: 10.1002/pd.2324. [DOI] [PubMed] [Google Scholar]
- 40.Sorbo MF, Grimstad H, Bjorngaard JH, Schei B, Lukasse M. Prevalence of sexual, physical and emotional abuse in the Norwegian mother and child cohort study. BMC Public Health. 2013;13:186–2458–13–186. doi: 10.1186/1471-2458-13-186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Socialstyrelsen (The National Board of Health and Welfare). Statistikdatabas för graviditeter, förlossningar och nyfödda. 2013 [http://www.socialstyrelsen.se/statistik/statistikdatabas/graviditeter-forlossningarochnyfodda]. Accessed 26 Nov 2015.
- 42.World Economic Forum: The Global Gender Gap Report 2013. Accessed 20 Jan 2016.
- 43.Taft A, O’Doherty L, Hegarty K, Ramsay J, Davidson L, Feder G. Screening women for intimate partner violence in healthcare settings. Cochrane Database Syst Rev. 2013;4:CD007007. doi: 10.1002/14651858.CD007007.pub2. [DOI] [PubMed] [Google Scholar]
- 44.Fahy K. What is woman-centred care and why does it matter? Women Birth. 2012;25(4):149–151. doi: 10.1016/j.wombi.2012.10.005. [DOI] [PubMed] [Google Scholar]
- 45.WHO . Global and regional estimates of violence against women: prevalence and health effects of intimate partner violence and non-partner sexual violence. 2013. [Google Scholar]
- 46.Wickberg B, Hwang CP. The Edinburgh Postnatal Depression Scale: validation on a Swedish community sample. Acta Psychiatr Scand. 1996;94(3):181–184. doi: 10.1111/j.1600-0447.1996.tb09845.x. [DOI] [PubMed] [Google Scholar]
- 47.Wijma B, Schei B, Swahnberg K, Hilden M, Offerdal K, Pikarinen U, Sidenius K, Steingrimsdottir T, Stoum H, Halmesmaki E, Nordic cross-sectional study Emotional, physical, and sexual abuse in patients visiting gynaecology clinics: a Nordic cross-sectional study. Lancet. 2003;361(9375):2107–2113. doi: 10.1016/S0140-6736(03)13719-1. [DOI] [PubMed] [Google Scholar]
- 48.World Medical Association Declaration of Helsinki. Ethical Principles for Medical Research Involving Human Subjects. [http://www.wma.net/en/30publications/10policies/b3/]. Accessed 30 Oct 2013. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analysed during the current study are not publicly available due to the fact that we are still working with the dataset but may possibly be available from the corresponding author on reasonable request.


